GI motility patterns and regulation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GI motility patterns and regulation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GI motility patterns and regulation US Medical PG Question 1: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
GI motility patterns and regulation Explanation: ***Muscarinic (M1)***
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
GI motility patterns and regulation US Medical PG Question 2: A scientist is studying the mechanism by which the gastrointestinal system coordinates the process of food digestion. Specifically, she is interested in how distension of the lower esophagus by a bolus of food changes responses in the downstream segments of the digestive system. She observes that there is a resulting relaxation and opening of the lower esophageal (cardiac) sphincter after the introduction of a food bolus. She also observes a simultaneous relaxation of the orad stomach during this time. Which of the following substances is most likely involved in the process being observed here?
- A. Neuropeptide-Y
- B. Secretin
- C. Ghrelin
- D. Vasoactive intestinal polypeptide (Correct Answer)
- E. Motilin
GI motility patterns and regulation Explanation: ***Vasoactive intestinal polypeptide***
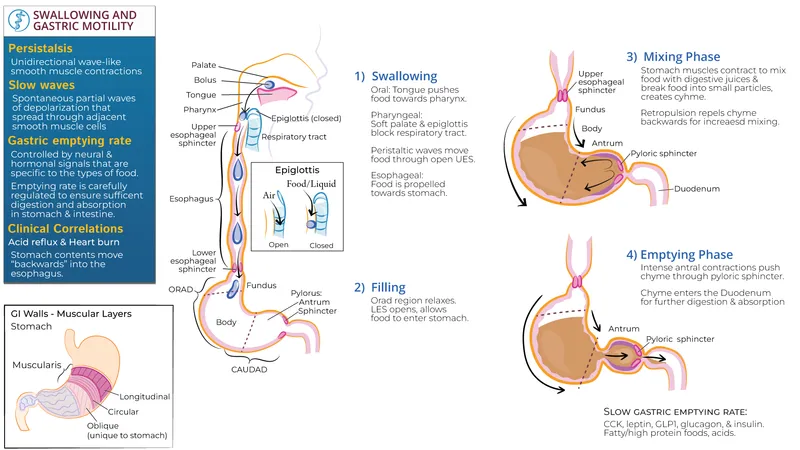
- **VIP (Vasoactive intestinal polypeptide)** is a neuropeptide that mediates **relaxation** of the **smooth muscle** in the gastrointestinal tract, including the **lower esophageal sphincter** and the **orad stomach**, facilitating the passage of food.
- This relaxation is part of the **receptive relaxation** process, allowing the stomach to accommodate food without a significant increase in intragastric pressure.
*Neuropeptide-Y*
- **Neuropeptide-Y (NPY)** is primarily involved in stimulating **food intake** and **reducing energy expenditure**, acting as an orexigenic peptide.
- It does not directly mediate the relaxation of the **lower esophageal sphincter** or **orad stomach** in response to food bolus distension.
*Secretin*
- **Secretin** is a hormone released in response to **acid in the duodenum** and primarily stimulates the pancreas to release **bicarbonate-rich fluid**.
- Its main role is to neutralize stomach acid, not to mediate sphincter relaxation or stomach accommodation.
*Ghrelin*
- **Ghrelin** is known as the "**hunger hormone**" and primarily stimulates **appetite** and **growth hormone release**.
- It does not play a direct role in the relaxation of the **lower esophageal sphincter** or **orad stomach** during swallowing.
*Motilin*
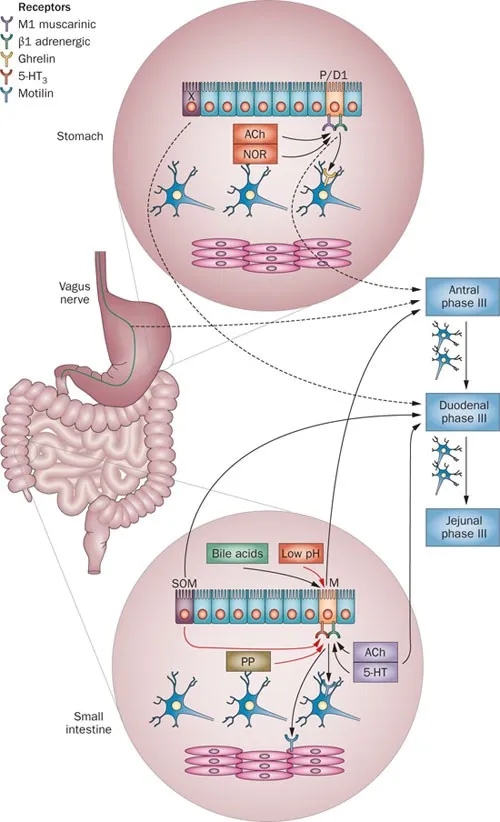
- **Motilin** promotes **gastric and intestinal motility** during the **interdigestive phase**, responsible for the migrating motor complex (MMC).
