Defecation reflex US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Defecation reflex. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Defecation reflex US Medical PG Question 1: A 32-year-old woman presents to the office with complaints of intense anal pain every time she has a bowel movement. The pain has been present for the past 4 weeks, and it is dull and throbbing in nature. It is associated with mild bright red bleeding from the rectum that is aggravated during defecation. She has no relevant past medical history. When asked about her sexual history, she reports practicing anal intercourse. The vital signs include heart rate 98/min, respiratory rate 16/min, temperature 37.6°C (99.7°F), and blood pressure 110/66 mm Hg. On physical examination, the anal sphincter tone is markedly increased, and it's impossible to introduce the finger due to severe pain. What is the most likely diagnosis?
- A. Local anal trauma (Correct Answer)
- B. Rectal prolapse and paradoxical contraction of the puborectalis muscle
- C. Inflammatory bowel disease
- D. Anorectal abscess
- E. Hemorrhoidal disease
Defecation reflex Explanation: ***Local anal trauma***
- The patient's history of **anal intercourse**, severe **anal pain** during bowel movements, **bright red bleeding**, and a markedly **increased anal sphincter tone** with inability to perform a DRE due to pain are highly indicative of an **anal fissure** caused by local trauma.
- The dull, throbbing pain suggests associated spasm of the internal anal sphincter, a common complication of anal fissures.
*Rectal prolapse and paradoxical contraction of the puborectalis muscle*
- **Rectal prolapse** typically presents with a sensation of a mass protruding from the anus and difficulty with bowel movements, not usually intense, sharp pain and bright red bleeding.
- **Paradoxical contraction of the puborectalis muscle** (anismus) causes difficult defecation and straining but is not typically associated with acute, severe pain and bright red bleeding as primary symptoms.
*Inflammatory bowel disease*
- While IBD can cause rectal bleeding and anal pain (e.g., in Crohn's disease with perianal fistulas or fissures), the presentation here is acute and highly suggestive of a mechanical cause, without other systemic symptoms of IBD like diarrhea, weight loss, or abdominal pain.
- The **isolated acute anal pain** and bleeding linked to defecation and anal intercourse are less typical for an initial presentation of IBD without other associated symptoms.
*Anorectal abscess*
- Anorectal abscesses typically present with severe, constant, throbbing **perianal pain** that is often worse when sitting, and may be accompanied by fever, chills, and localized swelling or erythema, which are not described here.
- While an abscess might cause throbbing pain, the association with **defecation-induced pain** and **bright red bleeding** from a visible source like an anal fissure is less characteristic.
*Hemorrhoidal disease*
- Hemorrhoids often cause **painless bright red bleeding** during defecation or can cause itching and discomfort. **Thrombosed external hemorrhoids** can cause acute, severe pain but usually present with a palpable, tender nodule.
- The description of **intense, sharp anal pain** during bowel movements, increased sphincter tone, and inability to perform a digital rectal exam are more consistent with an anal fissure than typical hemorrhoidal disease.
Defecation reflex US Medical PG Question 2: A 45-year-old woman comes to the office with a 2-week history of rectal bleeding that occurs every day with her bowel movements. She denies any pain during defecation. Apart from this, she does not have any other complaints. Her past medical history is insignificant except for 5 normal vaginal deliveries. Her vitals are a heart rate of 72/min, a respiratory rate of 15/min, a temperature of 36.7°C (98.1°F), and a blood pressure of 115/85 mm Hg. On rectovaginal examination, there is a palpable, non-tender, prolapsed mass that can be pushed back by the examiner's finger into the anal sphincter. What is the most likely diagnosis?
- A. Rectal ulcer
- B. Anal fissure
- C. Hemorrhoids (Correct Answer)
- D. Proctitis
- E. Anorectal fistula
Defecation reflex Explanation: ***Hemorrhoids***
- The presentation of **painless rectal bleeding** with bowel movements and a **palpable, prolapsed, reducible mass** is classic for hemorrhoids, especially common in multiparous women.
- The absence of pain and the ability to reduce the prolapsed mass are key differentiating features from other perianal conditions.
*Rectal ulcer*
- Rectal ulcers typically present with **painful defecation** and may cause blood in the stool, but are not usually associated with a reducible prolapsed mass.
- They are often associated with other inflammatory conditions or trauma, which are not described here.
*Anal fissure*
- Anal fissures are characterized by **severe pain during and after defecation** due to a tear in the anal canal lining, and the bleeding is usually bright red and minimal.
- The primary symptom is pain, which this patient explicitly denies.
*Proctitis*
- Proctitis involves **inflammation of the rectal lining**, leading to symptoms like tenesmus, urgency, and bloody or purulent discharge, often with abdominal pain.
