Pancreatic exocrine function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pancreatic exocrine function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
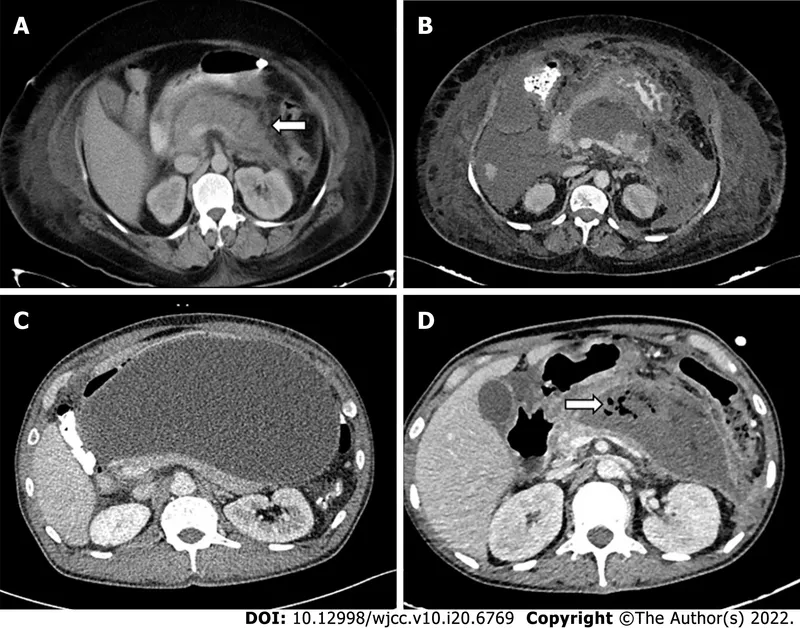
Pancreatic exocrine function US Medical PG Question 1: A 42-year-old woman is brought to the emergency department because of a 5-day history of epigastric pain, fever, nausea, and malaise. Five weeks ago she had acute biliary pancreatitis and was treated with endoscopic retrograde cholangiopancreatography and subsequent cholecystectomy. Her maternal grandfather died of pancreatic cancer. She does not smoke. She drinks 1–2 beers daily. Her temperature is 38.7°C (101.7°F), respirations are 18/min, pulse is 120/min, and blood pressure is 100/70 mm Hg. Abdominal examination shows epigastric tenderness and three well-healed laparoscopy scars. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10 g/dL
Leukocyte count 15,800/mm3
Serum
Na+ 140 mEq/L
Cl− 103 mEq/L
K+ 4.5 mEq/L
HCO3- 25 mEq/L
Urea nitrogen 18 mg/dL
Creatinine 1.0 mg/dL
Alkaline phosphatase 70 U/L
Aspartate aminotransferase (AST, GOT) 22 U/L
Alanine aminotransferase (ALT, GPT) 19 U/L
γ-Glutamyltransferase (GGT) 55 U/L (N = 5–50)
Bilirubin 1 mg/dl
Glucose 105 mg/dL
Amylase 220 U/L
Lipase 365 U/L (N = 14–280)
Abdominal ultrasound shows a complex cystic fluid collection with irregular walls and septations in the pancreas. Which of the following is the most likely diagnosis?
- A. Pancreatic cancer
- B. Acute cholangitis
- C. Pancreatic abscess (Correct Answer)
- D. Pancreatic pseudocyst
- E. ERCP-induced pancreatitis
Pancreatic exocrine function Explanation: ***Pancreatic abscess***
- The presence of fever, leukocytosis (WBC 15,800/mm³), and a complex, septated fluid collection seen on ultrasound, following acute pancreatitis, is highly suggestive of a **pancreatic abscess**.
- **Pancreatic abscesses** develop as a complication of acute pancreatitis, typically resulting from infected pancreatic necrosis and often present with persistent symptoms of infection.
*Pancreatic cancer*
- While there is a family history of pancreatic cancer, her acute presentation with **fever, leukocytosis**, and a tender, complex fluid collection is **not typical** for initial pancreatic cancer presentation.
