Clinical estimation of GFR US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical estimation of GFR. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical estimation of GFR US Medical PG Question 1: A healthy 30-year-old female has a measured creatinine clearance of 100 mL/min. She has a filtration fraction (FF) of 25%. Serum analysis reveals a creatinine level of 0.9 mg/dL and an elevated hematocrit of 0.6. Which of the following is the best estimate of this patient’s renal blood flow?
- A. 1.2 L/min
- B. 600 mL/min
- C. 800 mL/min
- D. 400 mL/min
- E. 1.0 L/min (Correct Answer)
Clinical estimation of GFR Explanation: ***1.0 L/min***
- The **renal plasma flow (RPF)** can be calculated by dividing the **creatinine clearance (which approximates GFR)** by the **filtration fraction (FF)**: RPF = GFR / FF = 100 mL/min / 0.25 = 400 mL/min.
- To find the **renal blood flow (RBF)**, we use the formula RBF = RPF / (1 - Hematocrit). Given RPF = 400 mL/min and Hematocrit = 0.6, RBF = 400 mL/min / (1 - 0.6) = 400 mL/min / 0.4 = 1000 mL/min, or **1.0 L/min**.
*1.2 L/min*
- This value would result if the hematocrit were lower (e.g., 0.5) or if the GFR or FF were different, leading to an incorrect RPF or RBF calculation.
- It does not align with the provided values when applying the standard physiological formulas relating GFR, FF, RPF, and hematocrit.
*600 mL/min*
- This value might be obtained if the hematocrit was significantly underestimated or if the RPF calculation was incorrect in determining the RBF.
- It arises from using an incorrect formula or misinterpreting the relationship between plasma flow and blood flow.
*800 mL/min*
- This result would occur if the calculation for RPF or the subsequent RBF was erroneous, possibly by using an incorrect denominator in the RBF formula.
- For example, if RPF was incorrectly assumed to be 320 mL/min and divided by 0.4 (1-Hematocrit).
*400 mL/min*
- This value represents the calculated **renal plasma flow (RPF)**, not the **renal blood flow (RBF)**.
- RBF is always higher than RPF because it includes both plasma and cellular components of blood.
Clinical estimation of GFR US Medical PG Question 2: A 39-year-old woman is brought to the emergency department in a semi-unconscious state by her neighbor who saw her lose consciousness. There was no apparent injury on the primary survey. She is not currently taking any medications. She has had loose stools for the past 3 days and a decreased frequency of urination. No further history could be obtained. The vital signs include: blood pressure 94/62 mm Hg, temperature 36.7°C (98.0°F), pulse 105/min, and respiratory rate 10/min. The skin appears dry. Routine basic metabolic panel, urine analysis, urine osmolality, and urine electrolytes are pending. Which of the following lab abnormalities would be expected in this patient?
- A. Serum blood urea nitrogen/creatinine (BUN/Cr) > 20 (Correct Answer)
- B. Urine osmolality < 350 mOsm/kg
- C. Fractional excretion of sodium (FENa) > 2%
- D. Urine Na+ > 40 mEq/L
- E. Serum creatinine < 1 mg/dL
Clinical estimation of GFR Explanation: ***Serum blood urea nitrogen/creatinine (BUN/Cr) > 20***
- The patient presents with classic signs of **hypovolemia**, including hypotension, tachycardia, dry skin, and decreased urine output, likely due to significant fluid loss from diarrheal illness. This state leads to **prerenal azotemia**.
- In prerenal azotemia, the kidneys reabsorb more water and urea to conserve fluid, leading to a disproportionate rise in BUN compared to creatinine, resulting in a **BUN/Cr ratio typically > 20:1**.
*Urine osmolality < 350 mOsm/kg*
- This value indicates the kidney is actively excreting dilute urine, which would be expected in conditions like **diabetes insipidus** or **excessive fluid intake**.
- In response to hypovolemia, the kidneys attempt to conserve water, leading to the excretion of **highly concentrated urine**, with osmolality typically **> 500 mOsm/kg**.