- It does not typically present with a palpable, prolapsed, reducible anal mass.
*Anorectal fistula*
- Anorectal fistulas are abnormal tracts between the anal canal or rectum and the perianal skin, usually causing **pain, swelling, and purulent discharge**.
- While bleeding can occur, the primary symptom is drainage, and they do not present as a reducible prolapsed mass.
Defecation reflex US Medical PG Question 3: A 3-day-old newborn is brought to the physician because of abdominal distention, inconsolable crying, and 3 episodes of bilious vomiting since the previous evening. He was delivered at home at 40 weeks' gestation by a trained midwife. He has not passed meconium. Physical examination shows abdominal distention, a tight anal sphincter, and an explosive passage of air and feces on removal of the examining finger. Abnormal development of which of the following best explains this patient's condition?
- A. Submucosa and muscularis externa (Correct Answer)
- B. Epithelium and submucosa
- C. Muscularis mucosae and lamina propria
- D. Muscularis mucosae and serosa
- E. Epithelium and lamina propria
Defecation reflex Explanation: ***Submucosa and muscularis externa***
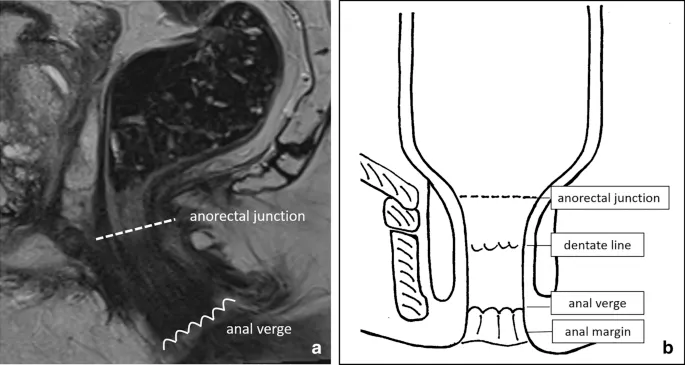
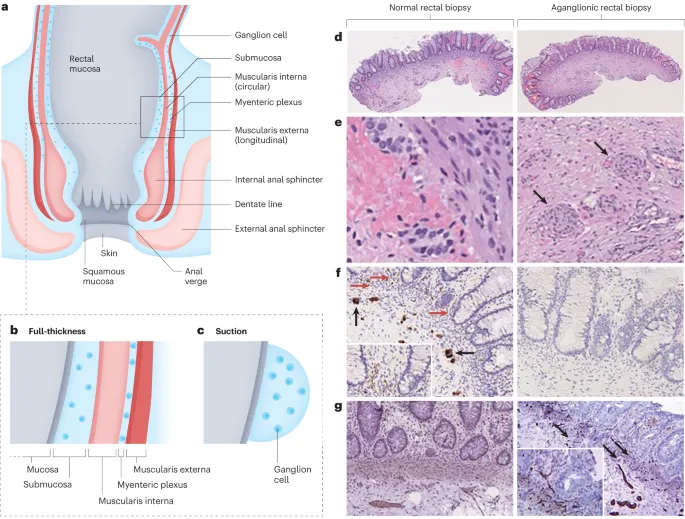
- This patient's symptoms (abdominal distention, bilious vomiting, failure to pass meconium, tight anal sphincter with explosive stool passage) are classic for **Hirschsprung disease**.
- Hirschsprung disease is characterized by the absence of **ganglion cells** in the myenteric (Auerbach's) plexus (located between the inner circular and outer longitudinal layers of the muscularis externa) and the submucosal (Meissner's) plexus (located in the submucosa) of the distal colon.
*Epithelium and submucosa*
- The **epithelium** is involved in absorption and secretion, and its primary dysfunction would typically lead to diarrhea or malabsorption, not an obstructive picture like this.
- While the submucosa contains Meissner's plexus, the lack of ganglion cells in the muscularis externa's Auerbach's plexus is equally crucial to the pathophysiology of Hirschsprung disease.
*Muscularis mucosae and lamina propria*
- The **muscularis mucosae** is a thin layer that causes folding of the mucosa, while the **lamina propria** is connective tissue supporting the epithelium; neither is directly implicated in the primary pathology of Hirschsprung disease which involves neural crest cell migration.
- Absence of ganglion cells in these layers would not explain the severe motility disorder observed in Hirschsprung disease involving the entire bowel wall.
*Muscularis mucosae and serosa*
- The **serosa** is the outermost connective tissue layer and is not directly involved in the intrinsic innervation or motility problems seen in Hirschsprung disease.
- Dysfunction of the muscularis mucosae alone would not result in the functional obstruction due to absent peristalsis.
