Lipid digestion and absorption US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lipid digestion and absorption. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lipid digestion and absorption US Medical PG Question 1: A 57-year-old man calls his primary care physician to discuss the results of his annual laboratory exams. The results show that he has dramatically decreased levels of high-density lipoprotein (HDL) and mildly increased levels of low-density lipoprotein (LDL). The physician says that the HDL levels are of primary concern so he is started on the lipid level modifying drug that most effectively increases serum HDL levels. Which of the following is the most likely a side effect of this medication that the patient should be informed about?
- A. Hepatotoxicity
- B. Gallstones
- C. Flushing (Correct Answer)
- D. Malabsorption
- E. Myalgia
Lipid digestion and absorption Explanation: ***Flushing***
- The medication that most effectively increases HDL levels is **niacin (vitamin B3)**.
- A common and well-known side effect of niacin, especially at therapeutic doses, is **cutaneous flushing**, often accompanied by itching and warmth, due to prostaglandin release.
*Hepatotoxicity*
- While some lipid-modifying drugs, particularly statins, can cause hepatotoxicity, it is less characteristic of niacin directly affecting the liver.
- **Niacin** can cause mild liver enzyme elevations but severe hepatotoxicity is rare with standard doses and monitoring.
*Gallstones*
- **Fibrates** (e.g., gemfibrozil, fenofibrate) are known to increase the risk of gallstone formation by increasing cholesterol excretion into bile.
- Fibrates primarily lower triglycerides and can moderately increase HDL, but are not the *most effective* for significantly raising HDL.
*Malabsorption*
- **Bile acid sequestrants** (e.g., cholestyramine, colestipol) can cause malabsorption of fat-soluble vitamins and other drugs.
- These drugs primarily lower LDL and have minimal effects on HDL levels.
*Myalgia*
- **Statins** (HMG-CoA reductase inhibitors) are well-known to cause muscle-related side effects, including myalgia, myopathy, and in severe cases, rhabdomyolysis.
- Statins primarily lower LDL, and their effect on HDL is generally modest.
Lipid digestion and absorption US Medical PG Question 2: What is the primary mechanism for iron absorption in the duodenum?
- A. Simple diffusion
- B. Passive paracellular transport
- C. Endocytosis
- D. DMT1 transporter (Correct Answer)
Lipid digestion and absorption Explanation: ***DMT1 transporter***
- The **divalent metal transporter 1 (DMT1)** is the primary mechanism for absorbing **non-heme iron (ferrous iron, Fe2+)** into duodenal enterocytes.
- This active transport process is pH-dependent and drives iron uptake against a concentration gradient.
*Simple diffusion*
- Applies to the movement of substances down their concentration gradient without the aid of membrane proteins, which is not the main mechanism for iron due to its ionic nature.
- While some highly lipid-soluble substances can cross membranes this way, metal ions like iron require specific transporters.
*Passive paracellular transport*
- Involves substances moving *between* cells, rather than *through* them, often occurring in leaky epithelia.
- While some fluid and electrolytes may use this route, it is not the primary or regulated pathway for iron absorption.
*Endocytosis*
- A process where cells engulf substances by forming vesicles from the plasma membrane.
- While some macromolecules are absorbed via endocytosis, it is not the major mechanism for absorbing dietary iron in the duodenum.
Lipid digestion and absorption US Medical PG Question 3: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Lipid digestion and absorption Explanation: ***It is stimulated by epinephrine***
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Lipid digestion and absorption US Medical PG Question 4: A 51-year-old homeless man presents to the emergency department with severe abdominal pain and cramping for the past 3 hours. He endorses radiation to his back. He adds that he vomited multiple times. He admits having been hospitalized repeatedly for alcohol intoxication and abdominal pain. His temperature is 103.8° F (39.8° C), respiratory rate is 15/min, pulse is 107/min, and blood pressure is 100/80 mm Hg. He refuses a physical examination due to severe pain. Blood work reveals the following:
Serum:
Albumin: 3.2 gm/dL
Alkaline phosphatase: 150 U/L
Alanine aminotransferase: 76 U/L
Aspartate aminotransferase: 155 U/L
Gamma-glutamyl transpeptidase: 202 U/L
Lipase: 800 U/L
What is the most likely diagnosis of this patient?
