Protein digestion and absorption US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Protein digestion and absorption. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Protein digestion and absorption US Medical PG Question 1: A 4-year-old boy is brought to the physician because of frequent respiratory tract infections and chronic diarrhea. His stools are bulky and greasy, and he has around 8 bowel movements daily. He is at the 10th percentile for height and 25th percentile for weight. Chest examination shows intercostal retractions along with diffuse wheezing and expiratory rhonchi. Which of the following is the most likely cause of his condition?
- A. Increased frequency of trinucleotide repeats
- B. Altered configuration of a protease inhibitor
- C. Intracellular retention of misfolded proteins (Correct Answer)
- D. Defective ciliary protein function
- E. Frameshift mutation of muscle-anchoring proteins
Protein digestion and absorption Explanation: ***Intracellular retention of misfolded proteins***
- The combination of **recurrent respiratory infections**, **chronic diarrhea with greasy stools**, and **failure to thrive (low height/weight percentiles)** in a young child strongly suggests **cystic fibrosis (CF)**.
- CF is caused by mutations in the **CFTR gene**, leading to the production of a **misfolded CFTR protein** that is retained in the endoplasmic reticulum and subsequently degraded, preventing it from reaching the cell membrane. This results in defective chloride transport.
*Increased frequency of trinucleotide repeats*
- This is characteristic of disorders like **Fragile X syndrome**, **Huntington's disease**, and **Friedreich's ataxia**.
- These conditions present with neurological symptoms and intellectual disability, not the respiratory and gastrointestinal manifestations seen in this patient.
*Altered configuration of a protease inhibitor*
- This describes **alpha-1 antitrypsin deficiency**, which primarily causes **emphysema** and **liver disease (cirrhosis)**.
- While it can present with respiratory symptoms, chronic greasy stools and failure to thrive are not typical features.
*Defective ciliary protein function*
- This is the underlying cause of **primary ciliary dyskinesia (PCD)**, also known as **Kartagener syndrome** when associated with situs inversus.
- PCD causes recurrent respiratory infections and bronchiole dilatation, but **chronic diarrhea with bulky, greasy stools** and **failure to thrive** are not characteristic.
*Frameshift mutation of muscle-anchoring proteins*
- This type of mutation is associated with various **muscular dystrophies**, such as **Duchenne muscular dystrophy**, affecting muscle function.
- These disorders typically manifest with progressive muscle weakness and do not explain the respiratory and gastrointestinal issues described.
Protein digestion and absorption US Medical PG Question 2: A 3-year-old boy is brought to the physician because he is easily fatigued and has not gained weight. He eats 3 meals and has 3 to 4 bowel movements daily with bulky stools that float. He had recurrent episodes of sinusitis in infancy. He is at the 15th percentile for height and 5th percentile for weight. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. Impaired intestinal amino acid transport
- B. Mucosal damage from excessive gastric acid
- C. Intestinal inflammatory reaction to gluten
- D. Small intestine bacterial overgrowth
- E. Exocrine pancreatic insufficiency (Correct Answer)
Protein digestion and absorption Explanation: **Exocrine pancreatic insufficiency**
- The patient's presentation with **failure to thrive**, **bulky, floating stools** (suggestive of **steatorrhea**), abdominal distension, and recurrent sinusitis points strongly towards **cystic fibrosis**.
- **Cystic fibrosis** is a genetic disorder causing thick, viscous secretions that obstruct exocrine ducts, most notably in the **pancreas** (leading to malabsorption) and respiratory tract (recurrent infections).
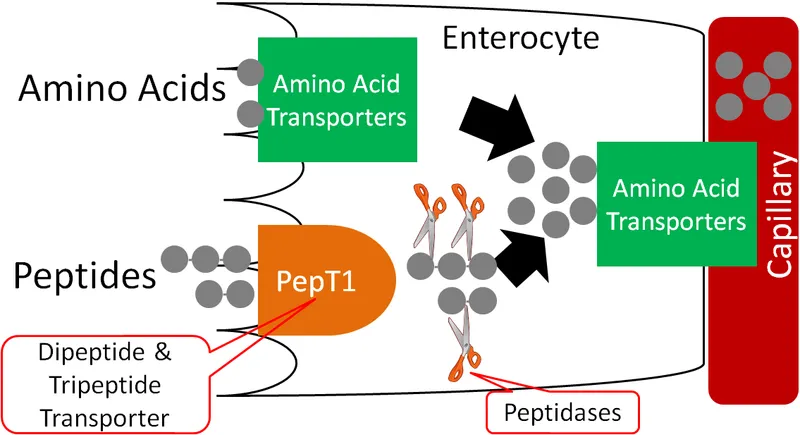
*Impaired intestinal amino acid transport*
- This condition is typically associated with specific genetic disorders like **Hartnup disease** or **cystinuria**, which primarily affect amino acid absorption without the widespread symptoms seen here.