*Fractional excretion of sodium (FENa) > 2%*
- An FENa > 2% suggests **intrinsic renal damage** (acute tubular necrosis) where the kidneys cannot effectively reabsorb sodium.
- In prerenal azotemia, the kidneys are structurally intact and actively conserve sodium to maintain circulating volume, leading to an **FENa < 1%**.
*Urine Na+ > 40 mEq/L*
- A urine sodium concentration above 40 mEq/L is observed in **intrinsic kidney injury** or during **diuretic use**, where sodium reabsorption is impaired.
- With hypovolemia, the kidneys avidly reabsorb sodium, striving to restore volume. This results in a **low urine sodium concentration**, typically **< 20 mEq/L**.
*Serum creatinine < 1 mg/dL*
- While a serum creatinine < 1 mg/dL *could* be normal for some individuals, in the context of significant dehydration and prerenal azotemia, one would expect a **rise in serum creatinine** alongside BUN.
- The patient's condition, characterized by hypovolemia and decreased renal perfusion, leads to **elevated serum creatinine**.
Clinical estimation of GFR US Medical PG Question 3: A laboratory technician processes basic metabolic panels for two patients. Patient A is 18 years old and patient B is 83 years old. Neither patient takes any medications regularly. Serum laboratory studies show:
Patient A Patient B
Na+ (mEq/L) 145 141
K+ (mEq/L) 3.9 4.4
Cl- (mEq/L) 103 109
HCO3- (mEq/L) 22 21
BUN (mg/dL) 18 12
Cr (mg/dL) 0.8 1.2
Glucose (mg/dL) 105 98
Which of the following most likely accounts for the difference in creatinine seen between these two patients?
- A. Volume depletion
- B. Low body mass index
- C. Insulin resistance
- D. Normal aging (Correct Answer)
- E. High serum aldosterone levels
Clinical estimation of GFR Explanation: ***Normal aging***
- **Creatinine** is a byproduct of **muscle metabolism**, and serum levels reflect both production (muscle mass) and clearance (GFR).
- In **elderly individuals**, **GFR progressively declines** with age (approximately 1 mL/min/year after age 30).
- However, **muscle mass also decreases** with aging (sarcopenia), leading to **reduced creatinine production**.
- Patient B's creatinine of 1.2 mg/dL appears only mildly elevated, but this likely **underestimates the true decline in renal function** because decreased muscle mass reduces baseline creatinine production.
- This is why **estimated GFR calculations** (using Cockcroft-Gault or MDRD equations) incorporate age and weight to account for this phenomenon.
*Volume depletion*
- **Volume depletion** typically leads to an increase in both **BUN** and **creatinine**, often with a disproportionately higher **BUN:Cr ratio** (>20:1).
- Patient B's BUN is **lower** (12 mg/dL) than Patient A's (18 mg/dL), with a BUN:Cr ratio of 10:1, which argues **against volume depletion**.
*Low body mass index*
- **Low BMI** generally correlates with lower muscle mass, which would result in a **lower serum creatinine** level, not higher.
- Patient B has a **higher creatinine** compared to Patient A, making low BMI an unlikely explanation for the observed difference.
*Insulin resistance*
- **Insulin resistance** is associated with altered glucose metabolism and can contribute to conditions like diabetes and chronic kidney disease over time.
- However, it does not directly explain the **age-related creatinine differences** between these two patients with normal glucose levels and no evidence of diabetic nephropathy.
*High serum aldosterone levels*
- **High aldosterone levels** primarily affect **sodium and potassium balance** and fluid retention (causing hypokalemia and mild hypernatremia).
- Both patients have **normal electrolytes**, and aldosterone does not directly account for **age-related creatinine differences**.