- A. Duodenal peptic ulcer
- B. Choledocholithiasis
- C. Pancreatitis (Correct Answer)
- D. Cholecystitis
- E. Gallbladder cancer
Lipid digestion and absorption Explanation: ***Pancreatitis***
- The patient's history of **repeated alcohol intoxication** and abdominal pain, combined with **severe abdominal pain radiating to the back**, vomiting, and significantly elevated **lipase (800 U/L)**, are highly indicative of **acute pancreatitis**.
- The elevated **liver enzymes (ALT, AST, GGT)** and **alkaline phosphatase** can be associated with cholestasis or liver involvement often seen in alcohol-induced pancreatitis or can be elevated due to a gallstone lodged in the common bile duct, which is also a common cause of pancreatitis.
*Duodenal peptic ulcer*
- While duodenal ulcers cause severe abdominal pain, they typically present with **epigastric pain** that may be relieved by food, and often cause **melena or hematemesis** if bleeding.
- The extremely high **lipase level** and pain radiating to the back are not characteristic of an uncomplicated duodenal ulcer.
*Choledocholithiasis*
- **Choledocholithiasis** (gallstones in the common bile duct) can cause severe right upper quadrant or epigastric pain and elevated liver enzymes, but it doesn't typically present with an isolated, dramatically high **lipase** level without concomitant pancreatitis.
- The main symptom is **biliary colic**, often post-prandial, and usually involves jaundice or cholangitis if infected.
*Cholecystitis*
- **Cholecystitis** presents with **right upper quadrant pain**, often radiating to the shoulder, associated with fever and nausea, and is usually triggered by fatty meals.
- Although there might be some elevation in liver enzymes and amylase/lipase, the **markedly elevated lipase** and pain radiating to the back are more suggestive of pancreatitis.
*Gallbladder cancer*
- **Gallbladder cancer** typically presents with more insidious symptoms, such as chronic right upper quadrant pain, weight loss, jaundice, and anorexia.
- It would not usually present with an acute episode of **severe abdominal pain and drastically high lipase** in this manner.
Lipid digestion and absorption US Medical PG Question 5: A 12-year-old boy is brought to the emergency department because of acute onset abdominal pain. On arrival, he also complains of nausea and shortness of breath in addition to epigastric pain. He has previously been admitted to the hospital several times for respiratory infections with Pseudomonas species and uses a nebulizer and a chest wall oscillation vest at home. The patient's acute condition is found to be due to premature activation of an enzyme that normally interacts with the brush border. Which of the following describes the activity of this enzyme?
- A. Activates pancreatic enzyme precursors (Correct Answer)
- B. Breaks down elastin molecules
- C. Hydrolyzes phospholipids
- D. Digests triglycerides
- E. Activates phospholipase A2
Lipid digestion and absorption Explanation: ***Activates pancreatic enzyme precursors***
- The patient's history of **recurrent respiratory infections with Pseudomonas** and use of a **nebulizer/chest wall oscillation vest** strongly suggests **cystic fibrosis (CF)**.
- In cystic fibrosis, **thickened secretions** can obstruct the pancreatic ducts, leading to **autodigestion of the pancreas** due to obstruction preventing the release of pancreatic enzymes. The enzyme being referred to is **trypsin**, which, when prematurely activated, activates other pancreatic enzyme precursors, leading to **pancreatitis**.
*Breaks down elastin molecules*
- This activity is characteristic of **elastase**, an enzyme produced by the pancreas. While elastase is involved in the overall digestive process and can be prematurely activated, its primary role is not the one alluded to in the clinical presentation, which points to **pancreatitis** from premature activation of the cascade.
- Damage to elastin is more classically associated with conditions like **emphysema** (due to alpha-1 antitrypsin deficiency) rather than acute abdominal pain secondary to autodigestion.
*Hydrolyzes phospholipids*
- This is the function of **phospholipase**, another pancreatic enzyme. While also capable of contributing to pancreatic autodigestion if prematurely activated, it is typically activated by **trypsin**, making trypsin the primary enzyme responsible for initiating the cascade of activation.