- Its actions are generally prokinetic, rather than causing relaxation of the upper GI tract in response to a food bolus.
GI motility patterns and regulation US Medical PG Question 3: What is the primary mechanism for iron absorption in the duodenum?
- A. Simple diffusion
- B. Passive paracellular transport
- C. Endocytosis
- D. DMT1 transporter (Correct Answer)
GI motility patterns and regulation Explanation: ***DMT1 transporter***
- The **divalent metal transporter 1 (DMT1)** is the primary mechanism for absorbing **non-heme iron (ferrous iron, Fe2+)** into duodenal enterocytes.
- This active transport process is pH-dependent and drives iron uptake against a concentration gradient.
*Simple diffusion*
- Applies to the movement of substances down their concentration gradient without the aid of membrane proteins, which is not the main mechanism for iron due to its ionic nature.
- While some highly lipid-soluble substances can cross membranes this way, metal ions like iron require specific transporters.
*Passive paracellular transport*
- Involves substances moving *between* cells, rather than *through* them, often occurring in leaky epithelia.
- While some fluid and electrolytes may use this route, it is not the primary or regulated pathway for iron absorption.
*Endocytosis*
- A process where cells engulf substances by forming vesicles from the plasma membrane.
- While some macromolecules are absorbed via endocytosis, it is not the major mechanism for absorbing dietary iron in the duodenum.
GI motility patterns and regulation US Medical PG Question 4: An investigator is developing a drug that selectively inhibits the retrograde axonal transport of rabies virus towards the central nervous system. To achieve this effect, this drug must target which of the following?
- A. Dynein (Correct Answer)
- B. Tubulin
- C. Nidogen
- D. Kinesin
- E. Acetylcholine
GI motility patterns and regulation Explanation: ***Dynein***
- **Dynein** is a microtubule-dependent motor protein responsible for **retrograde axonal transport**, moving cargo (like rabies virus) away from the axon terminals towards the cell body and ultimately the central nervous system.
- Inhibiting dynein would therefore prevent the **rabies virus** from traveling from the site of infection (e.g., muscle cell) to the central nervous system.
*Tubulin*
- **Tubulin** is the primary protein subunit that polymerizes to form **microtubules**, which serve as the tracks for axonal transport.
- Inhibiting tubulin polymerization would disrupt both **anterograde** and **retrograde transport** nonspecifically, leading to severe neurotoxicity rather than selective inhibition of rabies virus transport.
*Nidogen*
- **Nidogen** (also known as entactin) is a glycoprotein component of the **basal lamina**, an extracellular matrix structure.
- It plays a role in cell adhesion and tissue organization but is not directly involved in the intracellular motor processes of axonal transport.
*Kinesin*
- **Kinesin** is a microtubule-dependent motor protein primarily responsible for **anterograde axonal transport**, moving cargo from the cell body towards the axon terminals.
- Inhibiting kinesin would disrupt the outward movement of vesicles and organelles, but would not prevent the **inward retrograde transport** of the rabies virus.
*Acetylcholine*
- **Acetylcholine** is a neurotransmitter that plays a role in synaptic transmission in both the peripheral and central nervous systems.
- While rabies virus can affect neuronal function, acetylcholine itself is not a motor protein or a structural component directly involved in the physical process of **axonal transport**.
GI motility patterns and regulation US Medical PG Question 5: A 68-year-old man comes to the physician because of headache, fatigue, and nonproductive cough for 1 week. He appears pale. Pulmonary examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 9.5 g/dL and an elevated serum lactate dehydrogenase concentration. A peripheral blood smear shows normal red blood cells that are clumped together. Results of cold agglutinin titer testing show a 4-fold elevation above normal. An x-ray of the chest shows diffuse, patchy infiltrates bilaterally. Treatment is begun with an antibiotic that is also used to promote gut motility. Which of the following is the primary mechanism of action of this drug?
- A. Inhibition of bacterial RNA polymerase
- B. Inhibition of folic acid synthesis
- C. Free radical creation within bacterial cells
- D. Inhibition of transpeptidase cross-linking at the cell wall
- E. Inhibition of peptide translocation at the 50S ribosomal subunit (Correct Answer)
GI motility patterns and regulation Explanation: ***Inhibition of peptide translocation at the 50S ribosomal subunit***
- This drug described is likely **erythromycin** or another **macrolide antibiotic**, which inhibits bacterial protein synthesis by binding to the **50S ribosomal subunit** and preventing translocation.
