Gastrointestinal hormones US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gastrointestinal hormones. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gastrointestinal hormones US Medical PG Question 1: A scientist is studying the mechanism by which the gastrointestinal system coordinates the process of food digestion. Specifically, she is interested in how distension of the lower esophagus by a bolus of food changes responses in the downstream segments of the digestive system. She observes that there is a resulting relaxation and opening of the lower esophageal (cardiac) sphincter after the introduction of a food bolus. She also observes a simultaneous relaxation of the orad stomach during this time. Which of the following substances is most likely involved in the process being observed here?
- A. Neuropeptide-Y
- B. Secretin
- C. Ghrelin
- D. Vasoactive intestinal polypeptide (Correct Answer)
- E. Motilin
Gastrointestinal hormones Explanation: ***Vasoactive intestinal polypeptide***
- **VIP (Vasoactive intestinal polypeptide)** is a neuropeptide that mediates **relaxation** of the **smooth muscle** in the gastrointestinal tract, including the **lower esophageal sphincter** and the **orad stomach**, facilitating the passage of food.
- This relaxation is part of the **receptive relaxation** process, allowing the stomach to accommodate food without a significant increase in intragastric pressure.
*Neuropeptide-Y*
- **Neuropeptide-Y (NPY)** is primarily involved in stimulating **food intake** and **reducing energy expenditure**, acting as an orexigenic peptide.
- It does not directly mediate the relaxation of the **lower esophageal sphincter** or **orad stomach** in response to food bolus distension.
*Secretin*
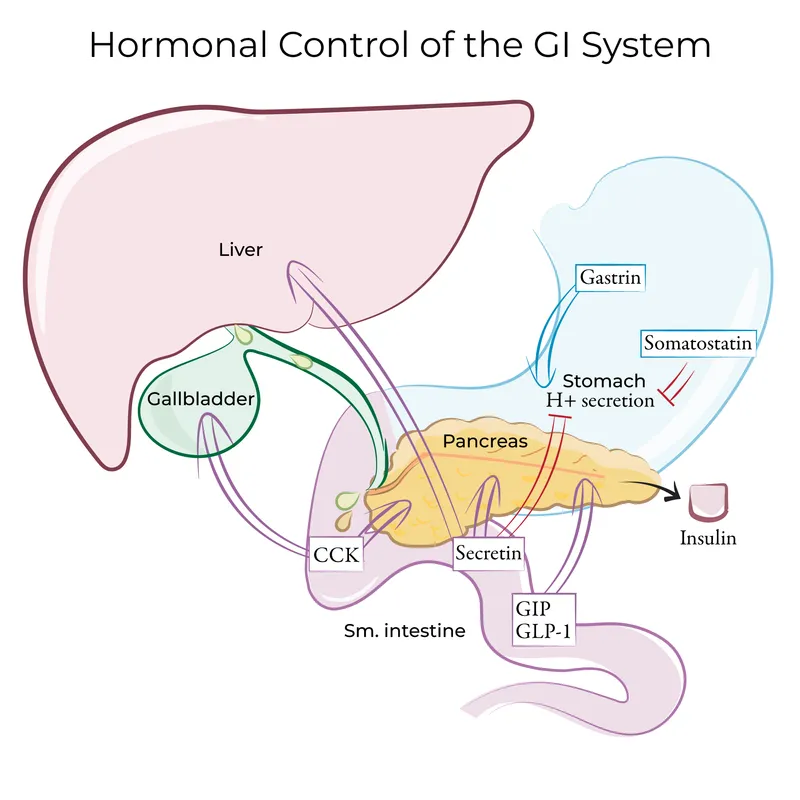
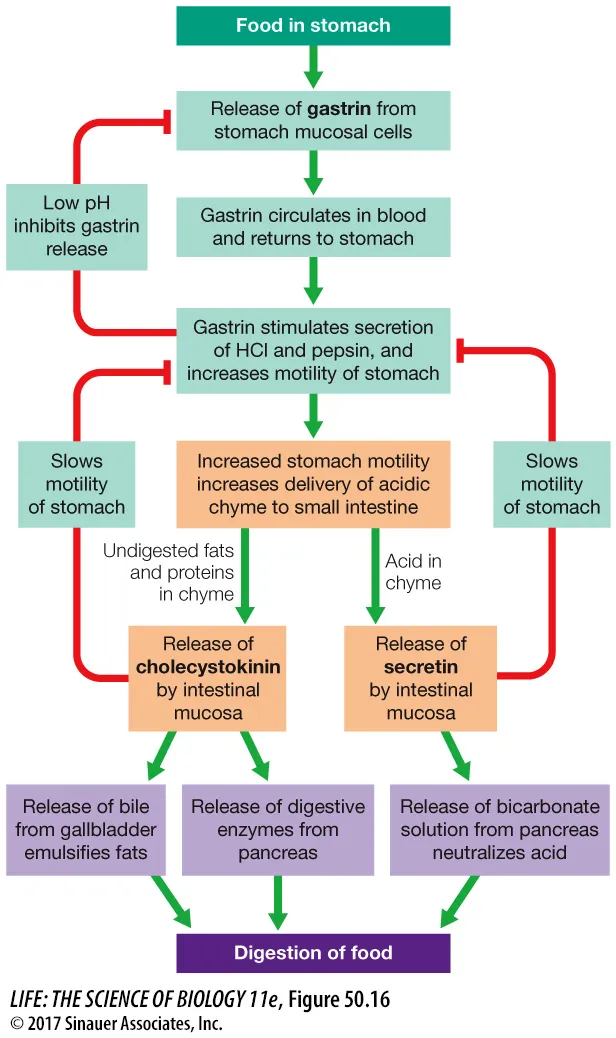
- **Secretin** is a hormone released in response to **acid in the duodenum** and primarily stimulates the pancreas to release **bicarbonate-rich fluid**.
- Its main role is to neutralize stomach acid, not to mediate sphincter relaxation or stomach accommodation.
*Ghrelin*