- **Phospholipase A2** acts on phospholipids, but the question describes an enzyme that *normally interacts with the brush border* before activation of the precursors begins.
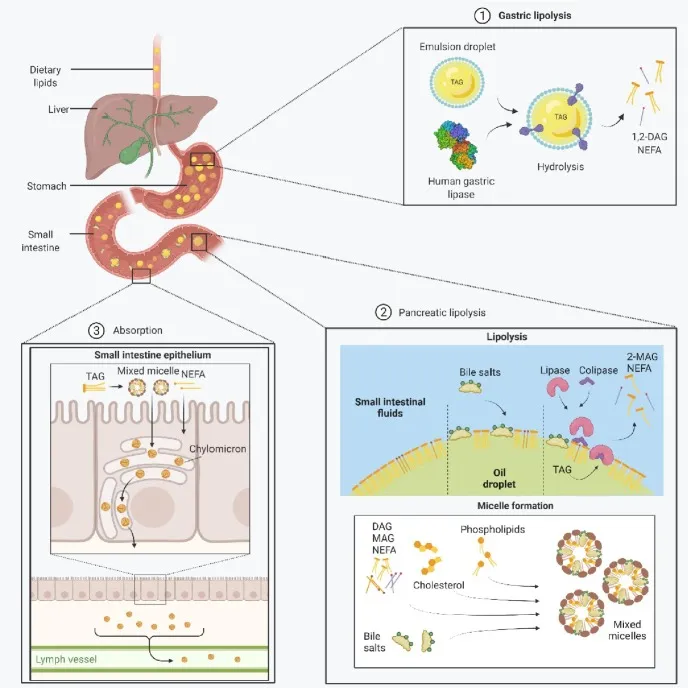
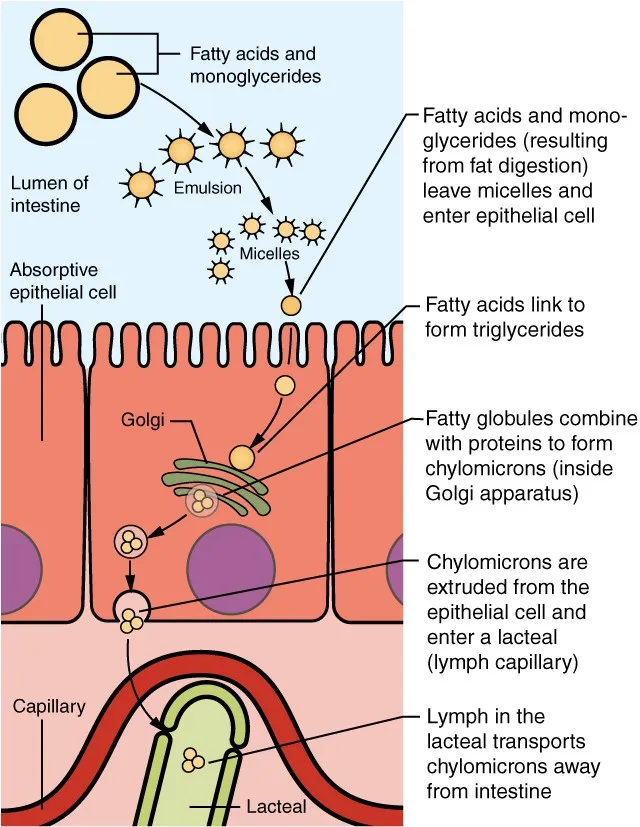
*Digests triglycerides*
- This is the function of **pancreatic lipase**. Premature activation of lipase can contribute to the fat necrosis seen in pancreatitis.
- However, lipase, like many other pancreatic enzymes, is activated by **trypsin**, which is the initial enzyme in the cascade of activation leading to autodigestion.
*Activates phospholipase A2*
- This describes the action of **trypsinogen turning into trypsin**, which then activates other proenzymes like **prophospholipase A2**.
- While correct that trypsin activates phospholipase A2, the question asks about the primary enzyme whose *premature activation* causes the issue, which is **trypsin** itself, as it activates *multiple* pancreatic enzyme precursors, initiating a cascade.