- Pancreatic cancer typically presents with **jaundice, weight loss**, and chronic abdominal pain rather than acute infectious symptoms and a fluid collection after pancreatitis.
*Acute cholangitis*
- Acute cholangitis is characterized by **Charcot's triad** (fever, jaundice, right upper quadrant pain) or **Reynold's pentad** (Charcot's triad plus altered mental status and hypotension).
- The patient's **normal bilirubin level** (1 mg/dL), absence of jaundice, and epigastric pain (not right upper quadrant specific) make acute cholangitis less likely, especially with a history of cholecystectomy.
*Pancreatic pseudocyst*
- A pancreatic pseudocyst is a **sterile** fluid collection without signs of active infection (e.g., fever, leukocytosis) and typically has well-defined, smooth walls rather than irregular walls or septations.
- While she has a fluid collection from pancreatitis, the **fever, leukocytosis, and irregular/septated walls** on ultrasound point away from a simple pseudocyst and towards an infected collection.
*ERCP-induced pancreatitis*
- ERCP-induced pancreatitis would have occurred **immediately after the procedure**, which was five weeks ago. The current symptoms occurring five weeks later suggest a complication of the initial pancreatitis, not a new induction.
- While ERCP can cause pancreatitis, this diagnosis refers to the initial event, not a **secondary infectious complication** manifesting weeks later.
Pancreatic exocrine function US Medical PG Question 2: A group of investigators is performing a phase I trial of a novel drug among patients with chronic right upper quadrant pain. Iminodiacetic acid labeled with technetium 99m is administered intravenously and subjects are subsequently imaged with a gamma camera. It is found that administration of the experimental drug increases the amount of iminodiacetic acid in the intestines. The effect of this novel drug is most similar to that of a substance secreted by which of the following cells?
- A. Pancreatic D cells
- B. Antral G cells
- C. Jejunal I cells (Correct Answer)
- D. Duodenal S cells
- E. Duodenal K cells
Pancreatic exocrine function Explanation: ***Jejunal I cells***
- The imaging study with **iminodiacetic acid (HIDA)** scan assesses **gallbladder function** and bile flow; increased intestinal HIDA suggests increased bile secretion into the duodenum.
- **I cells** in the jejunum secrete **cholecystokinin (CCK)**, which stimulates gallbladder contraction and the release of bile into the intestines, mimicking the drug's effect.
*Pancreatic D cells*
- **Pancreatic D cells** secrete **somatostatin**, a hormone that generally inhibits digestive processes, including bile secretion and gallbladder contraction.
- This effect is opposite to the experimental drug's action of increasing bile flow into the intestines.
*Antral G cells*
- **Antral G cells** secrete **gastrin**, which primarily stimulates gastric acid secretion by parietal cells and promotes gastric motility.
- Gastrin has a minimal direct effect on bile secretion or gallbladder contraction.
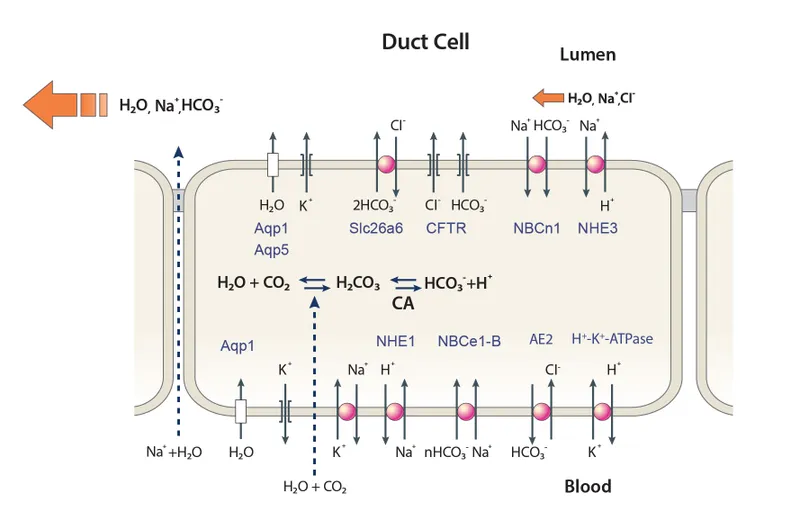
*Duodenal S cells*
- **S cells** in the duodenum secrete **secretin**, which primarily stimulates bicarbonate and water secretion from the pancreas and bile ducts, without a direct effect on gallbladder contraction or bile acid secretion.