- While it can contribute to nutritional deficiencies, it does not explain the **respiratory symptoms** or the characteristic **fat malabsorption** implied by floating stools.
*Mucosal damage from excessive gastric acid*
- This might suggest conditions like **Zollinger-Ellison syndrome** or severe GERD, which can cause malabsorption due to inactivation of pancreatic enzymes or damage to the small intestine.
- However, it does not account for the **recurrent sinusitis** or the specific type of malabsorption (steatorrhea) typically associated with pancreatic insufficiency.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, abdominal distension, and failure to thrive.
- However, **celiac disease** is not typically associated with **recurrent sinusitis** or the early-onset, severe growth failure and pulmonary issues often seen in cystic fibrosis.
*Small intestine bacterial overgrowth*
- SIBO can cause **malabsorption**, abdominal distension, and failure to thrive, but it does not directly lead to **recurrent sinusitis**.
- While SIBO can be a complication of other malabsorptive conditions, it is not the primary underlying cause suggested by the comprehensive clinical picture, especially the respiratory component.
Protein digestion and absorption US Medical PG Question 3: A scientist is studying the mechanism by which the gastrointestinal system coordinates the process of food digestion. Specifically, she is interested in how distension of the lower esophagus by a bolus of food changes responses in the downstream segments of the digestive system. She observes that there is a resulting relaxation and opening of the lower esophageal (cardiac) sphincter after the introduction of a food bolus. She also observes a simultaneous relaxation of the orad stomach during this time. Which of the following substances is most likely involved in the process being observed here?
- A. Neuropeptide-Y
- B. Secretin
- C. Ghrelin
- D. Vasoactive intestinal polypeptide (Correct Answer)
- E. Motilin
Protein digestion and absorption Explanation: ***Vasoactive intestinal polypeptide***
- **VIP (Vasoactive intestinal polypeptide)** is a neuropeptide that mediates **relaxation** of the **smooth muscle** in the gastrointestinal tract, including the **lower esophageal sphincter** and the **orad stomach**, facilitating the passage of food.
- This relaxation is part of the **receptive relaxation** process, allowing the stomach to accommodate food without a significant increase in intragastric pressure.
*Neuropeptide-Y*
- **Neuropeptide-Y (NPY)** is primarily involved in stimulating **food intake** and **reducing energy expenditure**, acting as an orexigenic peptide.
- It does not directly mediate the relaxation of the **lower esophageal sphincter** or **orad stomach** in response to food bolus distension.
*Secretin*
- **Secretin** is a hormone released in response to **acid in the duodenum** and primarily stimulates the pancreas to release **bicarbonate-rich fluid**.
- Its main role is to neutralize stomach acid, not to mediate sphincter relaxation or stomach accommodation.
*Ghrelin*
- **Ghrelin** is known as the "**hunger hormone**" and primarily stimulates **appetite** and **growth hormone release**.
- It does not play a direct role in the relaxation of the **lower esophageal sphincter** or **orad stomach** during swallowing.
*Motilin*
- **Motilin** promotes **gastric and intestinal motility** during the **interdigestive phase**, responsible for the migrating motor complex (MMC).
- Its actions are generally prokinetic, rather than causing relaxation of the upper GI tract in response to a food bolus.
Protein digestion and absorption US Medical PG Question 4: A 23-year-old man presents to the office complaining of weight loss and fatigue for the past 2 months. He states that he has been experiencing foul-smelling, light-colored stools but thinks it is because he hasn’t been eating well, recently. He has a past medical history significant for cystic fibrosis, which is well-controlled medically. He denies any shortness of breath, chest or abdominal pain, nausea, vomiting, or melena. On physical examination, his skin is pale and dry. Which of the following would be the most likely etiology of a malabsorption syndrome giving rise to this patient’s current condition?
