Gut microbiome interactions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gut microbiome interactions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gut microbiome interactions US Medical PG Question 1: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Gut microbiome interactions Explanation: ***NF-κB***
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
Gut microbiome interactions US Medical PG Question 2: An 87-year-old male nursing home resident is currently undergoing antibiotic therapy for the treatment of a decubitus ulcer. One week into the treatment course, he experiences several episodes of watery diarrhea. Subsequent sigmoidoscopy demonstrates the presence of diffuse yellow plaques on the mucosa of the sigmoid colon. Which of the following is the best choice of treatment for this patient?
- A. Intravenous vancomycin
- B. Intravenous gentamicin
- C. Oral metronidazole (Correct Answer)
- D. Oral trimethoprim/sulfamethoxazole
- E. Oral morphine
Gut microbiome interactions Explanation: ***Oral metronidazole***
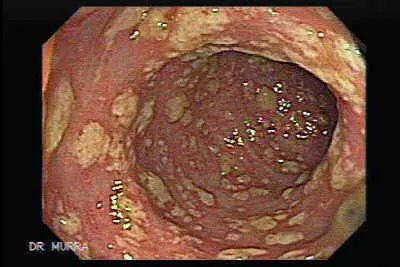
- The patient's presentation with **watery diarrhea** and **yellow plaques (pseudomembranes) on sigmoidoscopy** after antibiotic therapy is classic for **Clostridioides difficile infection (CDI)**.
- Among the options provided, **oral metronidazole** is the best choice as it achieves therapeutic concentrations in the colonic lumen and has activity against C. difficile.
- Current **IDSA guidelines** recommend oral **vancomycin or fidaxomicin** as first-line therapy for CDI; however, metronidazole remains an acceptable alternative, particularly in resource-limited settings or when first-line agents are unavailable.
- Metronidazole has good **colonic penetration** when administered orally and is effective against anaerobic bacteria including C. difficile.
*Intravenous vancomycin*
- While **vancomycin** is highly effective against C. difficile, it **must be administered orally** to treat CDI because IV vancomycin does not achieve adequate concentrations in the gut lumen.
- Intravenous vancomycin is excreted primarily by the kidneys and does not reach the colonic mucosa in therapeutic amounts.
- IV vancomycin is appropriate for systemic infections like **MRSA bacteremia or endocarditis**, but not for intestinal infections like CDI.
*Intravenous gentamicin*
- **Gentamicin** is an aminoglycoside antibiotic effective against **gram-negative bacteria** but has **no activity against C. difficile**, which is a gram-positive anaerobic bacillus.
- Aminoglycosides carry significant risks of **nephrotoxicity and ototoxicity**, making them inappropriate for this clinical scenario.
- Use of gentamicin would not address the underlying CDI and could worsen outcomes.
*Oral trimethoprim/sulfamethoxazole*
- **Trimethoprim/sulfamethoxazole** is a broad-spectrum antibiotic effective for various infections (UTIs, Pneumocystis, etc.) but has **no significant activity against C. difficile**.
- Continued antibiotic use with agents ineffective against C. difficile could further disrupt normal gut flora and potentially **worsen the CDI**.
*Oral morphine*
- **Morphine** is an opioid analgesic with **no antibacterial properties** and therefore cannot treat bacterial infections like CDI.
- Opioids can actually **slow gastrointestinal motility**, which may worsen outcomes in CDI by prolonging exposure to toxins.
- While it might provide symptomatic relief of abdominal discomfort, it does not address the underlying infection and is contraindicated in infectious diarrhea.
Gut microbiome interactions US Medical PG Question 3: A 2-day-old newborn male delivered at 38 weeks' gestation is evaluated for poor feeding and irritability. His temperature is 35°C (95°F), pulse is 168/min, respirations are 80/min, and blood pressure is 60/30 mm Hg. Blood culture on sheep agar grows motile, gram-positive bacteria surrounded by a narrow clear zone. Further testing confirms the presence of a pore-forming toxin. Which of the following is the most important factor in successful clearance of the causal pathogen?
