Intestinal barrier function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intestinal barrier function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intestinal barrier function US Medical PG Question 1: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Intestinal barrier function Explanation: ***NF-κB***
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
Intestinal barrier function US Medical PG Question 2: An investigator is studying the effect of different cytokines on the growth and differentiation of B cells. The investigator isolates a population of B cells from the germinal center of a lymph node. After exposure to a particular cytokine, these B cells begin to produce an antibody that prevents attachment of pathogens to mucous membranes but does not fix complement. Which of the following cytokines is most likely responsible for the observed changes in B-cell function?
- A. Interleukin-5 (Correct Answer)
- B. Interleukin-6
- C. Interleukin-8
- D. Interleukin-2
- E. Interleukin-4
Intestinal barrier function Explanation: ***Interleukin-5***
- The antibody described (prevents pathogen attachment to mucous membranes, does not fix complement) is characteristic of **IgA**.
- **IL-5** plays a crucial role in promoting **IgA secretion** by differentiated B cells and supports B cell growth and differentiation in mucosal immunity.
- IL-5 works synergistically with **TGF-β** (the primary cytokine for IgA class switching) to enhance IgA production, particularly in mucosal-associated lymphoid tissue.
- Among the options provided, **IL-5 has the strongest association with IgA production**.
*Interleukin-4*
- **IL-4** is the primary cytokine driving class switching to **IgE** (and IgG4), not IgA.
- IL-4 is central to **allergic responses** and type 2 immunity, promoting B cells to produce IgE antibodies against allergens and parasites.
- It does not play a significant role in IgA production or mucosal immunity.
*Interleukin-6*
- **IL-6** is a pleiotropic cytokine involved in acute phase reactions, inflammation, and promoting B cell **differentiation into plasma cells**.
- While it supports general B cell maturation and antibody secretion, it is not specifically associated with **IgA production** or class switching.
*Interleukin-8*
- **IL-8** (CXCL8) is a **chemokine** that primarily recruits and activates neutrophils during inflammation.
- It has no direct role in B cell class switching or antibody production.
*Interleukin-2*
- **IL-2** is essential for T cell proliferation and differentiation, enhancing **cell-mediated immunity**.
- While it can indirectly affect B cell responses through T cell help, it is not directly responsible for promoting **IgA production** or class switching.
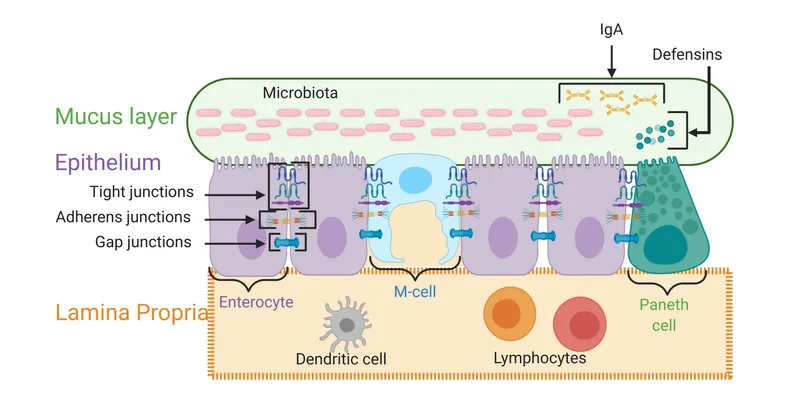
Intestinal barrier function US Medical PG Question 3: An investigator is studying the interaction between epithelial cells and calcium ion concentration. When the calcium ion concentration available to a sample of epithelial tissue is decreased, an increased gap between adjacent epithelial cells is seen on electron microscopy. This observed decrease in cell adhesion is most likely due to an effect on which of the following proteins?
- A. Actin
- B. Integrin
- C. Cadherin (Correct Answer)
- D. Claudin
- E. Cytokeratin
Intestinal barrier function Explanation: ***Cadherin***
- **Cadherins** are calcium-dependent adhesion proteins that mediate cell-to-cell adhesion, particularly in epithelial tissues.
- A decrease in calcium concentration would directly impair cadherin function, leading to reduced cell adhesion and increased intercellular gaps.
*Actin*
- **Actin** is a component of the cell's cytoskeleton, involved in cell shape, motility, and intracellular transport, but not directly responsible for calcium-dependent cell adhesion between epithelial cells.
- While actin filaments interact with adhesion junctions, their primary role is structural and dynamic rather than adhesive.
*Integrin*
- **Integrins** are primarily involved in cell-to-extracellular matrix adhesion, connecting the cell to the surrounding matrix, not directly mediating calcium-dependent cell-to-cell adhesion between epithelial cells.