Clinical estimation of GFR US Medical PG Question 4: A 32-year-old man is brought to the Emergency Department after 3 consecutive days of diarrhea, fatigue and weakness. His stool has been soft and mucoid, with no blood stains. The patient just came back from a volunteer mission in Guatemala, where he remained asymptomatic. His personal medical history is unremarkable. Today his blood pressure is 98/60 mm Hg, pulse is 110/min, respiratory rate is 19/min, and his body temperature is 36.7°C (98.1°F). On physical exam, he has sunken eyes, dry mucosa, mild diffuse abdominal tenderness, and hyperactive bowel sounds. Initial laboratory tests are shown below:
Serum creatinine (SCr) 1.8 mg/dL
Blood urea nitrogen (BUN) 50 mg/dL
Serum sodium 132 mEq/L
Serum potassium 3.5 mEq/L
Serum chloride 102 mEq/L
Which of the following phenomena would you expect in this patient?
- A. Low urine osmolality, high FeNa+, high urine Na+
- B. High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+
- C. Low urine osmolality, high FeNa+, low urine Na+
- D. High urine osmolality, low FeNa+, low urine Na+ (Correct Answer)
- E. Low urine osmolality, low FeNa+, high urine Na+
Clinical estimation of GFR Explanation: ***High urine osmolality, low FeNa+, low urine Na+***
- The patient exhibits signs of **dehydration** (hypotension, tachycardia, sunken eyes, dry mucosa) and **acute kidney injury (AKI)** with elevated BUN and creatinine, particularly a **BUN/creatinine ratio of 27.8** (50/1.8). These findings point to **prerenal AKI** due to hypovolemia from diarrhea.
- In prerenal AKI, the kidneys attempt to conserve water and sodium to restore intravascular volume. This leads to **increased ADH** secretion and **aldosterone**, resulting in **high urine osmolality** (concentrated urine), **low fractional excretion of sodium (FeNa+)** (<1%), and **low urine sodium concentration** (<20 mEq/L).
*Low urine osmolality, high FeNa+, high urine Na+*
- This pattern is typical of **acute tubular necrosis (ATN)**, an intrinsic cause of AKI, where tubular damage impairs the kidney's ability to concentrate urine and reabsorb sodium.
- The context of dehydration and prerenal state makes ATN less likely as the initial primary pathology compared to the body's compensatory mechanisms during hypovolemia.
*High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+*
- This combination is generally contradictory. High urine osmolality suggests water conservation, while high FeNa+ and urine Na+ indicate sodium wasting, which would typically be seen in diuretic use or specific renal tubular disorders, not uncompensated hypovolemia.
- In prerenal AKI, the body actively reabsorbs sodium to expand volume, leading to low rather than high FeNa+ and urine Na+.
*Low urine osmolality, high FeNa+, low urine Na+*
- This combination is inconsistent. High FeNa+ and low urine Na+ do not usually occur together in a state of hypovolemia. If FeNa+ is high, it implies significant sodium excretion, which would typically be accompanied by higher urine Na+.
- Low urine osmolality also suggests impaired concentrating ability, which is not characteristic of the compensatory mechanisms in prerenal AKI.
*Low urine osmolality, low FeNa+, high urine Na+*
- This combination is also contradictory. Low urine osmolality with low FeNa+ and high urine Na+ does not align with typical kidney responses to dehydration or specific AKI etiologies.
- Low FeNa+ and high urine Na+ are conflicting, as low FeNa+ implies sodium conservation, while high urine Na+ indicates sodium excretion.