Lipid digestion and absorption US Medical PG Question 6: A 54-year-old man presents to his primary care physician with a 2-month-history of diarrhea. He says that he feels the urge to defecate 3-4 times per day and that his stools have changed in character since the diarrhea began. Specifically, they now float, stick to the side of the toilet bowl, and smell extremely foul. His past medical history is significant for several episodes of acute pancreatitis secondary to excessive alcohol consumption. His symptoms are found to be due to a deficiency in an enzyme. Which of the following enzymes is most likely deficient in this patient?
- A. Enterokinase
- B. Amylase
- C. Colipase
- D. Lipase (Correct Answer)
- E. Chymotrypsin
Lipid digestion and absorption Explanation: ***Lipase***
- The patient's history of **recurrent pancreatitis** likely led to **exocrine pancreatic insufficiency**, reducing the production of digestive enzymes, particularly **lipase**.
- **Steatorrhea** (foul-smelling, floating, sticky stools) is a classic symptom of **fat malabsorption**, which occurs due to insufficient lipase for triglyceride digestion.
*Enterokinase*
- **Enterokinase** is an enzyme produced in the **duodenum** that activates trypsinogen to trypsin, which then activates other pancreatic proteases.
- A deficiency would primarily cause **protein malabsorption**, not the pronounced fat malabsorption (steatorrhea) seen in this patient.
*Amylase*
- **Amylase** is responsible for **carbohydrate digestion**.
- While chronic pancreatitis can lead to amylase deficiency, the primary symptom of this patient's diarrhea, steatorrhea, points more directly to **fat malabsorption** rather than carbohydrate malabsorption.
*Colipase*
- **Colipase** is a co-enzyme that helps **lipase** bind to the fat-water interface to digest triglycerides.
- While essential for fat digestion, lipase itself is the primary enzyme responsible, and a direct deficiency in colipase alone is less commonly implicated as the sole cause of severe steatorrhea than a general pancreatic enzyme insufficiency affecting lipase production.
*Chymotrypsin*
- **Chymotrypsin** is a **protease** primarily involved in **protein digestion**.
- A deficiency would lead to **protein malabsorption**, which typically presents with symptoms like muscle wasting and edema, rather than the prominent steatorrhea described.
Lipid digestion and absorption US Medical PG Question 7: A researcher is studying proteins that contribute to intestinal epithelial permeability. He has isolated intestinal tissue from several mice. After processing the tissue into its individual components, he uses a Western blot analysis to identify a protein that forms part of a multi-protein complex at the apical aspect of epithelial cells. The complex is known to provide a diffusion barrier between the apical and basolateral aspects of epithelial cells. Which of the following proteins is this researcher most likely investigating?
- A. Integrin
- B. Connexon
- C. Desmoglein
- D. E-cadherin
- E. Claudin (Correct Answer)
Lipid digestion and absorption Explanation: ***Claudin***
- **Claudins** are integral membrane proteins that are primary components of **tight junctions** (zonulae occludentes), which form a diffusion barrier at the **apical aspect** of epithelial cells.
- They regulate **paracellular permeability**, crucial for maintaining the integrity of the intestinal epithelial barrier.
*Integrin*
- **Integrins** are transmembrane receptors that mediate cell-extracellular matrix (ECM) adhesion and cell-cell adhesion, but they are not the primary components of tight junction diffusion barriers.
- They are involved in cell signaling and structural support, rather than forming a direct paracellular seal.
*Connexon*
- A **connexon** is a protein assembly that forms a **gap junction**, allowing direct communication and passage of small molecules between adjacent cells.
- Gap junctions facilitate intercellular communication, but do not primarily contribute to sealing the paracellular space as a diffusion barrier.
*Desmoglein*
- **Desmoglein** is a cadherin family protein found in **desmosomes** (maculae adherens), which are cell-cell adhesion complexes that provide strong mechanical attachments between cells.
- Desmosomes resist shearing forces and provide structural integrity but do not regulate paracellular permeability as tight junctions do.
*E-cadherin*
- **E-cadherin** is a crucial component of **adherens junctions** (zonula adherens), which provide cell-cell adhesion and help establish and maintain cell polarity.