- A. Secretion of interferon-α from infected cells
- B. Secretion of interleukin 10 by regulatory T cells
- C. Interferon-γ-induced macrophage activation (Correct Answer)
- D. Secretion of immunoglobulin G from plasma cells
- E. Formation of the membrane attack complex
Gut microbiome interactions Explanation: ***Interferon-γ-induced macrophage activation***
- This clinical presentation of severe sepsis in a neonate, with a gram-positive, motile, pore-forming bacterium, is highly suggestive of **Listeria monocytogenes infection**.
- **Listeria** is an intracellular bacterium that primarily targets macrophages and monocytes, and its clearance crucially depends on a strong **cell-mediated immune response**, specifically **IFN-γ-mediated macrophage activation** to kill the intracellular pathogens.
*Secretion of interferon-α from infected cells*
- **Interferon-α** is mainly involved in the antiviral response, inhibiting viral replication and activating natural killer (NK) cells.
- While it has some role in innate immunity against bacteria, it is not the primary or most critical mechanism for clearing an intracellular bacterial infection like *Listeria*.
*Secretion of interleukin 10 by regulatory T cells*
- **Interleukin 10 (IL-10)** is an anti-inflammatory cytokine that downregulates the immune response, often associated with immune suppression and tolerance.
- Secreting IL-10 would likely **hinder** the effective clearance of an active bacterial infection rather than promote it.
*Secretion of immunoglobulin G from plasma cells*
- **Immunoglobulin G (IgG)** provides humoral immunity against extracellular bacteria and toxins, mediating opsonization and neutralization.
- While IgG may have some role in controlling the extracellular phase of *Listeria* infection, it is **ineffective** against the intracellular forms, which are the main challenge for clearance.
*Formation of the membrane attack complex*
- The **membrane attack complex (MAC)** is part of the complement system, which primarily targets and lyses extracellular bacteria.
- *Listeria* is an intracellular pathogen, meaning the MAC would not be able to reach and effectively lyse the bacteria once inside host cells.
Gut microbiome interactions US Medical PG Question 4: A 10-year-old girl is brought to the emergency department because of a 2-day history of bloody diarrhea and abdominal pain. Four days ago, she visited a petting zoo with her family. Her temperature is 39.4°C (102.9°F). Abdominal examination shows tenderness to palpation of the right lower quadrant. Stool cultures at 42°C grow colonies that turn black after adding phenylenediamine. Which of the following best describes the most likely causal organism?
- A. Gram-positive, anaerobic, rod-shaped bacteria that form spores
- B. Gram-positive, aerobic, rod-shaped bacteria that produce catalase
- C. Gram-negative, non-flagellated bacteria that do not ferment lactose
- D. Gram-negative, flagellated bacteria that do not ferment lactose (Correct Answer)
- E. Gram-negative, non-flagellated bacteria that ferment lactose
Gut microbiome interactions Explanation: ***Gram-negative, flagellated bacteria that do not ferment lactose***
- The clinical presentation of **bloody diarrhea**, **abdominal pain**, and fever, along with a history of **petting zoo exposure**, strongly suggests a *Campylobacter* infection, which is a **gram-negative, flagellated, curved rod** that does not ferment lactose.
- The growth at **42°C (thermophilic)** and a **positive oxidase test** (indicated by colonies turning black after adding phenylenediamine, an oxidase reagent) are characteristic features of *Campylobacter spp*.
*Gram-positive, anaerobic, rod-shaped bacteria that form spores*
- This description typically refers to organisms like *Clostridium difficile* or *Clostridium perfringens*, which can cause diarrhea.
- However, they are **anaerobic** and would not grow well in typical stool culture conditions without specific anaerobic techniques, nor would they produce a positive oxidase test.
*Gram-positive, aerobic, rod-shaped bacteria that produce catalase*
- This describes organisms like *Listeria monocytogenes* or *Bacillus cereus*.
- While *Listeria* can cause gastrointestinal symptoms, it's less commonly associated with the acute, bloody diarrhea and petting zoo exposure seen here, and *Bacillus cereus* typically causes food poisoning with vomiting.
*Gram-negative, non-flagellated bacteria that do not ferment lactose*
- This description commonly applies to *Shigella spp.*
- While *Shigella* causes **bloody diarrhea** and **abdominal pain**, it is typically **non-motile** (non-flagellated), whereas *Campylobacter* is motile due to its flagella.