- Secretin's main role is to neutralize gastric acid in the duodenum.
*Duodenal K cells*
- **K cells** in the duodenum and jejunum secrete **gastric inhibitory polypeptide (GIP)**, which primarily stimulates insulin release from pancreatic beta cells in response to glucose and inhibits gastric acid secretion.
- GIP does not directly stimulate bile flow or gallbladder contraction.
Pancreatic exocrine function US Medical PG Question 3: Nine healthy subjects participate in a study of gastric secretions. Subjects are asked to eat a meal at hour 0, at which time the pH of stomach contents and rate of stomach acid secretions are measured over the next 4 hours. Results of the study are shown. Which of the following mediators is most active at point A in the graph?
- A. Secretin
- B. Acetylcholine (Correct Answer)
- C. Prostaglandin
- D. Glucose-dependent insulinotropic peptide
- E. Somatostatin
Pancreatic exocrine function Explanation: ***Acetylcholine***
- At point A, the **pH is low** and the **rate of stomach acid secretion is high**, indicating a robust post-meal response for digestion.
- **Acetylcholine** is a primary neurocrine stimulant of gastric acid secretion, acting both directly on parietal cells and indirectly by stimulating histamine release, making it highly active during increased acid output.
*Secretin*
- **Secretin** primarily acts to *inhibit* gastric acid secretion and stimulate bicarbonate and fluid secretion from the pancreas and liver, particularly in response to low pH in the duodenum.
- It would be *less active* during a phase of high gastric acid secretion, as its main role is to neutralize acid after it leaves the stomach.
*Prostaglandin*
- **Prostaglandins (e.g., PGE2)** play a *cytoprotective role* in the stomach, inhibiting acid secretion and increasing mucus and bicarbonate production.
- Their activity would *reduce* the rate of stomach acid secretion, which is contrary to the high secretion rate observed at point A.
*Glucose-dependent insulinotropic peptide*
- **Glucose-dependent insulinotropic peptide (GIP)** primarily stimulates **insulin release** from pancreatic β-cells in response to ingested glucose and fat.
- While it has slight *inhibitory effects* on gastric acid secretion, its main role is metabolic, not directly related to the observed high acid secretion or low pH.
*Somatostatin*
- **Somatostatin** is a potent *inhibitor* of gastric acid secretion, acting directly on parietal cells and indirectly by inhibiting the release of histamine and gastrin.
- Therefore, it would be *less active* during a period of high gastric acid secretion, as its function is to suppress such activity.
Pancreatic exocrine function US Medical PG Question 4: During a study on gastrointestinal hormones, a volunteer is administered the hormone secreted by S cells. Which of the following changes most likely represent the effect of this hormone on gastric and duodenal secretions?
$$$ Gastric H+ %%% Duodenal HCO3- %%% Duodenal Cl- $$$
- A. ↓ ↓ ↓
- B. ↑ ↓ no change
- C. ↑ ↑ ↓
- D. ↓ ↑ ↓ (Correct Answer)
- E. ↓ no change no change
Pancreatic exocrine function Explanation: ***↓ ↑ ↓***
- S cells secrete **secretin**, which primarily inhibits **gastric acid (H+) secretion** to protect the duodenal mucosa from acidic chyme.
- Secretin also stimulates the pancreas and bile ducts to secrete **bicarbonate (HCO3-)**, neutralizing the acidic chyme. Duodenal **chloride (Cl-) secretion is typically reduced** as it is often exchanged for bicarbonate or water follows bicarbonate secretion for osmotic balance.
*↓ ↓ ↓*
- While **gastric H+ decreases** due to secretin, **duodenal HCO3- secretion increases**, not decreases, making this option incorrect.
- **Duodenal Cl- secretion** would likely decrease, but the other components are inconsistent with secretin's effects.