- Macrolides are used to treat **atypical pneumonia** caused by *Mycoplasma pneumoniae*, which is indicated by the patient's symptoms (headache, fatigue, nonproductive cough, bilateral patchy infiltrates) and **cold agglutinin disease**.
*Inhibition of bacterial RNA polymerase*
- This is the mechanism of action of **rifampin**, which is primarily used for **tuberculosis** and **meningitis prophylaxis**, not for atypical pneumonia.
- Rifampin's side effects and spectrum of activity do not align with the implied clinical scenario, especially the gut motility promotion.
*Inhibition of folic acid synthesis*
- This is the mechanism for **sulfonamides** and **trimethoprim**, which are bacteriostatic and target different pathogens than those causing cold agglutinin positive pneumonia.
- These drugs are not known for promoting gut motility.
*Free radical creation within bacterial cells*
- This mechanism is characteristic of **metronidazole**, an antibiotic used for anaerobic bacterial and parasitic infections.
- Metronidazole does not fit the clinical context of atypical pneumonia with cold agglutinins, nor is it a macrolide that promotes gut motility.
*Inhibition of transpeptidase cross-linking at the cell wall*
- This describes the mechanism of **beta-lactam antibiotics** (e.g., penicillins, cephalosporins), which are ineffective against **atypical pneumonia** because *Mycoplasma* lacks a cell wall.
- Beta-lactams do not typically promote gut motility.
GI motility patterns and regulation US Medical PG Question 6: Which neurotransmitter primarily mediates slow synaptic transmission in the enteric nervous system?
- A. Substance P
- B. Serotonin
- C. Acetylcholine
- D. Nitric oxide (Correct Answer)
GI motility patterns and regulation Explanation: **Nitric oxide**
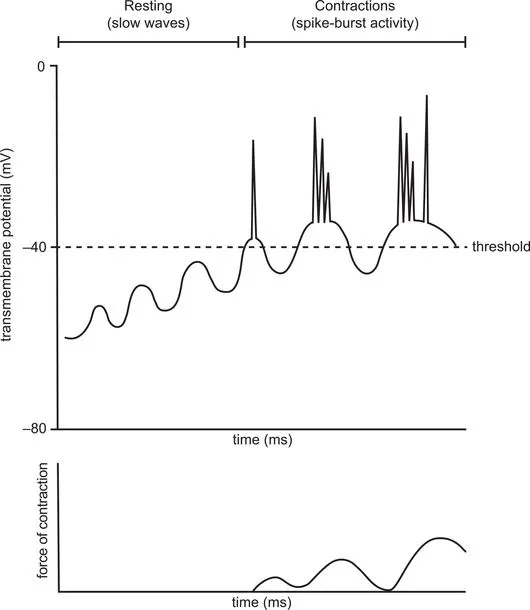
- **Nitric oxide (NO)** is a key **non-classical neurotransmitter** in the **enteric nervous system (ENS)**, mediating **slow synaptic transmission** due to its gaseous nature allowing for diffusion and longer-lasting effects.
- It is involved in **smooth muscle relaxation**, **vasodilation**, and diverse gastrointestinal functions, including **peristalsis** and **sphincter relaxation**.
*Substance P*
- **Substance P** is a **neuropeptide** that acts as an **excitatory neurotransmitter** in the ENS, primarily mediating **fast synaptic transmission** and smooth muscle contraction.
- It is involved in pain perception, inflammation, and is released by sensory neurons and some enteric neurons.
*Serotonin*
- **Serotonin (5-HT)** is a major neurotransmitter in the ENS, largely mediating **fast excitatory or inhibitory synaptic transmission** depending on the receptor subtype.
- It plays a crucial role in regulating gut motility, secretion, and visceral sensation, and is involved in both rapid signaling and neuromodulation.
*Acetylcholine*
- **Acetylcholine (ACh)** is the primary **excitatory neurotransmitter** of the **parasympathetic nervous system** within the ENS, mediating **fast synaptic transmission** by binding to nicotinic and muscarinic receptors.
- It is crucial for stimulating **smooth muscle contraction** (promoting peristalsis), increasing glandular secretions, and generally enhancing gut motility.
GI motility patterns and regulation US Medical PG Question 7: A 2-day-old newborn boy has failed to pass meconium after 48 hours. There is an absence of stool in the rectal vault. Family history is significant for MEN2A syndrome. Which of the following confirms the diagnosis?