- They can be affected by intracellular calcium signaling but do not directly bind calcium to mediate their adhesive function in the same way cadherins do.
*Claudin*
- **Claudins** are key components of **tight junctions**, which regulate paracellular permeability and form a barrier between cells, but they are not directly responsible for calcium-dependent cell-to-cell adhesion, which is characteristic of adherens junctions.
- While tight junctions contribute to overall cell-cell contact, the observation of an *increased gap* suggests an issue with adhesive complexes like adherens junctions, where cadherins are prominent.
*Cytokeratin*
- **Cytokeratins** are intermediate filaments found in epithelial cells, providing structural support and mechanical strength.
- They are linked to desmosomes and hemidesmosomes but are not directly involved in calcium-dependent cell-to-cell adhesion.
Intestinal barrier function US Medical PG Question 4: A 36-year-old man undergoes ileocecal resection after a gunshot injury. The resected ileocecal segment is sent for histological evaluation. One of the slides derived from the specimen is shown in the image. Which of the following statements regarding the structure marked within the red circle is correct?
- A. This structure can be only found in the colon.
- B. These structures mostly contain M-cells.
- C. This structure can become a site of entry of certain microorganisms including S. typhi. (Correct Answer)
- D. This structure only appears in case of bacterial infection.
- E. Infants have the largest amount of these structures within their intestinal wall.
Intestinal barrier function Explanation: ***This structure can become a site of entry of certain microorganisms including S. typhi.***
- The image illustrates **Peyer's patches**, which are lymphoid follicles found primarily in the ileum. These structures are rich in **M-cells**, which sample antigens from the intestinal lumen.
- While M-cells are crucial for initiating immune responses, some pathogens like *Salmonella typhi* exploit them to **translocate across the intestinal barrier** and disseminate, leading to systemic infection.
*This structure can be only found in the colon.*
- The structure shown is a **Peyer's patch**, which is predominantly found in the **ileum** of the small intestine, not exclusively in the colon.
- While lymphoid tissue is present throughout the GI tract, these large aggregated lymphoid nodules are characteristic of the ileum.
*These structures mostly contain M-cells.*
- While **M-cells (microfold cells)** are indeed present in the dome epithelium overlying Peyer's patches and are critical for antigen sampling, they constitute a minority of the cells within the entire structure.
- The bulk of Peyer's patches consists of **lymphocytes** (B cells, T cells), macrophages, and dendritic cells, forming lymphoid follicles and interfollicular areas.
*This structure only appears in case of bacterial infection.*
- **Peyer's patches** are a normal and permanent component of the gut-associated lymphoid tissue (GALT) and are present in healthy individuals.
- They serve as crucial sites for **immune surveillance** and the induction of adaptive immune responses to both commensal bacteria and pathogens, even in the absence of an active infection.
*Infants have the largest amount of these structures within their intestinal wall.*
- Peyer's patches are **well-developed at birth** and continue to increase in size and number during childhood and adolescence.
- They tend to **atrophy with age**, meaning that young adults and adolescents typically have the most prominent and numerous Peyer's patches, not infants.
Intestinal barrier function US Medical PG Question 5: A researcher is studying proteins that contribute to intestinal epithelial permeability. He has isolated intestinal tissue from several mice. After processing the tissue into its individual components, he uses a Western blot analysis to identify a protein that forms part of a multi-protein complex at the apical aspect of epithelial cells. The complex is known to provide a diffusion barrier between the apical and basolateral aspects of epithelial cells. Which of the following proteins is this researcher most likely investigating?