- A. Decreased recycling of bile acids
- B. Pancreatic insufficiency (Correct Answer)
- C. Autoimmune damage to parietal cells
- D. Chronic damage to intestinal mucosa
- E. Damage to intestinal brush border
Protein digestion and absorption Explanation: ***Pancreatic insufficiency***
- Cystic fibrosis typically causes **exocrine pancreatic insufficiency** due to thick secretions blocking the pancreatic ducts, leading to malabsorption of fats and fat-soluble vitamins.
- **Foul-smelling, light-colored stools** (steatorrhea) are a classic symptom of fat malabsorption resulting from inadequate lipase production.
*Decreased recycling of bile acids*
- This typically results in **fat malabsorption**, but it is commonly associated with diseases affecting the **terminal ileum** (e.g., Crohn's disease, resection).
- While it can cause steatorrhea, it is not the primary or most common cause of malabsorption in cystic fibrosis.
*Autoimmune damage to parietal cells*
- This condition leads to **pernicious anemia** due to a lack of intrinsic factor and subsequent **vitamin B12 malabsorption**.
- It does not typically cause **steatorrhea** or generalized fat malabsorption, and it is not directly associated with cystic fibrosis.
*Chronic damage to intestinal mucosa*
- This points towards conditions like **celiac disease** or severe inflammatory bowel disease, which impair nutrient absorption through mucosal injury.
- While cystic fibrosis can have gastrointestinal manifestations, primary mucosal damage is not the leading cause of malabsorption, and the patient's symptoms are more consistent with fat malabsorption.
*Damage to intestinal brush border*
- This is characteristic of conditions like **lactase deficiency** or **celiac disease**, which affect the absorption of specific nutrients (e.g., carbohydrates).
- While it causes malabsorption, the patient's presentation with **steatorrhea** points more specifically to fat malabsorption, which is primarily due to pancreatic enzyme deficiency in cystic fibrosis.
Protein digestion and absorption US Medical PG Question 5: A medical student is studying digestive enzymes at the brush border of the duodenum. He isolates and inactivates an enzyme in the brush border that has a high affinity for the pancreatic proenzyme trypsinogen. When the enzyme is inactivated, trypsinogen is no longer converted to its active form. Which of the following is the most likely underlying mechanism of this enzyme?
- A. Attachment of a carbohydrate to a side chain
- B. Phosphorylation of an amino acid side chain
- C. Carboxylation of a glutamate residue
- D. Cleavage of a propeptide from an N-terminus (Correct Answer)
- E. Conjugation of ubiquitin to lysine residue
Protein digestion and absorption Explanation: ***Cleavage of a propeptide from an N-terminus***
- The enzyme described is **enteropeptidase (also known as enterokinase)**, which is located in the **duodenal brush border**.
- Enteropeptidase's primary function is to activate **trypsinogen** by cleaving a small **N-terminal hexapeptide**, converting it into its active form, **trypsin**.
*Attachment of a carbohydrate to a side chain*
- This process is known as **glycosylation** and can affect protein folding, stability, and recognition, but it's not the primary mechanism by which brush border enzymes like enteropeptidase activate zymogens.
- While some enzymes are glycosylated, inactivation of this mechanism would not halt trypsinogen activation in this specific enzymatic pathway.
*Phosphorylation of an amino acid side chain*
- **Phosphorylation** is a common post-translational modification that regulates enzyme activity by adding a phosphate group, often to serine, threonine, or tyrosine residues.
- While important for many cellular signaling pathways and enzyme regulation, it is not the mechanism by which enteropeptidase activates trypsinogen.
*Carboxylation of a glutamate residue*
- **Carboxylation** typically involves the addition of a carboxyl group, notably important for blood clotting factors (e.g., vitamin K-dependent carboxylation).
- This modification is not involved in the activation of pancreatic proenzymes by brush border enzymes in the duodenum.
*Conjugation of ubiquitin to lysine residue*
- **Ubiquitination** is a process that tags proteins for degradation by the proteasome or can regulate protein function and localization.