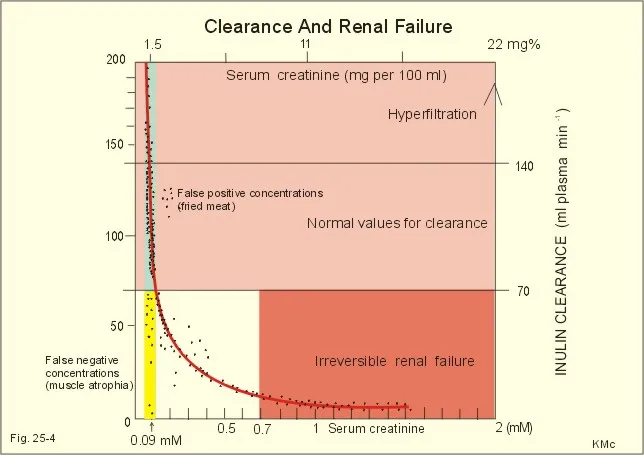
Clinical estimation of GFR US Medical PG Question 5: An investigator is attempting to assess the glomerular filtration rate (GFR) of a healthy adult volunteer. The volunteer's inulin clearance is evaluated under continuous inulin infusion and urine collection and compared to the creatinine clearance. It is found that the estimated GFR based on the volunteer's creatinine clearance is 129 mL/min and the estimated GFR calculated using the inulin clearance is 122 mL/min. Which of the following is the best explanation for the difference in these measurements?
- A. Inulin is actively secreted
- B. Creatinine is not freely filtered
- C. Inulin is not freely filtered
- D. Creatinine is actively secreted (Correct Answer)
- E. Creatinine is passively reabsorbed
Clinical estimation of GFR Explanation: ***Creatinine is actively secreted***
- The higher estimated GFR by **creatinine clearance** (129 mL/min) compared to **inulin clearance** (122 mL/min) indicates that creatinine is not only filtered but also **secreted** by the renal tubules.
- This **active secretion** into the urine leads to a slightly higher amount of creatinine in the final urine than what would be present from filtration alone, thus overestimating the GFR.
*Inulin is actively secreted*
- **Inulin** is considered the **gold standard** for measuring GFR because it is **freely filtered** by the glomerulus, and is neither secreted nor reabsorbed by the renal tubules.
- If inulin were actively secreted, its clearance would be higher than the actual GFR, which is contrary to the observation of a lower inulin clearance compared to creatinine clearance.
*Creatinine is not freely filtered*
- **Creatinine** is largely **freely filtered** by the glomeruli due to its small molecular size and lack of protein binding.
- If creatinine were not freely filtered, its clearance would be lower than the actual GFR, which is contrary to the observed higher creatinine clearance.
*Inulin is not freely filtered*
- **Inulin** is a small polysaccharide that is **freely filtered** by the renal glomeruli without significant impedance.
- Its property of being freely filtered and neither secreted nor reabsorbed is precisely why it serves as the reference standard for GFR measurement.
*Creatinine is passively reabsorbed*
- While some substances are passively reabsorbed, **creatinine** primarily undergoes **filtration and active secretion**, with negligible or no passive reabsorption under normal physiological conditions.
- If creatinine were passively reabsorbed, its clearance would be lower than the actual GFR, leading to an underestimation, which is not what the data shows.
Clinical estimation of GFR US Medical PG Question 6: A researcher is investigating the effects of a new antihypertensive medication on renal physiology. She gives a subject a dose of the new medication, and she then collects plasma and urine samples. She finds the following: Hematocrit: 40%; Serum creatinine: 0.0125 mg/mL; Urine creatinine: 1.25 mg/mL. Urinary output is 1 mL/min. Renal blood flow is 1 L/min. Based on the above information and approximating that the creatinine clearance is equal to the GFR, what answer best approximates filtration fraction in this case?
- A. 10%
- B. 17% (Correct Answer)
- C. 33%
- D. 50%
- E. 25%
Clinical estimation of GFR Explanation: ***17%***
- First, calculate **GFR** using the creatinine clearance formula: GFR = (Urine creatinine × Urinary output) / Serum creatinine = (1.25 mg/mL × 1 mL/min) / 0.0125 mg/mL = **100 mL/min**.
- Next, calculate **Renal Plasma Flow (RPF)** from Renal Blood Flow (RBF) and Hematocrit: RPF = RBF × (1 - Hematocrit) = 1000 mL/min × (1 - 0.40) = **600 mL/min**.
- Finally, calculate **Filtration Fraction (FF)** = GFR / RPF = 100 mL/min / 600 mL/min = 0.1667 = **16.7%, which approximates to 17%**.