- **Ghrelin** is known as the "**hunger hormone**" and primarily stimulates **appetite** and **growth hormone release**.
- It does not play a direct role in the relaxation of the **lower esophageal sphincter** or **orad stomach** during swallowing.
*Motilin*
- **Motilin** promotes **gastric and intestinal motility** during the **interdigestive phase**, responsible for the migrating motor complex (MMC).
- Its actions are generally prokinetic, rather than causing relaxation of the upper GI tract in response to a food bolus.
Gastrointestinal hormones US Medical PG Question 2: Nine healthy subjects participate in a study of gastric secretions. Subjects are asked to eat a meal at hour 0, at which time the pH of stomach contents and rate of stomach acid secretions are measured over the next 4 hours. Results of the study are shown. Which of the following mediators is most active at point A in the graph?
- A. Secretin
- B. Acetylcholine (Correct Answer)
- C. Prostaglandin
- D. Glucose-dependent insulinotropic peptide
- E. Somatostatin
Gastrointestinal hormones Explanation: ***Acetylcholine***
- At point A, the **pH is low** and the **rate of stomach acid secretion is high**, indicating a robust post-meal response for digestion.
- **Acetylcholine** is a primary neurocrine stimulant of gastric acid secretion, acting both directly on parietal cells and indirectly by stimulating histamine release, making it highly active during increased acid output.
*Secretin*
- **Secretin** primarily acts to *inhibit* gastric acid secretion and stimulate bicarbonate and fluid secretion from the pancreas and liver, particularly in response to low pH in the duodenum.
- It would be *less active* during a phase of high gastric acid secretion, as its main role is to neutralize acid after it leaves the stomach.
*Prostaglandin*
- **Prostaglandins (e.g., PGE2)** play a *cytoprotective role* in the stomach, inhibiting acid secretion and increasing mucus and bicarbonate production.
- Their activity would *reduce* the rate of stomach acid secretion, which is contrary to the high secretion rate observed at point A.