- While important for epithelial integrity, E-cadherin primarily links cells to the actin cytoskeleton and is not directly responsible for forming the selective diffusion barrier itself.
Lipid digestion and absorption US Medical PG Question 8: A 21-year-old college student comes to the emergency department because of a two-day history of vomiting and epigastric pain that radiates to the back. He has a history of atopic dermatitis and Hashimoto thyroiditis. His only medication is levothyroxine. He has not received any routine vaccinations. He drinks 1–2 beers on the weekends and occasionally smokes marijuana. The patient appears distressed and is diaphoretic. His temperature is 37.9°C (100.3°F), pulse is 105/min, respirations are 16/min, and blood pressure is 130/78 mm Hg. Physical examination shows abdominal distention with tenderness to palpation in the epigastrium. There is no guarding or rebound tenderness. Skin examination shows several clusters of yellow plaques over the trunk and extensor surfaces of the extremities. Hemoglobin concentration is 15.2 g/dL and serum calcium concentration is 7.9 mg/dL. Which of the following is the most appropriate next step in evaluation?
- A. Measure serum mumps IgM titer
- B. Measure serum lipid levels (Correct Answer)
- C. Obtain an upright x-ray of the abdomen
- D. Perform a pilocarpine-induced sweat test
- E. Measure stool elastase level
Lipid digestion and absorption Explanation: ***Measure serum lipid levels***
- This patient presents with **epigastric pain radiating to the back**, vomiting, and potential signs of systemic inflammation (fever, tachycardia), suggestive of **pancreatitis**. One of the most common causes of pancreatitis, especially in the absence of gallstones or significant alcohol abuse, is **severe hypertriglyceridemia**.
- The presence of **yellow plaques over the trunk and extensor surfaces** (likely **eruptive xanthomas**) is a strong indicator of **severe hypertriglyceridemia**, making serum lipid measurement the most appropriate next step to confirm this etiology for his pancreatitis.
*Measure serum mumps IgM titer*
- While mumps can cause pancreatitis, this patient has not received routine vaccinations, but there is no specific exposure history or other symptoms (like **parotitis**) to strongly suggest mumps as the primary cause.
- The more compelling physical finding of eruptive xanthomas points more directly to **hypertriglyceridemia** as the cause of pancreatitis.
*Obtain an upright x-ray of the abdomen*
- An upright abdominal x-ray is primarily used to look for **free air under the diaphragm** as an indicator of a perforated viscus, which would present with peritonitis and guarding. This patient has **no guarding or rebound tenderness**.
- While it can show signs of ileus, it is not the most targeted test for diagnosing the *cause* of pancreatitis or conditions indicated by eruptive xanthomas.
*Perform a pilocarpine-induced sweat test*
- A **pilocarpine-induced sweat test** is used to diagnose **cystic fibrosis (CF)**, which can cause pancreatic insufficiency and pancreatitis, especially in younger individuals.
- While CF could be considered in a young patient with pancreatic symptoms, his presentation with clear signs of **hyperlipidemia (eruptive xanthomas)** makes this a less direct or immediate next step.
*Measure stool elastase level*
- **Stool elastase** is a test for **exocrine pancreatic insufficiency**, indicating chronic damage to the pancreas.
- This patient is presenting with acute pancreatitis, not chronic insufficiency, and the prominent physical findings point to an **acute metabolic cause** rather than chronic pancreatic dysfunction as the primary differential at this stage.
Lipid digestion and absorption US Medical PG Question 9: A 39-year-old woman presents to her primary care physician because she has been experiencing intermittent abdominal pain for the last 2 weeks. She says that the pain is squeezing in nature, is located in the right upper quadrant, and is particularly severe after eating a meal. After a diagnosis is made, the patient asks why the pain gets worse after eating. The physician explains that food is detected by the gastrointestinal tract through numerous receptors and that this information is transmitted to other parts of the body to cause compensatory changes. The neurons responsible for transmitting this information are most likely located in a layer of the intestine that has which of the following characteristics?