- This is a mechanism for protein turnover and regulation, not for the activation of a proenzyme like trypsinogen.
Protein digestion and absorption US Medical PG Question 6: A 55-year-old woman presents with acute onset abdominal pain radiating to her back, nausea, and vomiting. CT scan suggests a diagnosis of acute pancreatitis. The pathogenesis of acute pancreatitis relates to inappropriate activation of trypsinogen to trypsin. Which of the following activates trypsin in normal digestion?
- A. Secretin
- B. Lipase
- C. Cholecystokinin
- D. Enterokinase (Correct Answer)
- E. Amylase
Protein digestion and absorption Explanation: ***Enterokinase***
- **Enterokinase** (also known as enteropeptidase) is a brush border enzyme of the duodenum that specifically cleaves and activates pancreatic **trypsinogen** into its active form, **trypsin**.
- Once activated, **trypsin** then activates other pancreatic proteases (e.g., chymotrypsinogen, procarboxypeptidases, proelastase) within the intestinal lumen.
*Secretin*
- **Secretin** is a hormone released by S cells in the duodenum in response to acidic chyme and acts on the pancreas to stimulate the secretion of **bicarbonate-rich fluid**, which neutralizes gastric acid.
- It does not directly activate digestive enzymes like trypsinogen.
*Lipase*
- **Lipase** is a pancreatic enzyme secreted in its active form that breaks down **dietary fats** (triglycerides) into fatty acids and monoglycerides.
- It plays no role in the activation of trypsinogen.
*Cholecystokinin*
- **Cholecystokinin (CCK)** is a hormone released by I cells in the duodenum in response to fats and proteins, stimulating the contraction of the **gallbladder** and the secretion of **pancreatic enzymes**.
- While it promotes the release of pancreatic enzymes, it does not directly activate trypsinogen.
*Amylase*
- **Amylase** is a pancreatic enzyme secreted in its active form that breaks down **complex carbohydrates** (starches) into simpler sugars (disaccharides and oligosaccharides).
- It is not involved in the activation cascade of pancreatic proteases.
Protein digestion and absorption US Medical PG Question 7: An investigator is studying gastric secretions in human volunteers. Measurements of gastric activity are recorded after electrical stimulation of the vagus nerve. Which of the following sets of changes is most likely to occur after vagus nerve stimulation?
$$$ Somatostatin secretion %%% Gastrin secretion %%% Gastric pH $$$
- A. ↓ ↓ ↓
- B. ↑ ↓ ↑
- C. ↓ ↑ ↓ (Correct Answer)
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Protein digestion and absorption Explanation: ***↓ ↑ ↓***
- Vagal stimulation directly promotes **gastrin release** from G cells, which in turn stimulates **acid secretion**.
- Increased acid secretion **decreases gastric pH** and a lower pH **inhibits somatostatin secretion** in a negative feedback loop.
*↓ ↓ ↓*
- This option incorrectly suggests that vagal stimulation would **decrease gastrin secretion**. Vagal stimulation is a primary stimulant for gastrin release.
- A decrease in gastrin would lead to less acid, resulting in a **higher gastric pH**, not a lower one.
*↑ ↓ ↑*
- This suggests an **increase in somatostatin** and a **decrease in gastrin** which is contrary to the direct effects of vagal stimulation.
- Furthermore, a decreased gastrin would lead to **higher pH**, not lower, unless acid secretion was independently inhibited, which is not the case here.
*↑ ↑ ↑*
- This option correctly indicates an **increase in gastrin secretion** but
incorrectly suggests an **increase in somatostatin** and an **increase in gastric pH**.
- Increased gastrin leads to **increased acid** and thus a **decreased pH**, while high acid levels inhibit somatostatin.
*↑ ↑ ↓*
- This sequence correctly shows an **increase in gastrin** and a **decrease in pH**, but incorrectly suggests an **increase in somatostatin**.
- Somatostatin secretion would be **inhibited** by the increased acid levels resulting from vagal stimulation and gastrin release.