*Glucose-dependent insulinotropic peptide*
- **Glucose-dependent insulinotropic peptide (GIP)** primarily stimulates **insulin release** from pancreatic β-cells in response to ingested glucose and fat.
- While it has slight *inhibitory effects* on gastric acid secretion, its main role is metabolic, not directly related to the observed high acid secretion or low pH.
*Somatostatin*
- **Somatostatin** is a potent *inhibitor* of gastric acid secretion, acting directly on parietal cells and indirectly by inhibiting the release of histamine and gastrin.
- Therefore, it would be *less active* during a period of high gastric acid secretion, as its function is to suppress such activity.
Gastrointestinal hormones US Medical PG Question 3: A 49-year-old male complains of heartburn, epigastric pain, and diarrhea. He has a past medical history significant for heartburn that is nonresponsive to omeprazole. He denies any alcohol intake, and has not been taking any nonsteroidal anti-inflammatory drugs. An endoscopy is performed, which shows two ulcers in the proximal duodenum, and one in the distal third of the duodenum. Which of the following is most likely true about this patient’s current condition?
- A. Chronic atrophic gastritis would decrease the suspected hormone level
- B. Secretin administration would suppress the release of the suspected hormone in this patient
- C. Parietal cell hypertrophy is likely present (Correct Answer)
- D. The suspected hormone acts via a receptor tyrosine kinase signaling pathway
- E. Increasing omeprazole dose will likely decrease the suspected hormone level
Gastrointestinal hormones Explanation: ***Parietal cell hypertrophy is likely present***
- The patient's symptoms (refractory heartburn, epigastric pain, diarrhea, and multiple duodenal ulcers, including distal ones) are highly suggestive of **Zollinger-Ellison syndrome (ZES)**, caused by a gastrinoma.
- **Gastrinomas** overproduce gastrin, which leads to **parietal cell hyperplasia and hypertrophy** due to its trophic effects and excessive acid secretion. This results in the observed multiple, refractory ulcers.
*Chronic atrophic gastritis would decrease the suspected hormone level*
- **Chronic atrophic gastritis** typically causes a *decrease* in gastric acid production due to glandular atrophy and loss of parietal cells.
- This reduction in acid secretion would lead to an *increase* in gastrin release as a feedback mechanism, trying to stimulate acid production, not a decrease.
*Secretin administration would suppress the release of the suspected hormone in this patient*
- In healthy individuals, **secretin** *inhibits* gastrin release from G cells, but in patients with **gastrinomas**, secretin paradoxically *stimulates* gastrin release.
- A positive secretin stimulation test (rise in gastrin levels after secretin administration) is a diagnostic hallmark for gastrinoma.
*The suspected hormone acts via a receptor tyrosine kinase signaling pathway*
- The suspected hormone, **gastrin**, exerts its effects primarily by binding to the **cholecystokinin B (CCK2) receptor**, which is a **G protein-coupled receptor (GPCR)**.
- Activation of this GPCR leads to increased intracellular calcium and protein kinase C activity, not a receptor tyrosine kinase pathway.
*Increasing omeprazole dose will likely decrease the suspected hormone level*
- While omeprazole *reduces acid secretion* and may alleviate symptoms, it does so by inhibiting the proton pump in parietal cells.
- Reducing acid output through omeprazole would *increase* gastrin release via a feedback loop, as the body tries to compensate for the perceived lack of acid, rather than decreasing gastrin levels in ZES patients.
Gastrointestinal hormones US Medical PG Question 4: A 57-year-old male presents to his primary care physician with upper abdominal pain. He reports a 3-month history of mild epigastric pain that improves with meals. He has lost 15 pounds since his symptoms started. His past medical history is notable for gynecomastia in the setting of a prolactinoma for which he underwent surgical resection over 10 years prior. He has a 15-pack-year smoking history, a history of heroin abuse, and is on methadone. His family history is notable for parathyroid adenoma in his father. His temperature is 98.8°F (37.1°C), blood pressure is 125/80 mmHg, pulse is 78/min, and respirations are 18/min. This patient’s symptoms are most likely due to elevations in a substance with which of the following functions?