*Gram-negative, non-flagellated bacteria that ferment lactose*
- This description would fit organisms like enteropathogenic *E. coli* (EPEC) or enterotoxigenic *E. coli* (ETEC).
- However, the specific growth conditions (thermophilic) and positive oxidase test pointed to by phenylenediamine reactivity are not characteristic of these organisms.
Gut microbiome interactions US Medical PG Question 5: A 42-year-old man with hypertension and type 2 diabetes mellitus is admitted to the hospital because of swelling and redness of the left leg for 3 days. He has chills and malaise. He is treated with intravenous clindamycin for 7 days. On the 8th day at the hospital, he has profuse, foul-smelling, and watery diarrhea. He has nausea and intermittent abdominal cramping. His temperature is 38°C (100.4°F), pulse is 97/min, and blood pressure is 110/78 mm Hg. Bowel sounds are hyperactive. Abdominal examination shows mild tenderness in the left lower quadrant. Rectal examination shows no abnormalities. His hemoglobin concentration is 14.3 g/dL, leukocyte count is 12,300/mm3, and C-reactive protein concentration is 62 mg/L (N=0.08–3.1). After discontinuing clindamycin, which of the following is the most appropriate pharmacotherapy for this patient's condition?
- A. Intravenous vancomycin
- B. Oral fidaxomicin (Correct Answer)
- C. Intravenous metronidazole
- D. Oral metronidazole
- E. Oral rifaximin
Gut microbiome interactions Explanation: ***Oral fidaxomicin***
- The patient's presentation with profuse, foul-smelling, watery diarrhea, abdominal cramping, and fever after prolonged antibiotic use (clindamycin) is highly suggestive of **Clostridioides difficile infection (CDI)**.
- **Oral fidaxomicin** is a first-line agent for initial CDI episodes with **superior efficacy** in reducing recurrence rates compared to metronidazole and similar cure rates to oral vancomycin. It is preferred due to its **narrow spectrum**, **bactericidal activity against C. difficile**, and **minimal disruption to normal colonic flora**.
- Current IDSA/SHEA guidelines recommend fidaxomicin or oral vancomycin as first-line therapy for initial CDI episodes.
*Intravenous vancomycin*
- **Intravenous vancomycin** has poor penetration into the GI tract and is therefore **ineffective for C. difficile infection (CDI)**, which is an intraluminal infection.
- Oral vancomycin is effective for CDI, but intravenous administration will not treat the infection.
*Intravenous metronidazole*
- **Intravenous metronidazole** has limited efficacy in treating **Clostridioides difficile infection (CDI)** as first-line therapy.
- While it achieves some colonic concentration even when given intravenously, oral agents (fidaxomicin or vancomycin) are preferred for initial episodes.
- IV metronidazole may be used as adjunctive therapy in fulminant cases with ileus when oral agents cannot reach the colon.
*Oral metronidazole*
- **Oral metronidazole** was previously used for non-severe CDI but is **no longer recommended as first-line therapy** per updated IDSA/SHEA guidelines due to inferior cure rates and higher recurrence rates compared to vancomycin and fidaxomicin.
- It may be considered only when fidaxomicin and vancomycin are unavailable.
*Oral rifaximin*
- **Oral rifaximin** is sometimes used as **adjunctive therapy following standard treatment** to prevent recurrent C. difficile infection (CDI).
- It is **not recommended as initial monotherapy** for an active CDI episode.
Gut microbiome interactions US Medical PG Question 6: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Gut microbiome interactions Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
Gut microbiome interactions US Medical PG Question 7: A 21-year-old woman comes to the physician because of a 4-day history of abdominal cramps and bloody diarrhea 5 times per day. Her symptoms began after she ate an egg sandwich from a restaurant. Her vital signs are within normal limits. Physical examination shows diffuse abdominal tenderness. Stool culture shows gram-negative rods that produce hydrogen sulfide and do not ferment lactose. Which of the following effects is most likely to occur if she receives antibiotic therapy?