*↑ ↓ no change*
- Secretin **inhibits gastric H+ secretion**, so an increase contradicts its primary function to protect the duodenum from acid.
- **Duodenal HCO3- secretion increases**, not decreases, and no change in Cl- is unlikely given the physiological responses to secretin.
*↑ ↑ ↓*
- Secretin **inhibits gastric H+ secretion**, so an increase is incorrect.
- While **duodenal HCO3- increases** and **Cl- decreases**, the initial change in gastric H+ makes this option wrong.
*↓ no change no change*
- While **gastric H+ is indeed decreased**, secretin significantly **increases duodenal HCO3- secretion** and likely decreases duodenal Cl- secretion, making "no change" in these parameters incorrect.
- Secretin has a pronounced effect on both bicarbonate and chloride transport in the duodenum.
Pancreatic exocrine function US Medical PG Question 5: A 56-year-old woman presents to the emergency department with an episode of nausea and severe unrelenting right upper abdominal pain. She had a cholecystectomy for gallstones a year earlier and has since experienced frequent recurrences of abdominal pain, most often after a meal. Her past medical history is otherwise unremarkable and she only takes medications for her pain when it becomes intolerable. Her physical exam is normal except for an intense abdominal pain upon deep palpation of her right upper quadrant. Her laboratory values are unremarkable with the exception of a mildly elevated alkaline phosphatase, amylase, and lipase. Her abdominal ultrasound shows a slightly enlarged common bile duct at 8 mm in diameter (N = up to 6 mm) and a normal pancreatic duct. The patient is referred to a gastroenterology service for an ERCP (endoscopic retrograde cholangiopancreatography) to stent her common bile duct. During the procedure the sphincter at the entrance to the duct is constricted. Which statement best describes the regulation of the function of the sphincter which is hampering the cannulation of the pancreatic duct in this patient?
- A. The sphincter is contracted between meals.
- B. A hormone released by duodenal cells that stimulates gastrointestinal motility is the most effective cause of relaxation.
- C. Regulation of function of the sphincter of Oddi does not involve neural inputs.
- D. A hormone released by the I cells of the duodenum in the presence of fatty acids is the most effective cause of relaxation. (Correct Answer)
- E. Sphincter relaxation is enhanced via stimulation of opioid receptors.
Pancreatic exocrine function Explanation: ***A hormone released by the I cells of the duodenum in the presence of fatty acids is the most effective cause of relaxation.***
- The **sphincter of Oddi** relaxes primarily in response to **cholecystokinin (CCK)**, which is released by **I cells** in the duodenum when **fatty acids** and amino acids enter the small intestine. This relaxation allows bile and pancreatic enzymes to flow into the duodenum to aid digestion.
- The patient's symptoms of post-cholecystectomy pain and dilated common bile duct suggest **sphincter of Oddi dysfunction**, where the sphincter fails to relax properly, hindering bile flow.
*The sphincter is contracted between meals.*
- While the sphincter of Oddi does maintain a **tonic contraction** between meals to prevent bile reflux and store bile in the gallbladder, this statement doesn't describe the primary mechanism for its **relaxation during digestion**.
- The problem in this patient is the failure of the sphincter to relax, rather than its normal contracted state.
*A hormone released by duodenal cells that stimulates gastrointestinal motility is the most effective cause of relaxation.*
- This likely refers to **motilin**, which is released by enterochromaffin cells (Mo cells) in the duodenum and primarily regulates gastrointestinal motility, particularly the migrating motor complex.
- Motilin does not directly or most effectively cause relaxation of the sphincter of Oddi; **CCK** from I cells is the primary hormonal mechanism.
*Regulation of function of the sphincter of Oddi does not involve neural inputs.*
- The function of the sphincter of Oddi is under **complex neural and hormonal control**.
- Both **parasympathetic (vagal)** and **sympathetic** nervous inputs modulate its activity, often working in conjunction with CCK to coordinate bile and pancreatic juice release.
*Sphincter relaxation is enhanced via stimulation of opioid receptors.*
- **Opioid receptors** in the sphincter of Oddi, when stimulated, can actually cause **contraction** or spasm of the sphincter.