- This is the correct answer based on the physiological calculations and represents a normal filtration fraction.
*10%*
- This would correspond to a filtration fraction of 0.10, which would require either a GFR of 60 mL/min (lower than calculated) or an RPF of 1000 mL/min (higher than calculated).
- This value is too low given the provided parameters and doesn't match the calculation from the given data.
*25%*
- This value would suggest FF = 0.25, requiring a GFR of 150 mL/min with the calculated RPF of 600 mL/min.
- This is higher than the calculated GFR of 100 mL/min and doesn't match the given creatinine values.
*33%*
- This would imply FF = 0.33, requiring a GFR of approximately 200 mL/min with RPF of 600 mL/min.
- This is significantly higher than the calculated GFR and would represent an abnormally elevated filtration fraction.
*50%*
- A filtration fraction of 50% is unphysiologically high and would indicate severe pathology.
- This would require a GFR of 300 mL/min with the calculated RPF, which is impossible given the provided creatinine clearance data.
Clinical estimation of GFR US Medical PG Question 7: A 58-year-old Caucasian woman visits her primary care physician for an annual check-up. She has a history of type 2 diabetes mellitus and stage 3A chronic kidney disease. Her estimated glomerular filtration rate has not changed since her last visit. Today, her parathyroid levels are moderately elevated. She lives at home with her husband and 2 children and works as a bank clerk. Her vitals are normal, and her physical examination is unremarkable. Which of the following explains this new finding?
- A. Uremia
- B. Acidemia
- C. Hyperuricemia
- D. Hypercalcemia
- E. Phosphate retention (Correct Answer)
Clinical estimation of GFR Explanation: ***Phosphate retention***
- **Chronic kidney disease** often leads to **phosphate retention** because the damaged kidneys cannot effectively excrete phosphate.
- This elevated phosphate stimulates the parathyroid glands to secrete more **parathyroid hormone (PTH)** as a compensatory mechanism, leading to secondary hyperparathyroidism.
*Uremia*
- While uremia (accumulation of nitrogenous waste products) is a feature of chronic kidney disease, it is not the **direct cause** of elevated parathyroid levels.
- Uremia primarily causes symptoms like fatigue, nausea, and altered mental status, but it doesn't independently trigger PTH release in the same direct manner as phosphate retention or hypocalcemia.
*Acidemia*
- **Metabolic acidosis** is common in chronic kidney disease, but it generally **inhibits** PTH secretion, not stimulates it.
- While it can worsen bone disease, acidemia itself does not explain the primary elevation of parathyroid hormone.
*Hyperuricemia*
- **Hyperuricemia** (elevated uric acid levels) is often associated with chronic kidney disease due to decreased renal excretion of uric acid.
- However, hyperuricemia does not directly cause or explain elevated parathyroid hormone levels.
*Hypercalcemia*
- **Hypercalcemia** would typically **suppress** parathyroid hormone secretion, not elevate it.
- In chronic kidney disease, **hypocalcemia** (due to impaired vitamin D activation and phosphate retention) is more common and would stimulate PTH.
Clinical estimation of GFR US Medical PG Question 8: A 68-year-old woman presents to her primary care physician for a regular check-up. She complains of swelling of her legs and face, which is worse in the morning and decreases during the day. She was diagnosed with type 2 diabetes mellitus a year ago and prescribed metformin, but she has not been compliant with it preferring 'natural remedies' over the medications. She does not have a history of cardiovascular disease or malignancy. Her vital signs are as follows: blood pressure measured on the right hand is 130/85 mm Hg, on the left hand, is 110/80 mm Hg, heart rate is 79/min, respiratory rate is 16/min, and the temperature is 36.6℃ (97.9°F). Physical examination reveals S1 accentuation best heard in the second intercostal space at the right sternal border. Facial and lower limbs edema are evident. The results of the laboratory tests are shown in the table below.