- A. Promote gastric mucosal growth
- B. Increase pancreatic bicarbonate secretion
- C. Decrease gastrin secretion
- D. Increase pancreatic exocrine secretion
- E. Increase gastric acid secretion (Correct Answer)
Gastrointestinal hormones Explanation: ***Increase gastric acid secretion***
- The patient's history of a prolactinoma, family history of parathyroid adenoma, and current symptoms suggest **Multiple Endocrine Neoplasia type 1 (MEN1)**.
- **MEN1** often involves **pancreatic neuroendocrine tumors**, specifically **gastrinomas**, which autonomously secrete **gastrin**, leading to **Zollinger-Ellison syndrome (ZES)**.
- **Gastrin's primary function** is to stimulate **parietal cells** in the gastric mucosa to secrete **hydrochloric acid (HCl)**, leading to **massive gastric acid hypersecretion**.
- This acid hypersecretion causes **severe peptic ulcer disease** (explaining the epigastric pain), **refractory ulcers**, and often **diarrhea** from acid overload in the small intestine.
*Promote gastric mucosal growth*
- While gastrin does have a **trophic effect** on gastric mucosa (promoting mucosal growth), this is a **secondary/chronic effect**, not the primary pathophysiologic mechanism.
- The acute symptoms (epigastric pain, ulcers, weight loss) are directly caused by **acid hypersecretion**, not mucosal growth.
- In clinical practice, the focus in Zollinger-Ellison syndrome is on managing the **acid hypersecretion** with high-dose proton pump inhibitors.
*Increase pancreatic bicarbonate secretion*
- **Secretin** is the primary hormone responsible for increasing pancreatic bicarbonate secretion in response to duodenal acidification.
- Gastrin does not significantly affect pancreatic bicarbonate secretion.
*Decrease gastrin secretion*
- This is incorrect; the problem in gastrinomas is **autonomous hypersecretion of gastrin**.
- Normally, low gastric pH inhibits gastrin release via negative feedback, but gastrinomas secrete gastrin autonomously, independent of feedback mechanisms.
*Increase pancreatic exocrine secretion*
- **Cholecystokinin (CCK)** is the primary hormone that stimulates pancreatic enzyme secretion.
- While the excessive acid entering the duodenum in ZES may indirectly stimulate pancreatic secretion, gastrin itself does not directly increase pancreatic exocrine secretion significantly.
Gastrointestinal hormones US Medical PG Question 5: An investigator is studying gastric secretions in human volunteers. Measurements of gastric activity are recorded after electrical stimulation of the vagus nerve. Which of the following sets of changes is most likely to occur after vagus nerve stimulation?
$$$ Somatostatin secretion %%% Gastrin secretion %%% Gastric pH $$$
- A. ↓ ↓ ↓
- B. ↑ ↓ ↑
- C. ↓ ↑ ↓ (Correct Answer)
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Gastrointestinal hormones Explanation: ***↓ ↑ ↓***
- Vagal stimulation directly promotes **gastrin release** from G cells, which in turn stimulates **acid secretion**.
- Increased acid secretion **decreases gastric pH** and a lower pH **inhibits somatostatin secretion** in a negative feedback loop.
*↓ ↓ ↓*
- This option incorrectly suggests that vagal stimulation would **decrease gastrin secretion**. Vagal stimulation is a primary stimulant for gastrin release.
- A decrease in gastrin would lead to less acid, resulting in a **higher gastric pH**, not a lower one.
*↑ ↓ ↑*
- This suggests an **increase in somatostatin** and a **decrease in gastrin** which is contrary to the direct effects of vagal stimulation.
- Furthermore, a decreased gastrin would lead to **higher pH**, not lower, unless acid secretion was independently inhibited, which is not the case here.