- This is a well-known side effect that can worsen or induce biliary colic, not enhance relaxation.
Pancreatic exocrine function US Medical PG Question 6: A 28-year-old man presents to the emergency department with diffuse abdominal pain and nausea for the past 5 hours. The pain started with a dull ache but is now quite severe. He notes that he “just doesn’t feel like eating” and has not eaten anything for almost a day. Although the nausea is getting worse, the patient has not vomited. He notes no medical issues in the past and is not currently taking any medications. He admits to drinking alcohol (at least 2–3 bottles of beer per day after work and frequent binge-drinking weekends with friends). He says that he does not smoke or use illicit drugs. Vital signs include: pulse rate 120/min, respiratory rate 26/min, and blood pressure 100/70 mm Hg. On examination, the patient’s abdomen is diffusely tender. His breath smells like alcohol, with a fruity tinge to it. Bowel sounds are present. No other findings are noted. Fingerstick glucose is 76mg/dL. After the examination, the patient suddenly and spontaneously vomits. Which of the following is the underlying mechanism of the most likely diagnosis in this patient?
- A. Increased acetyl CoA levels (Correct Answer)
- B. Inadequate insulin production
- C. Increased osmolal gap
- D. Starvation
- E. Thiamine deficiency
Pancreatic exocrine function Explanation: ***Increased acetyl CoA levels***
- This patient presents with **alcoholic ketoacidosis (AKA)**, and the underlying biochemical mechanism is the accumulation of **acetyl CoA** that is shunted into ketone body synthesis.
- In AKA, starvation depletes glycogen stores and **oxaloacetate** (needed for the TCA cycle). Simultaneously, alcohol metabolism increases the **NADH/NAD+ ratio**, which further impairs gluconeogenesis and reduces oxaloacetate availability.
- Enhanced lipolysis (due to low insulin and high counter-regulatory hormones) produces large amounts of fatty acids, which undergo β-oxidation to generate **acetyl CoA**.
- With insufficient oxaloacetate to enter the TCA cycle, acetyl CoA accumulates and is diverted to **ketogenesis** (producing acetoacetate, β-hydroxybutyrate, and acetone).
- The **fruity breath** is from acetone, and the metabolic acidosis causes the patient's symptoms (abdominal pain, nausea, tachycardia, tachypnea).
*Starvation*
- While **starvation** is a critical **precipitating factor** in AKA (it depletes glycogen and triggers lipolysis), it is not the underlying biochemical mechanism itself.
- Starvation creates the metabolic conditions (low insulin, depleted oxaloacetate) that lead to the accumulation of acetyl CoA and subsequent ketogenesis, but the question asks for the mechanism, not the trigger.
*Inadequate insulin production*
- **Inadequate insulin production** is the primary defect in **diabetic ketoacidosis (DKA)**, which is ruled out by this patient's normal blood glucose (76 mg/dL).
- In AKA, insulin levels are typically low (due to starvation), but this is secondary to metabolic stress rather than a primary pancreatic failure. The key mechanism is still the acetyl CoA accumulation and shunting to ketogenesis.
*Increased osmolal gap*
- An **increased osmolal gap** suggests unmeasured osmolytes, typically seen with toxic alcohol ingestions (methanol, ethylene glycol) or severe lactic acidosis.
- While ethanol itself can transiently increase the osmolal gap, this is not the mechanism explaining the ketoacidosis, fruity breath, and clinical presentation in this case.
*Thiamine deficiency*
- **Thiamine deficiency** is common in chronic alcoholics and causes Wernicke-Korsakoff syndrome and other neurological complications.
- Thiamine is a cofactor for pyruvate dehydrogenase and α-ketoglutarate dehydrogenase, but its deficiency does not directly cause the ketoacidosis seen here, which results from altered lipid metabolism and acetyl CoA accumulation.
Pancreatic exocrine function US Medical PG Question 7: A group of scientists is studying the mechanism of action of various pancreatic hormones in rats. The scientists studied hormone A, which is secreted by the β-cells of the pancreas, and found that hormone A binds to a complex dimeric receptor on the cell membrane and exerts its effects via phosphorylation and subsequent downstream signaling that includes dephosphorylation of different intracellular proteins. Now they are studying hormone B, which is secreted by the α-cells and antagonizes the actions of hormone A. Which 2nd messenger system would hormone B utilize to exert its cellular effects?