- A. Orange discoloration of bodily fluids
- B. Pruritic maculopapular rash on the extensor surface
- C. Self-limiting systemic inflammatory response
- D. Prolonged fecal excretion of the pathogen (Correct Answer)
- E. Thrombocytopenia and hemolytic anemia
Gut microbiome interactions Explanation: ***Prolonged fecal excretion of the pathogen***
- The patient's symptoms (abdominal cramps, bloody diarrhea after eating an egg sandwich) and stool culture results (gram-negative rods, hydrogen sulfide producers, non-lactose fermenting) are highly suggestive of **Salmonella enterica** infection.
- Antibiotic treatment for non-typhoidal Salmonella gastroenteritis typically **prolongs fecal excretion** and does not shorten the illness, reserving antibiotics for severe cases or immunocompromised individuals.
*Orange discoloration of bodily fluids*
- **Orange discoloration of bodily fluids** (urine, sweat, tears) is a known side effect of **rifampin**, an antibiotic primarily used for tuberculosis and some bacterial meningitides.
- Rifampin is not indicated nor commonly used for Salmonella gastroenteritis.
*Pruritic maculopapular rash on the extensor surface*
- A **pruritic maculopapular rash on the extensor surfaces** is a common presentation of drug reactions, often associated with **penicillins** or **cephalosporins**, especially in viral infections (e.g., amoxicillin rash in mononucleosis).
- This is a general antibiotic side effect and not specifically linked to the outcome of treating Salmonella.
*Self-limiting systemic inflammatory response*
- A self-limiting systemic inflammatory response could be a general reaction to an active infection or a drug, but it's not the most likely or specific outcome of **antibiotic therapy in Salmonella gastroenteritis**.
- Worsening of symptoms can occur in some cases due to toxemia from bacterial lysis (e.g., Jarisch-Herxheimer reaction), but "self-limiting systemic inflammatory response" is too generic for this specific scenario.
*Thrombocytopenia and hemolytic anemia*
- **Thrombocytopenia and hemolytic anemia** in the setting of diarrheal illness strongly suggest **hemolytic uremic syndrome (HUS)**, which is typically associated with **Shiga toxin-producing E. coli** (STEC), particularly E. coli O157:H7.
- While Salmonella can cause severe disease, HUS is not a typical complication of its treatment, and antibiotics are often avoided in STEC infections due to increased risk of HUS.
Gut microbiome interactions US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Gut microbiome interactions Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Gut microbiome interactions US Medical PG Question 9: A 49-year-old man presents to the emergency department with acute onset of pain and redness of the skin of his lower leg for the past 3 days. He has had type 2 diabetes mellitus for the past 12 years, but he is not compliant with his medications. He has smoked 10–15 cigarettes per day for the past 20 years. His temperature is 38°C (100.4°F), pulse is 95/min, and blood pressure is 110/70 mm Hg. On physical examination, the pretibial area is erythematous, edematous, and tender. He is diagnosed with acute cellulitis, and intravenous ceftazidime sodium is started. On the 5th day of antibiotic therapy, the patient complains of severe watery diarrhea, fever, and abdominal tenderness without rigidity. Complete blood count is ordered for the patient and shows 14,000 white blood cells/mm3. Which of the following is the best initial therapy for this patient?
- A. Intravenous vancomycin
- B. Oral ciprofloxacin
- C. Fecal microbiota transplantation
- D. Oral vancomycin (Correct Answer)
- E. Oral metronidazole
Gut microbiome interactions Explanation: ***Oral vancomycin***
- The patient exhibits classic symptoms of **Clostridioides difficile infection (CDI)**: watery diarrhea, fever, abdominal tenderness, and leukocytosis following antibiotic use (ceftazidime). Oral vancomycin is the **first-line therapy** for severe CDI.
- Oral vancomycin achieves high intraluminal concentrations, effectively targeting C. difficile in the colon with minimal systemic absorption.
*Intravenous vancomycin*
- Intravenous vancomycin has **poor penetration** into the gastrointestinal tract and is therefore ineffective for treating C. difficile infection.
- It is primarily used for systemic infections caused by **methicillin-resistant Staphylococcus aureus (MRSA)**.