*↑ ↑ ↑*
- This option correctly indicates an **increase in gastrin secretion** but
incorrectly suggests an **increase in somatostatin** and an **increase in gastric pH**.
- Increased gastrin leads to **increased acid** and thus a **decreased pH**, while high acid levels inhibit somatostatin.
*↑ ↑ ↓*
- This sequence correctly shows an **increase in gastrin** and a **decrease in pH**, but incorrectly suggests an **increase in somatostatin**.
- Somatostatin secretion would be **inhibited** by the increased acid levels resulting from vagal stimulation and gastrin release.
Gastrointestinal hormones US Medical PG Question 6: A 39-year-old woman presents to her primary care physician because she has been experiencing intermittent abdominal pain for the last 2 weeks. She says that the pain is squeezing in nature, is located in the right upper quadrant, and is particularly severe after eating a meal. After a diagnosis is made, the patient asks why the pain gets worse after eating. The physician explains that food is detected by the gastrointestinal tract through numerous receptors and that this information is transmitted to other parts of the body to cause compensatory changes. The neurons responsible for transmitting this information are most likely located in a layer of the intestine that has which of the following characteristics?
- A. Contracts to generate local movement in mucosa
- B. Contains cells that primarily absorb nutrients
- C. Connective tissue that envelops the other layers
- D. Contracts to generate peristaltic waves (Correct Answer)
- E. Contains large blood vessels and large lymphatic vessels
Gastrointestinal hormones Explanation: ***Contracts to generate peristaltic waves***
- This describes the **muscularis propria** (external muscle layer), which contains the **myenteric plexus (Auerbach's plexus)** between its inner circular and outer longitudinal smooth muscle layers.
- The **myenteric plexus is the primary neural network** responsible for detecting food through mechanoreceptors and chemoreceptors, transmitting sensory information, and coordinating both local reflexes and systemic compensatory responses throughout the gastrointestinal tract.
- These neurons communicate with the **autonomic nervous system** and coordinate the release of hormones like **cholecystokinin (CCK)** after eating, which causes gallbladder contraction (relevant to this patient's postprandial pain from cholecystitis).
- While this layer's most obvious function is generating peristalsis, it contains the most extensive enteric nervous system network for sensory integration and motor coordination.
*Contains large blood vessels and large lymphatic vessels*
- This describes the **submucosa**, which contains the **submucosal plexus (Meissner's plexus)**.
- While the submucosal plexus does contain sensory neurons, it primarily regulates **local functions** such as mucosal secretion, absorption, and blood flow rather than the broader systemic compensatory responses described in the question.
- The submucosa's neural network is more limited compared to the myenteric plexus.
*Contracts to generate local movement in mucosa*
- This describes the **muscularis mucosae**, a thin layer of smooth muscle within the mucosa that causes local folding and movement of the mucosal surface.
- This layer lacks significant neural plexuses and is not involved in transmitting sensory information for systemic responses.
*Contains cells that primarily absorb nutrients*
- This refers to the **mucosa**, specifically the epithelial cells lining the intestinal surface.
- While the mucosa contains chemoreceptors and mechanoreceptors, the question asks about the neurons that **transmit** this information, which are located in the deeper neural plexuses (primarily myenteric), not in the absorptive epithelium itself.
*Connective tissue that envelops the other layers*
- This describes the **serosa** (or adventitia), the outermost protective layer.
- The serosa contains minimal neural tissue and is not involved in sensory detection or transmission of gastrointestinal information.
Gastrointestinal hormones US Medical PG Question 7: During a study on gastrointestinal hormones, a volunteer is administered the hormone secreted by S cells. Which of the following changes most likely represent the effect of this hormone on gastric and duodenal secretions?
$$$ Gastric H+ %%% Duodenal HCO3- %%% Duodenal Cl- $$$
- A. ↓ ↓ ↓
- B. ↑ ↓ no change
- C. ↑ ↑ ↓
- D. ↓ ↑ ↓ (Correct Answer)
- E. ↓ no change no change
Gastrointestinal hormones Explanation: ***↓ ↑ ↓***
- S cells secrete **secretin**, which primarily inhibits **gastric acid (H+) secretion** to protect the duodenal mucosa from acidic chyme.