- A. Integrin
- B. Connexon
- C. Desmoglein
- D. E-cadherin
- E. Claudin (Correct Answer)
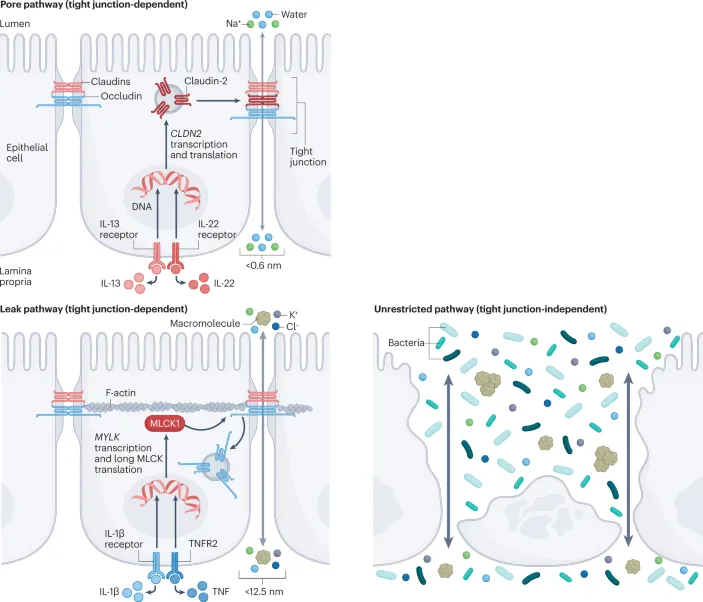
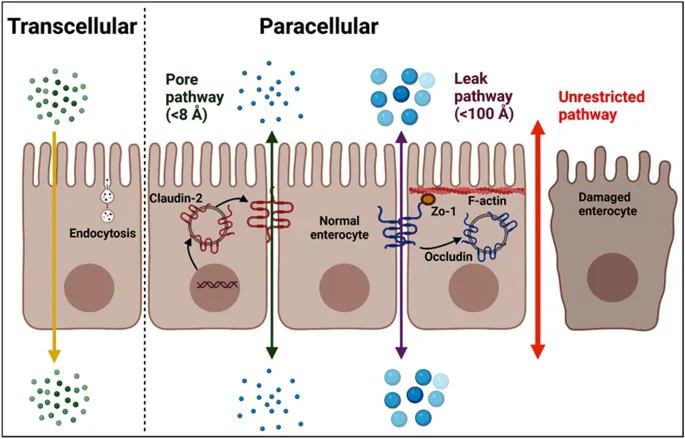
Intestinal barrier function Explanation: ***Claudin***
- **Claudins** are integral membrane proteins that are primary components of **tight junctions** (zonulae occludentes), which form a diffusion barrier at the **apical aspect** of epithelial cells.
- They regulate **paracellular permeability**, crucial for maintaining the integrity of the intestinal epithelial barrier.
*Integrin*
- **Integrins** are transmembrane receptors that mediate cell-extracellular matrix (ECM) adhesion and cell-cell adhesion, but they are not the primary components of tight junction diffusion barriers.
- They are involved in cell signaling and structural support, rather than forming a direct paracellular seal.
*Connexon*
- A **connexon** is a protein assembly that forms a **gap junction**, allowing direct communication and passage of small molecules between adjacent cells.
- Gap junctions facilitate intercellular communication, but do not primarily contribute to sealing the paracellular space as a diffusion barrier.
*Desmoglein*
- **Desmoglein** is a cadherin family protein found in **desmosomes** (maculae adherens), which are cell-cell adhesion complexes that provide strong mechanical attachments between cells.
- Desmosomes resist shearing forces and provide structural integrity but do not regulate paracellular permeability as tight junctions do.
*E-cadherin*
- **E-cadherin** is a crucial component of **adherens junctions** (zonula adherens), which provide cell-cell adhesion and help establish and maintain cell polarity.
- While important for epithelial integrity, E-cadherin primarily links cells to the actin cytoskeleton and is not directly responsible for forming the selective diffusion barrier itself.
Intestinal barrier function US Medical PG Question 6: Which neurotransmitter primarily mediates slow synaptic transmission in the enteric nervous system?
- A. Substance P
- B. Serotonin
- C. Acetylcholine
- D. Nitric oxide (Correct Answer)
Intestinal barrier function Explanation: **Nitric oxide**
- **Nitric oxide (NO)** is a key **non-classical neurotransmitter** in the **enteric nervous system (ENS)**, mediating **slow synaptic transmission** due to its gaseous nature allowing for diffusion and longer-lasting effects.
- It is involved in **smooth muscle relaxation**, **vasodilation**, and diverse gastrointestinal functions, including **peristalsis** and **sphincter relaxation**.
*Substance P*
- **Substance P** is a **neuropeptide** that acts as an **excitatory neurotransmitter** in the ENS, primarily mediating **fast synaptic transmission** and smooth muscle contraction.
- It is involved in pain perception, inflammation, and is released by sensory neurons and some enteric neurons.
*Serotonin*
- **Serotonin (5-HT)** is a major neurotransmitter in the ENS, largely mediating **fast excitatory or inhibitory synaptic transmission** depending on the receptor subtype.
- It plays a crucial role in regulating gut motility, secretion, and visceral sensation, and is involved in both rapid signaling and neuromodulation.
*Acetylcholine*
- **Acetylcholine (ACh)** is the primary **excitatory neurotransmitter** of the **parasympathetic nervous system** within the ENS, mediating **fast synaptic transmission** by binding to nicotinic and muscarinic receptors.
- It is crucial for stimulating **smooth muscle contraction** (promoting peristalsis), increasing glandular secretions, and generally enhancing gut motility.