- A. Direct cytoplasmic receptor binding
- B. Phospholipase C
- C. Tyrosine kinase
- D. Direct nuclear receptor binding
- E. Adenylyl cyclase-cyclic AMP (Correct Answer)
Pancreatic exocrine function Explanation: ***Adenylyl cyclase-cyclic AMP***
- Hormone B is **glucagon**, secreted by pancreatic α-cells, which antagonizes the effects of insulin (hormone A). Glucagon primarily acts through a **G protein-coupled receptor** that activates **adenylyl cyclase**, leading to an increase in intracellular **cyclic AMP (cAMP)**.
- Increased cAMP then activates **protein kinase A (PKA)**, which phosphorylates various intracellular proteins to promote **glycogenolysis** and **gluconeogenesis**, thereby raising blood glucose levels.
*Direct cytoplasmic receptor binding*
- This mechanism is characteristic of **steroid hormones**, which are lipid-soluble and can diffuse across the cell membrane to bind to receptors in the cytoplasm.
- Pancreatic hormones like glucagon are **peptide hormones**, which are water-soluble and typically bind to cell surface receptors.
*Phospholipase C*
- Activation of **phospholipase C (PLC)** leads to the production of **inositol triphosphate (IP3)** and **diacylglycerol (DAG)**, which mobilize intracellular calcium and activate protein kinase C, respectively.
- While some G protein-coupled receptors activate PLC, **glucagon's primary signaling pathway** involves adenylyl cyclase.
*Tyrosine kinase*
- **Tyrosine kinase receptors** are often associated with growth factors and insulin (hormone A) signaling, leading to phosphorylation of tyrosine residues on target proteins.
- Glucagon's receptor is a **G protein-coupled receptor**, not a receptor tyrosine kinase, and its actions are mediated through serine/threonine phosphorylation via PKA.
*Direct nuclear receptor binding*
- This mechanism is typical for **steroid hormones** and **thyroid hormones**, which are lipid-soluble and bind to receptors in the nucleus to directly influence gene transcription.
- As a peptide hormone, glucagon binds to cell surface receptors and does not directly interact with nuclear receptors.
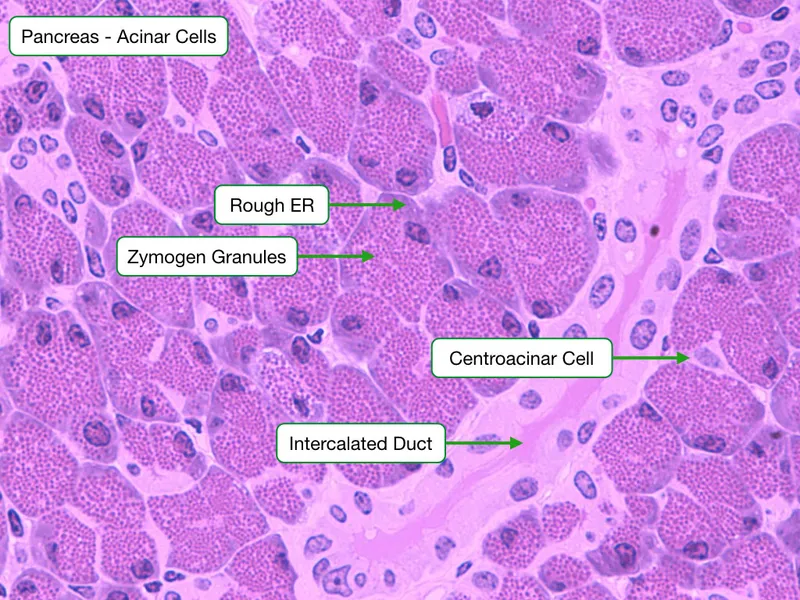
Pancreatic exocrine function US Medical PG Question 8: An 11-year-old boy who recently emigrated from Ukraine is brought to the physician for the evaluation of failure to thrive. Genetic analysis shows the deletion of the 508th codon in a gene on chromosome 7. The deletion results in defective post-translational folding of a protein and retention of the misfolded protein in the rough endoplasmic reticulum. The activity of which of the following channels is most likely to be increased as a result of the defect?