Protein digestion and absorption US Medical PG Question 8: A 4-year-old girl is brought to the physician by her parents because she is severely underweight. She is easily fatigued and has difficulty keeping up with other children at her daycare. She has a good appetite and eats 3 full meals a day. She has 4 to 5 bowel movements daily with bulky, foul-smelling stools that float. She has had recurrent episodes of sinusitis since infancy. Her parents report that she recently started to snore during her sleep. She is at the 15th percentile for height and 3rd percentile for weight. Her vital signs are within normal limits. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. T. whippelii infiltration of intestinal villi
- B. Impaired intestinal amino acid transport
- C. Exocrine pancreatic insufficiency (Correct Answer)
- D. Small intestine bacterial overgrowth
- E. Intestinal inflammatory reaction to gluten
Protein digestion and absorption Explanation: ***Exocrine pancreatic insufficiency***
- The constellation of **failure to thrive**, **bulky, foul-smelling, floating stools** (suggesting **steatorrhea**), recurrent **sinusitis**, and **recurrent respiratory symptoms** (snoring, expiratory crackles) is highly indicative of **cystic fibrosis**, whose primary cause of malabsorption is **exocrine pancreatic insufficiency**.
- **Cystic fibrosis** leads to thick, viscous secretions that obstruct pancreatic ducts, preventing digestive enzymes from reaching the small intestine and causing **malabsorption of fats and fat-soluble vitamins**.
*T. whippelii infiltration of intestinal villi*
- This describes **Whipple's disease**, which typically affects **middle-aged men** and presents with malabsorption, arthralgia, and neurological symptoms.
- It is rare in children and usually presents with symptoms like diarrhea and weight loss, but not commonly with the **recurrent respiratory infections** and **pancreatic insufficiency** seen here.
*Impaired intestinal amino acid transport*
- This typically refers to conditions like **Hartnup disease**, which involves defective transport of neutral amino acids and can lead to **pellagra-like symptoms** (dermatitis, diarrhea, dementia) due to niacin deficiency.
- This condition does not explain the **steatorrhea**, **recurrent sinusitis**, or **respiratory symptoms** found in the patient.
*Small intestine bacterial overgrowth*
- While **SIBO** can cause malabsorption, **abdominal distention**, and loose stools, it does not typically cause **recurrent sinusitis** or the classic **bulky, foul-smelling, floating stools associated with pancreatic insufficiency**.
- SIBO is also not a primary cause of **failure to thrive** in a global sense, but rather a secondary complication.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, **abdominal distention**, **failure to thrive**, and **anemia** (pale conjunctivae).
- However, celiac disease does not typically cause **recurrent sinusitis** or the **respiratory symptoms** (snoring, crackles) that are prominent in this patient's presentation.
Protein digestion and absorption US Medical PG Question 9: A 39-year-old woman presents to her primary care physician because she has been experiencing intermittent abdominal pain for the last 2 weeks. She says that the pain is squeezing in nature, is located in the right upper quadrant, and is particularly severe after eating a meal. After a diagnosis is made, the patient asks why the pain gets worse after eating. The physician explains that food is detected by the gastrointestinal tract through numerous receptors and that this information is transmitted to other parts of the body to cause compensatory changes. The neurons responsible for transmitting this information are most likely located in a layer of the intestine that has which of the following characteristics?
- A. Contracts to generate local movement in mucosa
- B. Contains cells that primarily absorb nutrients
- C. Connective tissue that envelops the other layers
- D. Contracts to generate peristaltic waves (Correct Answer)
- E. Contains large blood vessels and large lymphatic vessels
Protein digestion and absorption Explanation: ***Contracts to generate peristaltic waves***
- This describes the **muscularis propria** (external muscle layer), which contains the **myenteric plexus (Auerbach's plexus)** between its inner circular and outer longitudinal smooth muscle layers.
- The **myenteric plexus is the primary neural network** responsible for detecting food through mechanoreceptors and chemoreceptors, transmitting sensory information, and coordinating both local reflexes and systemic compensatory responses throughout the gastrointestinal tract.
- These neurons communicate with the **autonomic nervous system** and coordinate the release of hormones like **cholecystokinin (CCK)** after eating, which causes gallbladder contraction (relevant to this patient's postprandial pain from cholecystitis).
- While this layer's most obvious function is generating peristalsis, it contains the most extensive enteric nervous system network for sensory integration and motor coordination.