Intestinal barrier function US Medical PG Question 7: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Intestinal barrier function Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Intestinal barrier function US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Intestinal barrier function Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Intestinal barrier function US Medical PG Question 9: A 55-year-old woman presents with acute onset abdominal pain radiating to her back, nausea, and vomiting. CT scan suggests a diagnosis of acute pancreatitis. The pathogenesis of acute pancreatitis relates to inappropriate activation of trypsinogen to trypsin. Which of the following activates trypsin in normal digestion?
- A. Secretin
- B. Lipase
- C. Cholecystokinin
- D. Enterokinase (Correct Answer)
- E. Amylase
Intestinal barrier function Explanation: ***Enterokinase***
- **Enterokinase** (also known as enteropeptidase) is a brush border enzyme of the duodenum that specifically cleaves and activates pancreatic **trypsinogen** into its active form, **trypsin**.
- Once activated, **trypsin** then activates other pancreatic proteases (e.g., chymotrypsinogen, procarboxypeptidases, proelastase) within the intestinal lumen.
*Secretin*
- **Secretin** is a hormone released by S cells in the duodenum in response to acidic chyme and acts on the pancreas to stimulate the secretion of **bicarbonate-rich fluid**, which neutralizes gastric acid.
- It does not directly activate digestive enzymes like trypsinogen.
*Lipase*
- **Lipase** is a pancreatic enzyme secreted in its active form that breaks down **dietary fats** (triglycerides) into fatty acids and monoglycerides.
- It plays no role in the activation of trypsinogen.
*Cholecystokinin*
- **Cholecystokinin (CCK)** is a hormone released by I cells in the duodenum in response to fats and proteins, stimulating the contraction of the **gallbladder** and the secretion of **pancreatic enzymes**.
- While it promotes the release of pancreatic enzymes, it does not directly activate trypsinogen.
*Amylase*
- **Amylase** is a pancreatic enzyme secreted in its active form that breaks down **complex carbohydrates** (starches) into simpler sugars (disaccharides and oligosaccharides).
- It is not involved in the activation cascade of pancreatic proteases.
Intestinal barrier function US Medical PG Question 10: A 32-year-old female with Crohn's disease diagnosed in her early 20s comes to your office for a follow-up appointment. She is complaining of headaches and fatigue. Which of the following arterial blood gas findings might you expect?
- A. High PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
- B. Low PaO2, low O2 saturation (SaO2), low O2 content (CaO2)
- C. Normal PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
- D. Normal PaO2, normal O2 saturation (SaO2), low O2 content (CaO2) (Correct Answer)
- E. Low PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
Intestinal barrier function Explanation: ***Normal PaO2, normal O2 saturation (SaO2), low O2 content (CaO2)***
- Patients with **Crohn's disease** are prone to developing **iron deficiency anemia** due to chronic inflammation, malabsorption, and blood loss, leading to reduced hemoglobin levels.
- While PaO2 and SaO2 measure oxygen *tension* and *percentage saturation* of available hemoglobin, respectively, **O2 content (CaO2)** directly reflects the *total amount* of oxygen delivered to tissues, which is primarily dependent on hemoglobin concentration. Therefore, with anemia, CaO2 will be low despite normal PaO2 and SaO2 because there is less hemoglobin to carry oxygen.
*High PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- High PaO2 would indicate **hyperoxygenation**, which is not an expected complication of Crohn's disease or its associated anemia.
- Normal O2 content is inconsistent with the presence of anemia, which significantly reduces the body's total oxygen-carrying capacity.
*Low PaO2, low O2 saturation (SaO2), low O2 content (CaO2)*
- Low PaO2 and SaO2 suggest a primary **respiratory problem** or severe hypoxemia, which is not directly linked to Crohn's disease or the typical presentation of iron deficiency anemia.
- While low O2 content is correct for anemia, the accompanying low PaO2 and SaO2 indicate a different underlying pathology for oxygen transport issues.
*Normal PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- This finding would indicate **normal oxygenation** and oxygen-carrying capacity, which is contrary to the clinical scenario of a patient with Crohn's likely complicated by anemia.
- The patient's symptoms of headaches and fatigue are consistent with poor tissue oxygenation, which would not occur if all these parameters were normal.
*Low PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- A low PaO2 with a normal SaO2 is physiologically unlikely unless there is a **left shift of the oxygen dissociation curve** with adequate hemoglobin, which doesn't fit the expected anemic state.
- Normal O2 content would rule out the presence of anemia as a cause for the symptoms, which is a common complication in Crohn's disease.
More Intestinal barrier function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.