- A. Barium enema demonstrating absence of a transition zone
- B. Atrophic nerve fibers and increased acetylcholinesterase activity
- C. Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum
- D. Genetic testing confirming mutation in the RET oncogene
- E. Absence of ganglion cells demonstrated by rectal suction biopsy (Correct Answer)
GI motility patterns and regulation Explanation: ***Absence of ganglion cells demonstrated by rectal suction biopsy***
- The **absence of ganglion cells** in the colorectum, particularly on a **rectal suction biopsy**, is the definitive diagnostic feature of **Hirschsprung disease**.
- This congenital condition is characterized by the **failure of neural crest cells to migrate** to the distal bowel, leading to an aganglionic segment that cannot relax, resulting in functional obstruction.
*Barium enema demonstrating absence of a transition zone*
- A **barium enema** is a useful initial imaging study for suspected **Hirschsprung disease**, often showing a **transition zone** between a constricted aganglionic segment and a dilated, normally innervated proximal bowel.
- The *absence* of a transition zone would make **Hirschsprung disease** *less likely* or could indicate **total colonic aganglionosis**, but it is not a direct confirmatory diagnostic finding and still requires biopsy.
*Atrophic nerve fibers and increased acetylcholinesterase activity*
- While increased **acetylcholinesterase activity** in hypertrophied nerve fibers is a characteristic finding in the muscularis mucosa and submucosa of aganglionic segments in **Hirschsprung disease**, the description of "*atrophic* nerve fibers" is incorrect.
- The abnormal nerve fibers are typically hypertrophic, and this finding from specialized staining on a biopsy supports the diagnosis but is not the primary confirmatory feature itself; the **absence of ganglion cells** is paramount.
*Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum*
- **Rectal manometry** is used to assess the neuromuscular function of the rectum and anal sphincter. In **Hirschsprung disease**, there is a characteristic **failure of the internal anal sphincter to relax** when the rectum is distended.
- Demonstrating normal *relaxation* of the internal anal sphincter would effectively *rule out* **Hirschsprung disease**, as the **failure of relaxation** is a key physiological abnormality.
*Genetic testing confirming mutation in the RET oncogene*
- Mutations in the **RET oncogene** are associated with **Hirschsprung disease**, especially in familial cases and those associated with syndromic forms like **MEN2A**.
- While a positive genetic test can support the diagnosis and guide genetic counseling, it is **not sufficient for a definitive diagnosis** on its own, as penetrance is variable and the definitive diagnosis relies on histological confirmation of aganglionosis.
GI motility patterns and regulation US Medical PG Question 8: A 57-year-old male is found to have an elevated prostate specific antigen (PSA) level on screening labwork. PSA may be elevated in prostate cancer, benign prostatic hypertrophy (BPH), or prostatitis. Which of the following best describes the physiologic function of PSA?
- A. Regulation of transcription factors and phosphorylation of proteins
- B. Maintains corpus luteum
- C. Response to peritoneal irritation
- D. Sperm production
- E. Liquefaction of semen (Correct Answer)
GI motility patterns and regulation Explanation: ***Liquefaction of semen***
- Prostate-specific antigen (PSA) is a **serine protease** produced by the epithelial cells of the prostate gland.
- Its primary physiological role is to **liquefy the seminal coagulum** formed after ejaculation, allowing sperm to become motile and navigate the female reproductive tract.
*Regulation of transcription factors and phosphorylation of proteins*
- This function is characteristic of **kinases** and **phosphatases**, which are involved in intracellular signaling pathways.
- While essential for cellular function, it does not describe the specific role of PSA.
*Maintains corpus luteum*
- The maintenance of the corpus luteum is primarily the role of **luteinizing hormone (LH)** and, in pregnancy, **human chorionic gonadotropin (hCG)**.
- These hormones are involved in the female reproductive cycle, unrelated to PSA.
*Response to peritoneal irritation*
- Peritoneal irritation triggers an inflammatory response involving various immune cells and mediators, but not specifically PSA.
- PSA itself is not directly involved in the systemic or local response to peritoneal inflammation.
*Sperm production*
- **Sperm production (spermatogenesis)** occurs in the seminiferous tubules of the testes under the influence of hormones like FSH and testosterone.
- While semen is the vehicle for sperm, PSA's role is in the post-ejaculatory processing of semen, not in the initial production of sperm.
GI motility patterns and regulation US Medical PG Question 9: A 24-year-old man comes to the physician with his wife because of difficulty conceiving during the past year. He emigrated from rural Romania 2 years ago and has a history of recurrent respiratory infections since childhood for which he has not sought treatment. Physical examination shows mild hepatomegaly and clubbing of the nail beds. Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels are increased. Microscopic analysis of centrifuged seminal fluid shows no sperm cells. This patient's condition is most likely caused by impaired function of a channel protein that normally opens in response to binding of which of the following?