- A. Calcium channels of distal tubular cells
- B. ATP-sensitive potassium channels of pancreatic beta cells
- C. Bicarbonate channels of pancreatic ductal cells
- D. Chloride channels of epithelial cells in sweat glands
- E. Sodium channels of respiratory epithelial cells (Correct Answer)
Pancreatic exocrine function Explanation: ***Sodium channels of respiratory epithelial cells***
- The patient's presentation with **failure to thrive**, genetic defect (deletion of codon 508 on chromosome 7), and **defective protein folding** are classic for **cystic fibrosis (CF)**.
- In CF, the defective **CFTR protein** (a chloride channel) leads to reduced chloride secretion and increased **sodium absorption** in respiratory epithelial cells, causing thickened mucus.
*Calcium channels of distal tubular cells*
- Dysfunction of **calcium channels** in the distal tubules is not a primary feature of cystic fibrosis.
- Renal calcium handling issues are typically associated with conditions like **Dent's disease** or various types of **renal tubular acidosis**, not CF.
*ATP-sensitive potassium channels of pancreatic beta cells*
- While CF can lead to pancreatic insufficiency and **CF-related diabetes**, the primary defect is not in the **ATP-sensitive potassium channels** of beta cells.
- The insulin deficiency in CF diabetes is due to destruction of pancreatic islets secondary to duct obstruction and inflammation.
*Bicarbonate channels of pancreatic ductal cells*
- In cystic fibrosis, the **CFTR protein** is a chloride channel that also facilitates bicarbonate transport, and its dysfunction does impair **bicarbonate secretion** in pancreatic ductal cells.
- However, the question specifically asks about an *increase* in channel activity, and bicarbonate channel activity is *decreased* in CF.
*Chloride channels of epithelial cells in sweat glands*
- The **CFTR protein** is indeed a **chloride channel** in sweat glands, and in CF, its *activity is decreased*, leading to reduced chloride reabsorption and high sweat chloride (the basis for the sweat test).
- The question asks for an *increased* channel activity, which is seen with sodium channels due to the linked transport mechanisms.
Pancreatic exocrine function US Medical PG Question 9: A 61-year-old woman presents to the urgent care unit with a 2-week history of abdominal pain after meals. The patient reports vomiting over the past few days. The past medical history is significant for osteoarthritis and systemic lupus erythematosus. She regularly drinks alcohol. She does not smoke cigarettes. The patient currently presents with vital signs within normal limits. On physical examination, the patient appears to be in moderate distress, but she is alert and oriented. The palpation of the abdomen elicits tenderness in the epigastric region. The CT of the abdomen shows no signs of an acute process. The laboratory results are listed below. Which of the following is the most likely diagnosis?
Na+ 139 mEq/L
K+ 4.4 mEq/L
Cl- 109 mmol/L
HCO3- 20 mmol/L
BUN 14 mg/dL
Cr 1.0 mg/dL
Glucose 101 mg/dL
Total cholesterol 187 mg/dL
LDL 110 mg/dL
HDL 52 mg/dL
TG 120 mg/dL
AST 65 IU/L
ALT 47 IU/L
GGT 27 IU/L
Amylase 512 U/L
Lipase 1,262 U/L
- A. Acute liver failure
- B. Acute pancreatitis (Correct Answer)
- C. Acute mesenteric ischemia
- D. Acute cholecystitis
- E. Gastric ulcer
Pancreatic exocrine function Explanation: **Acute pancreatitis**
- The patient presents with classic symptoms of **acute pancreatitis**, including **epigastric abdominal pain** that worsens after meals, and **vomiting**.
- Significantly elevated **amylase** (512 U/L) and **lipase** (1,262 U/L) levels (both more than three times the upper limit of normal) confirm the diagnosis. The patient's history of **alcohol consumption** is a major risk factor.