Fasting plasma glucose 164 mg/dL
HbA1c 10.4%
Total cholesterol 243.2 mg/dL
Triglycerides 194.7 mg/dL
Creatinine 1.8 mg/dL
Urea nitrogen 22.4 mg/dL
Ca2+ 9.6 mg/dL
PO42- 3.84 mg/dL
Which of the following statements best describes this patient's condition?
- A. There is an error in Ca2+ measurement because the level of serum calcium is always decreased in the patient’s condition.
- B. If measured in this patient, there would be an increased PTH level. (Correct Answer)
- C. Increase in 1α, 25(OH)2D3 production is likely to contribute to alteration of the patient’s laboratory values.
- D. The calcitriol level is unlikely to be affected in this patient.
- E. Hypoparathyroidism is most likely the cause of the patient’s altered laboratory results.
Clinical estimation of GFR Explanation: ***If measured in this patient, there would be an increased PTH level.***
- This patient presents with signs of **chronic kidney disease (CKD)**, indicated by **elevated creatinine (1.8 mg/dL)** and **urea nitrogen (22.4 mg/dL)**, along with edema.
- In CKD, the kidneys are less able to excrete phosphate and synthesize calcitriol (active vitamin D), leading to **hyperphosphatemia (PO42- 3.84 mg/dL)** and **hypocalcemia**. These imbalances stimulate the parathyroid glands to produce more **parathyroid hormone (PTH)** as a compensatory mechanism, a condition known as **secondary hyperparathyroidism**.
*There is an error in Ca2+ measurement because the level of serum calcium is always decreased in the patient's condition.*
- While **hypocalcemia** is common in CKD, it's not universally present, especially in early or moderate stages.
- The measured **calcium level (9.6 mg/dL)** is within the normal range, suggesting that the compensatory increase in **PTH** might be maintaining **normocalcemia** or that severe hypocalcemia has not yet developed.
*Increase in 1α, 25(OH)2D3 production is likely to contribute to alteration of the patient's laboratory values.*
- In CKD, there is a **decreased production of 1α,25(OH)2D3 (calcitriol)** by the kidneys, not an increase.
- The enzyme **1-alpha-hydroxylase**, responsible for converting 25-hydroxyvitamin D to active calcitriol, becomes deficient as renal function declines.
*The calcitriol level is unlikely to be affected in this patient.*
- The **calcitriol level is significantly affected in CKD**, specifically it is reduced.
- Reduced calcitriol synthesis is a key factor in the development of **secondary hyperparathyroidism** and **renal osteodystrophy**.
*Hypoparathyroidism is most likely the cause of the patient's altered laboratory results.*
- **Hypoparathyroidism** would lead to **low PTH levels**, typically resulting in **hypocalcemia** and **hyperphosphatemia** due to impaired renal phosphate excretion.
- This patient's presentation, particularly the high phosphate and normal calcium (suggesting compensation), is consistent with **hyperparathyroidism secondary to chronic kidney disease**, not hypoparathyroidism.
Clinical estimation of GFR US Medical PG Question 9: A 9-year-old boy is brought to the physician's office by his mother because of facial swelling for the past 2 days. The mother says that her son has always been healthy and active but is becoming increasingly lethargic and now has a puffy face. Upon inquiry, the boy describes a foamy appearance of his urine, but denies having blood in the urine, urinary frequency at night, or pain during urination. He has no history of renal or urinary diseases. Physical examination is unremarkable, except for generalized swelling of the face and pitting edema on the lower limbs. Dipstick analysis reveals 4+ proteinuria. An abdominal ultrasound shows normal kidney size and morphology. A renal biopsy yields no findings under light and fluorescence microscopy; however, glomerular podocyte foot effacement is noted on electron microscopy. Which of the following changes in Starling forces occurs in this patient's condition?