- Secretin also stimulates the pancreas and bile ducts to secrete **bicarbonate (HCO3-)**, neutralizing the acidic chyme. Duodenal **chloride (Cl-) secretion is typically reduced** as it is often exchanged for bicarbonate or water follows bicarbonate secretion for osmotic balance.
*↓ ↓ ↓*
- While **gastric H+ decreases** due to secretin, **duodenal HCO3- secretion increases**, not decreases, making this option incorrect.
- **Duodenal Cl- secretion** would likely decrease, but the other components are inconsistent with secretin's effects.
*↑ ↓ no change*
- Secretin **inhibits gastric H+ secretion**, so an increase contradicts its primary function to protect the duodenum from acid.
- **Duodenal HCO3- secretion increases**, not decreases, and no change in Cl- is unlikely given the physiological responses to secretin.
*↑ ↑ ↓*
- Secretin **inhibits gastric H+ secretion**, so an increase is incorrect.
- While **duodenal HCO3- increases** and **Cl- decreases**, the initial change in gastric H+ makes this option wrong.
*↓ no change no change*
- While **gastric H+ is indeed decreased**, secretin significantly **increases duodenal HCO3- secretion** and likely decreases duodenal Cl- secretion, making "no change" in these parameters incorrect.
- Secretin has a pronounced effect on both bicarbonate and chloride transport in the duodenum.
Gastrointestinal hormones US Medical PG Question 8: Which of the following cells in the body depends on dynein for its unique functioning?
- A. Small intestinal mucosal cell
- B. Skeletal muscle cell
- C. Adipocyte
- D. Lower esophageal mucosal cell
- E. Fallopian tube mucosal cell (Correct Answer)
Gastrointestinal hormones Explanation: ***Fallopian tube mucosal cell***
- Dynein is a **motor protein** that facilitates the movement of **cilia** along microtubules.
- The ciliary action in fallopian tube mucosal cells is crucial for **transporting the ovum** from the ovary to the uterus.
*Small intestinal mucosal cell*
- These cells primarily depend on **microvilli** for absorption, which are actin-based structures and do not directly involve dynein for their primary function of absorption.
- While they have some cilia, their unique and defining function is nutrient absorption, not movement dependent on dynein.
*Skeletal muscle cell*
- Skeletal muscle cells rely on the interaction of **actin and myosin** filaments for **contraction**.
- Dynein is not directly involved in the mechanism of muscle contraction.
*Adipocyte*
- Adipocytes are specialized in **lipid storage** and release, a process that does not involve dynein.
- Their unique function does not depend on intracellular or extracellular movement facilitated by dynein.
*Lower esophageal mucosal cell*
- These cells primarily provide a **protective barrier** against gastric acid reflux.
- Their function involves **stratified squamous epithelium** and mucus production, not ciliary movement dependent on dynein.
Gastrointestinal hormones US Medical PG Question 9: A 50-year-old woman with long-standing diabetes presents with severe, watery diarrhea that wakes her at night. Stool studies show normal osmotic gap and negative stool cultures. Colonoscopy is normal. Trial of fasting does not improve diarrhea. Gastric emptying study shows delayed emptying. What neurotransmitter deficiency in the enteric nervous system best explains both her gastric and colonic dysmotility?
- A. Acetylcholine
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Substance P
- E. Vasoactive intestinal peptide
Gastrointestinal hormones Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is the primary **inhibitory neurotransmitter** in the enteric nervous system responsible for mediating **receptive relaxation** of the stomach and smooth muscle inhibition during peristalsis.
- In **diabetic autonomic neuropathy**, loss of nitrergic neurons leads to **gastroparesis** (failed pyloric relaxation) and **diabetic diarrhea** due to uncoordinated colonic motility and loss of descending inhibition.