- A. Contracts to generate local movement in mucosa
- B. Contains cells that primarily absorb nutrients
- C. Connective tissue that envelops the other layers
- D. Contracts to generate peristaltic waves (Correct Answer)
- E. Contains large blood vessels and large lymphatic vessels
Lipid digestion and absorption Explanation: ***Contracts to generate peristaltic waves***
- This describes the **muscularis propria** (external muscle layer), which contains the **myenteric plexus (Auerbach's plexus)** between its inner circular and outer longitudinal smooth muscle layers.
- The **myenteric plexus is the primary neural network** responsible for detecting food through mechanoreceptors and chemoreceptors, transmitting sensory information, and coordinating both local reflexes and systemic compensatory responses throughout the gastrointestinal tract.
- These neurons communicate with the **autonomic nervous system** and coordinate the release of hormones like **cholecystokinin (CCK)** after eating, which causes gallbladder contraction (relevant to this patient's postprandial pain from cholecystitis).
- While this layer's most obvious function is generating peristalsis, it contains the most extensive enteric nervous system network for sensory integration and motor coordination.
*Contains large blood vessels and large lymphatic vessels*
- This describes the **submucosa**, which contains the **submucosal plexus (Meissner's plexus)**.
- While the submucosal plexus does contain sensory neurons, it primarily regulates **local functions** such as mucosal secretion, absorption, and blood flow rather than the broader systemic compensatory responses described in the question.
- The submucosa's neural network is more limited compared to the myenteric plexus.
*Contracts to generate local movement in mucosa*
- This describes the **muscularis mucosae**, a thin layer of smooth muscle within the mucosa that causes local folding and movement of the mucosal surface.
- This layer lacks significant neural plexuses and is not involved in transmitting sensory information for systemic responses.
*Contains cells that primarily absorb nutrients*
- This refers to the **mucosa**, specifically the epithelial cells lining the intestinal surface.
- While the mucosa contains chemoreceptors and mechanoreceptors, the question asks about the neurons that **transmit** this information, which are located in the deeper neural plexuses (primarily myenteric), not in the absorptive epithelium itself.
*Connective tissue that envelops the other layers*
- This describes the **serosa** (or adventitia), the outermost protective layer.
- The serosa contains minimal neural tissue and is not involved in sensory detection or transmission of gastrointestinal information.
Lipid digestion and absorption US Medical PG Question 10: A 35-year-old woman presents with exertional dyspnea and fatigue for the past 3 weeks. She says there has been an acute worsening of her dyspnea in the past 5 days. On physical examination, the mucous membranes show pallor. Cardiac exam is significant for the presence of a mid-systolic murmur loudest in the 2nd left intercostal space. A CBC and peripheral blood smear show evidence of microcytic, hypochromic anemia. Which of the following parts of the GI tract is responsible for the absorption of the nutrient whose deficiency is most likely responsible for this patient’s condition?
- A. Duodenum (Correct Answer)
- B. Jejunum
- C. Terminal ileum
- D. Body of the stomach
- E. Antrum of the stomach
Lipid digestion and absorption Explanation: ***Duodenum***
- The patient's presentation with **exertional dyspnea**, **fatigue**, **pallor**, and **microcytic, hypochromic anemia** strongly indicates **iron deficiency anemia**.
- The **duodenum** is the primary site for **iron absorption** in the gastrointestinal tract, specifically in its acidic environment.
*Jejunum*
- The jejunum is primarily responsible for the absorption of most **nutrients** like carbohydrates, proteins, and fats.
- While some minimal iron absorption can occur here, it is not the main site for **dietary iron uptake**.
*Terminal ileum*
- The **terminal ileum** is the key site for the absorption of **vitamin B12** (cobalamin) and **bile salts**.
- Deficiency in vitamin B12 leads to **macrocytic anemia**, which is not consistent with this patient's microcytic anemia.
*Body of the stomach*
- The body of the stomach produces **hydrochloric acid** and **intrinsic factor** from parietal cells.
- While HCl is crucial for releasing iron from food, the stomach itself is not a primary site for **iron absorption**.
*Antrum of the stomach*
- The antrum of the stomach is mainly involved in **grinding food** and initiating digestion, as well as producing **gastrin**.
- It plays no direct role in the absorption of **iron** or other micronutrients responsible for the patient's anemic symptoms.
More Lipid digestion and absorption US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.