*Contains large blood vessels and large lymphatic vessels*
- This describes the **submucosa**, which contains the **submucosal plexus (Meissner's plexus)**.
- While the submucosal plexus does contain sensory neurons, it primarily regulates **local functions** such as mucosal secretion, absorption, and blood flow rather than the broader systemic compensatory responses described in the question.
- The submucosa's neural network is more limited compared to the myenteric plexus.
*Contracts to generate local movement in mucosa*
- This describes the **muscularis mucosae**, a thin layer of smooth muscle within the mucosa that causes local folding and movement of the mucosal surface.
- This layer lacks significant neural plexuses and is not involved in transmitting sensory information for systemic responses.
*Contains cells that primarily absorb nutrients*
- This refers to the **mucosa**, specifically the epithelial cells lining the intestinal surface.
- While the mucosa contains chemoreceptors and mechanoreceptors, the question asks about the neurons that **transmit** this information, which are located in the deeper neural plexuses (primarily myenteric), not in the absorptive epithelium itself.
*Connective tissue that envelops the other layers*
- This describes the **serosa** (or adventitia), the outermost protective layer.
- The serosa contains minimal neural tissue and is not involved in sensory detection or transmission of gastrointestinal information.
Protein digestion and absorption US Medical PG Question 10: A 65-year-old woman comes to the physician because of progressive weight loss for 3 months. Physical examination shows jaundice and a nontender, palpable gallbladder. A CT scan of the abdomen shows an ill-defined mass in the pancreatic head. She is scheduled for surgery to resect the pancreatic head, distal stomach, duodenum, early jejunum, gallbladder, and common bile duct and anastomose the jejunum to the remaining stomach, pancreas, and bile duct. Following surgery, this patient is at the greatest risk for which of the following?
- A. Wide-based gait
- B. Calcium oxalate kidney stones
- C. Microcytic anemia (Correct Answer)
- D. Increased bile production
- E. Hypercoagulable state
Protein digestion and absorption Explanation: ***Microcytic anemia***
- The surgical procedure described is a **Whipple procedure**, which involves partial gastrectomy and duodenectomy. This significant alteration to the upper GI tract can lead to **iron malabsorption**, as iron is primarily absorbed in the duodenum and proximal jejunum, and gastric acid is crucial for converting dietary iron to its absorbable ferrous form.
- **Iron deficiency** is the most common cause of **microcytic anemia**, characterized by small, pale red blood cells, due to impaired hemoglobin synthesis as a result of insufficient iron availability for the heme component.
*Wide-based gait*
- A **wide-based gait** is typically associated with **ataxia** or conditions affecting cerebellar function or proprioception, which are not direct complications of a Whipple procedure.
- While nutritional deficiencies can occur post-surgery, a wide-based gait specifically points to neurological impairment rather than postsurgical metabolic issues.
*Calcium oxalate kidney stones*
- **Calcium oxalate kidney stones** are often associated with conditions causing **hypercalciuria** or malabsorption of fat, which leads to increased oxalate absorption in the colon. While fat malabsorption can occur after a Whipple due to pancreatic insufficiency, dietary oxalate intake and hydration status are generally more significant determinants of stone formation.
- The surgery itself does not directly increase the risk for calcium oxalate kidney stones more than other listed complications.
*Increased bile production*
- A Whipple procedure involves the removal of the **gallbladder** and rerouting of the **bile duct** directly into the jejunum. This does not lead to increased bile production, but rather a different regulation and flow of bile.
- In fact, the absence of the gallbladder means there is no storage for bile, leading to a continuous, unregulated flow of bile into the small intestine, potentially contributing to maldigestion or diarrhea, but not "increased production."
*Hypercoagulable state*
- While surgery, including a Whipple procedure, can transiently increase the risk of a **hypercoagulable state** (e.g., deep vein thrombosis, pulmonary embolism) in the immediate postoperative period due to immobility and tissue injury, this risk is generally mitigated with prophylactic anticoagulation.
- The question asks about the **greatest risk** post-surgery, and long-term complications related to altered anatomy and malabsorption, such as microcytic anemia, are more direct and sustained consequences unique to the extent of the resection.
More Protein digestion and absorption US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.