*Acute liver failure*
- Acute liver failure would typically present with significantly elevated **ALT and AST values**, often in the thousands, along with signs of **hepatic encephalopathy** or coagulopathy, none of which are present here.
- While the AST and ALT are mildly elevated, they are not indicative of acute liver failure, and the patient's other liver function tests (GGT, cholesterol panel) are relatively normal.
*Acute mesenteric ischemia*
- **Acute mesenteric ischemia** presents with severe, **disproportionate pain** to physical findings, often described as "pain out of proportion to examination." It is less commonly associated with elevated lipase and amylase.
- While patient has a history of systemic lupus erythematosus that could potentially increase the risk of thrombotic events, the absence of severe abdominal pain and the very high lipase levels make this less likely.
*Acute cholecystitis*
- **Acute cholecystitis** typically presents with right upper quadrant pain, fever, and leukocytosis, often precipitated by fatty meals. **Murphy's sign** is usually positive.
- While abdominal pain after meals and vomiting could occur, the pain is specifically epigastric, and there are no signs of inflammation (fever, WBC count not provided but general physical examination findings are not pointing to cholecystitis) and the remarkably elevated lipase and amylase are not features of cholecystitis.
*Gastric ulcer*
- A **gastric ulcer** typically causes **epigastric pain** that may be relieved by food (duodenal ulcer) or worsened by food (gastric ulcer), and can cause vomiting.
- However, the extremely high **amylase and lipase levels** are not characteristic of a gastric ulcer and point towards a pancreatic etiology.
Pancreatic exocrine function US Medical PG Question 10: A 29-year-old man presents for the evaluation of infertility. He has a history of recurrent lower respiratory tract infections, productive cough, abdominal pain, and diarrhea. Physical examination reveals clubbing and bilateral crackles on chest auscultation. Chest X-ray reveals increased pulmonary markings and peripheral bronchi with a ‘tram track’ appearance. Which of the following pathophysiologies is responsible for the patient’s condition?
- A. Fibrosis of the lung parenchyma
- B. Bronchial hypersensitivity
- C. Abnormal ciliary motion
- D. Gluten hypersensitivity
- E. Defective chloride transport (Correct Answer)
Pancreatic exocrine function Explanation: ***Defective chloride transport***
- The patient's presentation with **recurrent respiratory infections**, **bronchiectasis** (tram track appearance on CXR), **clubbing**, and **infertility** is highly suggestive of **cystic fibrosis**.
- **Cystic fibrosis** is caused by mutations in the **CFTR gene**, leading to **defective chloride transport** across epithelial cells, resulting in thick, viscous secretions.
*Fibrosis of the lung parenchyma*
- While chronic lung disease can lead to some **pulmonary fibrosis**, it is not the primary underlying pathophysiology described here.
- Pulmonary fibrosis typically presents with **restrictive lung disease** and interstitial patterns on imaging, rather than the prominent **bronchiectasis** seen in this patient.
*Bronchial hypersensitivity*
- This is characteristic of **asthma**, which involves airway inflammation and bronchoconstriction, but typically does not cause the extensive **recurrent infections**, **bronchiectasis**, or **infertility** seen in this case.
- Asthma is less likely to result in **clubbing** or the progressive lung damage implied by a "tram track" appearance.
*Abnormal ciliary motion*
- This describes **primary ciliary dyskinesia (PCD)**, which can also cause recurrent respiratory infections and male infertility due to **immotile sperm**.
- However, PCD typically presents with **situs inversus** in a significant proportion of cases and does not involve the characteristic **exocrine gland dysfunction** (e.g., severe abdominal symptoms, pancreatic insufficiency leading to diarrhea) often seen in cystic fibrosis implied by the broad clinical picture.
*Gluten hypersensitivity*
- Also known as **celiac disease**, this is primarily a **gastrointestinal condition** characterized by malabsorption due to immune reactions to gluten.
- While celiac disease can cause **abdominal pain** and **diarrhea**, it does not explain the **recurrent respiratory infections**, **bronchiectasis**, **clubbing**, or **male infertility**.
More Pancreatic exocrine function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.