*Acetylcholine*
- **Acetylcholine** is the primary **excitatory neurotransmitter** responsible for muscle contraction; a deficiency would likely lead to paralytic ileus rather than secretory-pattern diarrhea.
- Though diabetic neuropathy affects cholinergic fibers, the hallmark of the inhibitory dysmotility seen in **gastroparesis** is specifically linked to the NO pathway.
*Serotonin*
- **Serotonin (5-HT)** is predominantly involved in the initiation of the **peristaltic reflex** and intestinal secretion via enterochromaffin cells.
- While 5-HT levels can be altered in IBS, it is not the classic neurotransmitter deficiency cited for the specific combination of **delayed gastric emptying** and autonomic diarrhea in diabetics.
*Substance P*
- **Substance P** acts as a **co-transmitter** with acetylcholine to promote smooth muscle contraction and pain transmission.
- Deficiency of Substance P would impair motor activity but does not explain the loss of **inhibitory control** and relaxation necessary for normal gastric emptying.
*Vasoactive intestinal peptide*
- **Vasoactive intestinal peptide (VIP)** is an inhibitory neurotransmitter that promotes intestinal secretion and smooth muscle relaxation.
- While VIP is involved in relaxation, **Nitric oxide** is considered the more critical mediator for the **pyloric and fundal relaxation** that is specifically impaired in diabetic gastropathy.
Gastrointestinal hormones US Medical PG Question 10: A 25-year-old man undergoes extensive small bowel resection following trauma, leaving 40 cm of jejunum anastomosed to the ascending colon. The ileocecal valve is removed. Six months postoperatively, he requires total parenteral nutrition. Despite this, he develops calcium oxalate kidney stones. Evaluate the mechanism linking his intestinal resection to nephrolithiasis.
- A. Decreased urinary citrate from chronic metabolic acidosis
- B. Hyperparathyroidism from vitamin D malabsorption causing hypercalciuria
- C. Increased colonic absorption of oxalate due to enhanced permeability from bile salts
- D. Dehydration from chronic diarrhea concentrating urinary oxalate
- E. Increased enteric oxalate absorption from calcium binding to malabsorbed fatty acids (Correct Answer)
Gastrointestinal hormones Explanation: ***Increased enteric oxalate absorption from calcium binding to malabsorbed fatty acids***
- In **short bowel syndrome**, unabsorbed **fatty acids** in the gut compete with oxalate by binding to **calcium**, forming calcium soaps.
- This leaves **oxalate** free and unbound in the intestinal lumen, significantly increasing its absorption in the **intact colon**, leading to **enteric hyperoxaluria**.
*Decreased urinary citrate from chronic metabolic acidosis*
- While **hypocitraturia** is a risk factor for stones due to diarrhea-induced metabolic acidosis, it is not the primary mechanism of **enteric hyperoxaluria** following fat malabsorption.
- **Citrate** normally inhibits stone formation by binding calcium, but its absence does not explain the high levels of **urinary oxalate** seen in these patients.
*Hyperparathyroidism from vitamin D malabsorption causing hypercalciuria*
- Vitamin D malabsorption typically leads to **hypocalciuria**, as the body attempts to conserve calcium due to low levels and **secondary hyperparathyroidism**.
- Stone formation in this context is driven by high **oxalate excretion**, not by high calcium levels in the urine.
*Increased colonic absorption of oxalate due to enhanced permeability from bile salts*
- While unabsorbed **bile salts** can irritate the colonic mucosa and slightly increase permeability, this is a secondary phenomenon.
- The fundamental metabolic driver for stone formation is the **loss of calcium-oxalate binding** in the lumen due to fat malabsorption.
*Dehydration from chronic diarrhea concentrating urinary oxalate*
- Chronic diarrhea causes **low urine volume**, which concentrates all solutes, but this is a non-specific factor for all stone types.
- The specific development of **calcium oxalate stones** in this patient is uniquely tied to the **malabsorptive biochemistry** resulting from the loss of the ileum.
More Gastrointestinal hormones US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.