- A. Cyclic guanosine monophosphate
- B. γ-aminobutyric acid
- C. Cyclic adenosine monophosphate (cAMP) (Correct Answer)
- D. N-methyl-D-aspartate
- E. Dynein
GI motility patterns and regulation Explanation: ***Cyclic adenosine monophosphate (cAMP)***
- This patient presents with **infertility** (azoospermia), **recurrent respiratory infections**, **hepatomegaly**, and **elevated liver enzymes**, which are highly suggestive of **cystic fibrosis**.
- **Cystic fibrosis** is caused by mutations in the **CFTR gene**, which encodes a **chloride channel protein** that is activated by **cAMP-dependent protein kinase A phosphorylation**.
*Cyclic guanosine monophosphate*
- **Cyclic GMP (cGMP)** is involved in the activation of certain **ion channels**, notably in **phototransduction** and the regulation of **vascular tone** via nitric oxide signaling.
- It does not directly regulate the chloride channels implicated in cystic fibrosis.
*γ-aminobutyric acid*
- **GABA** is the primary **inhibitory neurotransmitter** in the central nervous system, acting on **ligand-gated chloride channels** (GABA-A receptors) and G-protein coupled receptors (GABA-B receptors).
- Its function is unrelated to the **CFTR chloride channel** or the pathophysiology of cystic fibrosis.
*N-methyl-D-aspartate*
- **NMDA receptors** are a type of **glutamate receptor** that are **ligand-gated ion channels** permeable to calcium, sodium, and potassium, crucial for synaptic plasticity and learning.
- They are not involved in the function of the **CFTR protein** or the manifestations of cystic fibrosis.
*Dynein*
- **Dynein** is a **motor protein** responsible for the movement of **cilia and flagella**, and defects in dynein are associated with **primary ciliary dyskinesia (PCD)**.
- While PCD can cause recurrent respiratory infections and infertility due to immotile sperm, the hepatomegaly and elevated liver enzymes point more strongly towards **cystic fibrosis**, where the defect is in a **channel protein** regulated by cAMP, not a motor protein.
GI motility patterns and regulation US Medical PG Question 10: A 32-year-old woman patient presents to her family physician with recurrent retrosternal chest pain. She has had similar episodes for the past 7 months along with difficulty swallowing solid as well as liquid food. She recently completed an 8-week course of a proton pump inhibitor, but she is still bothered by the feeling that food gets stuck down her 'food pipe'. Her pain is not related to exertion. She denies any history of acid reflux disease. Her blood pressure is 125/81 mm Hg, respirations are 21/min, pulse is 78/min, and temperature is 36.7°C (98.1°F). She currently does not have pain. A barium swallow X-ray image is normal. Which of the following tests would aid in the diagnosis of this patient's condition?
- A. Electrocardiogram
- B. Upper GI endoscopy
- C. Manometry (Correct Answer)
- D. Injection of botulinum toxin
- E. Additional therapy with proton pump inhibitors
GI motility patterns and regulation Explanation: ***Manometry***
- The patient's symptoms of **recurrent retrosternal chest pain** and **dysphagia for both solids and liquids** suggest a **motility disorder** of the esophagus, such as **achalasia** or **diffuse esophageal spasm**.
- **Esophageal manometry** directly measures the pressure and coordination of muscle contractions in the esophagus, identifying abnormalities in peristalsis and sphincter relaxation.
*Electrocardiogram*
- While chest pain can be cardiac in origin, the patient's symptoms are primarily related to **swallowing** and not exertion, making a primary cardiac cause less likely.
- An ECG would be unable to diagnose an **esophageal motility disorder**.
*Upper GI endoscopy*
- An **upper GI endoscopy** is primarily used to visualize the mucosa of the esophagus, stomach, and duodenum to detect structural abnormalities, inflammation, or ulcers.
- It would likely be normal in a pure **motility disorder** and would not provide functional information about esophageal contractions.
*Injection of botulinum toxin*
- **Botulinum toxin injection** is a treatment option for some esophageal motility disorders (e.g., achalasia), but it is not a diagnostic test.
- It works by paralyzing muscles, thereby reducing lower esophageal sphincter pressure.
*Additional therapy with proton pump inhibitors*
- The patient has already completed an 8-week course of a **PPI** without improvement, and she explicitly denies a history of **acid reflux disease**.
- This suggests that her symptoms are unlikely to be acid-related, making further PPI therapy ineffective for diagnosis or treatment.
More GI motility patterns and regulation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.