*Oral ciprofloxacin*
- **Fluoroquinolones** like ciprofloxacin are associated with an increased risk of developing C. difficile infection due to their broad-spectrum activity.
- They are not effective treatments for C. difficile and can potentially worsen the condition or select for resistant strains.
*Fecal microbiota transplantation*
- **Fecal microbiota transplantation (FMT)** is a highly effective treatment for recurrent C. difficile infection, but it is typically reserved for patients who have failed multiple courses of standard antibiotic therapy.
- It is not considered the initial therapy for acute, uncomplicated C. difficile infection.
*Oral metronidazole*
- **Oral metronidazole** was historically used for C. difficile infection but is **no longer recommended** as first-line therapy per current **2021 IDSA/SHEA guidelines** due to inferior clinical outcomes compared to vancomycin or fidaxomicin.
- Given the patient's fever and leukocytosis indicating severe infection, vancomycin is the preferred initial treatment.
Gut microbiome interactions US Medical PG Question 10: A 12-year-old girl is brought to the emergency department 3 hours after the sudden onset of colicky abdominal pain and vomiting. She also has redness and swelling of the face and lips without pruritus. Her symptoms began following a tooth extraction earlier this morning. She had a similar episode of facial swelling after a bicycle accident 1 year ago which resolved within 48 hours without treatment. Vital signs are within normal limits. Examination shows a nontender facial edema, erythema of the oral mucosa, and an enlarged tongue. The abdomen is soft and there is tenderness to palpation over the lower quadrants. An abdominal ultrasound shows segmental thickening of the intestinal wall. Which of the following is the most likely cause of this patient's condition?
- A. T-cell mediated immune reaction
- B. Drug-induced bradykinin excess
- C. Leukotriene overproduction
- D. Immune-complex deposition
- E. Complement inhibitor deficiency (Correct Answer)
Gut microbiome interactions Explanation: ***Complement inhibitor deficiency***
- This patient's presentation with recurrent episodes of **angioedema** (face and lip swelling, enlarged tongue, intestinal wall thickening causing abdominal pain), particularly triggered by **trauma** (tooth extraction, bicycle accident), strongly suggests **hereditary angioedema (HAE)**. HAE is caused by a deficiency or dysfunction of **C1 esterase inhibitor**, a key complement inhibitor.
- A deficiency in C1 esterase inhibitor leads to uncontrolled activation of both the **complement cascade** and the **kallikrein-bradykinin pathway**, resulting in excessive **bradykinin production**, which causes increased vascular permeability and localized edema without urticaria or pruritus.
*T-cell mediated immune reaction*
- **T-cell mediated reactions** are typically associated with **delayed-type hypersensitivity reactions** (e.g., contact dermatitis, graft rejection) and **autoimmune disorders**, which do not fit the acute, recurrent, non-pruritic angioedema seen here.
- These reactions primarily involve cell-mediated cytotoxicity or cytokine release, rather than rapid fluid extravasation due to bradykinin excess.
*Drug-induced bradykinin excess*
- While drug-induced angioedema (e.g., from **ACE inhibitors**) can also cause bradykinin excess, this patient's history of episodes since childhood (after a bicycle accident) and the current exacerbation after a tooth extraction, makes a **hereditary predisposition** much more likely than an isolated drug reaction in a 12-year-old.
- The triggers (trauma, dental procedure) are classic for HAE, which involves an intrinsic defect in bradykinin regulation, not merely an external pharmaceutical cause.
*Leukotriene overproduction*
- **Leukotrienes** are potent mediators involved in **allergic reactions** and **asthma**, contributing to bronchoconstriction, vascular permeability, and inflammation.
- Conditions involving leukotriene overproduction, such as aspirin-exacerbated respiratory disease, typically present with bronchospasm, rhinitis, or urticaria, which are not the primary features here.
*Immune-complex deposition*
- **Immune-complex deposition** is characteristic of conditions like **serum sickness**, **lupus nephritis**, or **vasculitis**, leading to inflammation, fever, rash, and organ damage.
- These conditions do not typically present with isolated, recurrent, non-pruritic angioedema and do not involve the specific mechanism of bradykinin overproduction seen in this patient.
More Gut microbiome interactions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.