- A. Decreased oncotic pressure in the Bowman's capsule
- B. Increased hydrostatic pressure in the Bowman's capsule
- C. Decreased hydrostatic pressure in the Bowman's capsule
- D. Decreased glomerular oncotic pressure (Correct Answer)
- E. Increased glomerular hydrostatic pressure
Clinical estimation of GFR Explanation: ***Decreased glomerular oncotic pressure***
- The patient presents with **nephrotic syndrome**, characterized by severe proteinuria (4+ on dipstick), edema, and **minimal change disease** (podocyte foot effacement on electron microscopy without changes on light or fluorescence microscopy).
- In nephrotic syndrome, large amounts of plasma proteins, particularly **albumin**, are lost in the urine, leading to **hypoalbuminemia** and a significant decrease in the **oncotic pressure of the plasma** (and thus the glomerular capillaries).
*Decreased oncotic pressure in the Bowman's capsule*
- The Bowman's capsule normally has a **very low oncotic pressure** due to the almost complete absence of proteins in the filtrate.
- While theoretically a massive increase in protein filtration could increase it, the primary Starling force affected by protein loss in nephrotic syndrome is the **plasma oncotic pressure**.
*Increased hydrostatic pressure in the Bowman's capsule*
- This condition is not typically associated with nephrotic syndrome and would rather **impair filtration**.
- Increased hydrostatic pressure in the Bowman's capsule is usually seen in conditions causing **urinary tract obstruction**, which is not present here.
*Decreased hydrostatic pressure in the Bowman's capsule*
- This would tend to **increase glomerular filtration rate** by favoring filtration, which is not the primary physiological change driving edema in nephrotic syndrome.
- There is no clinical indication for such a change in this patient's presentation.
*Increased glomerular hydrostatic pressure*
- While sometimes seen in specific glomerular diseases, this is not the primary or defining Starling force change in nephrotic syndrome leading to systemic edema.
- Increased glomerular hydrostatic pressure would tend to **increase filtration**, potentially worsening proteinuria, but the fundamental issue in nephrotic syndrome is the **loss of oncotic pressure due to protein leakage**.
Clinical estimation of GFR US Medical PG Question 10: A 70-year-old female with chronic kidney failure secondary to diabetes asks her nephrologist to educate her about the techniques used to evaluate the degree of kidney failure progression. She learns about the concept of glomerular filtration rate (GFR) and learns that it can be estimated by measuring the levels of some substances. The clearance of which of the following substances is the most accurate estimate for GFR?
- A. Paraaminohippurate (PAH)
- B. Sodium
- C. Inulin (Correct Answer)
- D. Creatinine
- E. Glucose
Clinical estimation of GFR Explanation: ***Inulin***
- **Inulin** is freely filtered by the glomeruli and is neither reabsorbed nor secreted by the renal tubules, making its clearance the **gold standard** for accurately measuring GFR.
- Due to its ideal physiological properties, inulin clearance perfectly reflects the rate at which plasma is filtered by the kidneys.
*Paraaminohippurate (PAH)*
- **PAH** is almost completely cleared from the blood by both glomerular filtration and **tubular secretion**, making its clearance an accurate measure of **renal plasma flow (RPF)**, not GFR.
- While important for assessing renal blood flow, it does not directly reflect the filtration capacity of the glomeruli.
*Sodium*
- **Sodium** is freely filtered at the glomerulus, but a significant portion (approximately **99%**) is **reabsorbed** by the renal tubules.
- Its clearance is highly variable and depends on various physiological factors, making it unsuitable for GFR estimation.
*Creatinine*
- **Creatinine** is freely filtered by the glomeruli and is also **modestly secreted** by the renal tubules, leading to an **overestimation of GFR** at lower kidney function levels.
- Despite being the most commonly used clinical marker due to its endogenous production, its tubular secretion makes it less accurate than inulin.
*Glucose*
- **Glucose** is freely filtered by the glomeruli but is almost **completely reabsorbed** by the renal tubules under normal physiological conditions.
- Its presence in urine (glycosuria) indicates a high plasma glucose level or tubular reabsorption defects, not a measure of GFR.
More Clinical estimation of GFR US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.