*Epithelium and lamina propria*
- The **epithelium** and **lamina propria** are primarily involved in the digestive and absorptive functions of the gut, and their abnormal development would not typically cause the characteristic features of Hirschsprung disease, which is a neurodevelopmental disorder of the gut.
- The core issue in Hirschsprung disease lies in the neural plexuses controlling motility, not the mucosal lining.
Defecation reflex US Medical PG Question 4: A 2-year-old boy is brought in to his pediatrician for a routine checkup. The parents mention that the child has been developing appropriately, although they have been noticing that the child appears to have chronic constipation. The parents report that their child does not routinely have daily bowel movements, and they have noticed that his abdomen has become more distended recently. In the past, they report that the patient was also delayed in passing meconium, but this was not further worked up. On exam, his temperature is 98.6°F (37.0°C), blood pressure is 110/68 mmHg, pulse is 74/min, and respirations are 14/min. The patient is noted to have a slightly distended abdomen that is nontender. Eventually, this patient undergoes a biopsy. Which of the following layers most likely reveals the causative pathologic finding of this disease?
- A. Submucosa
- B. Mucosa
- C. Lamina propria
- D. Muscularis mucosa
- E. Muscularis propria (between muscle layers) (Correct Answer)
Defecation reflex Explanation: ***Muscularis propria (between muscle layers)***
- This patient's presentation with **chronic constipation**, **abdominal distention**, and **delayed meconium passage** is highly suggestive of **Hirschsprung disease**.
- The causative pathology in Hirschsprung disease is the **absence of ganglion cells** in the **myenteric (Auerbach's) and submucosal (Meissner's) plexuses**, which is definitively diagnosed by a rectal biopsy showing this lack of innervation.
- The **myenteric plexus** is located **between the inner circular and outer longitudinal layers** of the **muscularis propria**, making this the primary layer examined for diagnostic findings.
*Submucosa*
- While the **submucosal (Meissner's) plexus** is also affected in Hirschsprung disease and the submucosa can show absent ganglion cells, the **myenteric plexus** in the muscularis propria is the primary diagnostic target in rectal biopsies.
- Both plexuses are affected, but the muscularis propria is considered the most definitive layer for diagnosis.
*Mucosa*
- The **mucosa** is the innermost layer of the gastrointestinal tract, consisting of epithelium, lamina propria, and muscularis mucosa.
- This layer does **not** contain the enteric nervous system plexuses (myenteric or submucosal) responsible for gut motility, so biopsy of this layer alone would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
*Lamina propria*
- The **lamina propria** is a thin layer of connective tissue found within the **mucosa**, beneath the epithelium.
- This layer primarily contains blood vessels, lymphatics, and immune cells, and it is **not** where the ganglion cells of the enteric nervous system are located or where the primary pathology of Hirschsprung disease is found.
*Muscularis mucosa*
- The **muscularis mucosa** is a thin layer of smooth muscle that forms the outermost layer of the **mucosa**.
- It does not contain the enteric plexuses (myenteric or submucosal) responsible for gut motility, so its biopsy would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
Defecation reflex US Medical PG Question 5: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Defecation reflex Explanation: ***S3–S4 nerve roots***
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Defecation reflex US Medical PG Question 6: A 2-day-old newborn boy has failed to pass meconium after 48 hours. There is an absence of stool in the rectal vault. Family history is significant for MEN2A syndrome. Which of the following confirms the diagnosis?
- A. Barium enema demonstrating absence of a transition zone
- B. Atrophic nerve fibers and increased acetylcholinesterase activity
- C. Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum
- D. Genetic testing confirming mutation in the RET oncogene
- E. Absence of ganglion cells demonstrated by rectal suction biopsy (Correct Answer)
Defecation reflex Explanation: ***Absence of ganglion cells demonstrated by rectal suction biopsy***
- The **absence of ganglion cells** in the colorectum, particularly on a **rectal suction biopsy**, is the definitive diagnostic feature of **Hirschsprung disease**.
- This congenital condition is characterized by the **failure of neural crest cells to migrate** to the distal bowel, leading to an aganglionic segment that cannot relax, resulting in functional obstruction.
*Barium enema demonstrating absence of a transition zone*
- A **barium enema** is a useful initial imaging study for suspected **Hirschsprung disease**, often showing a **transition zone** between a constricted aganglionic segment and a dilated, normally innervated proximal bowel.
- The *absence* of a transition zone would make **Hirschsprung disease** *less likely* or could indicate **total colonic aganglionosis**, but it is not a direct confirmatory diagnostic finding and still requires biopsy.
*Atrophic nerve fibers and increased acetylcholinesterase activity*
- While increased **acetylcholinesterase activity** in hypertrophied nerve fibers is a characteristic finding in the muscularis mucosa and submucosa of aganglionic segments in **Hirschsprung disease**, the description of "*atrophic* nerve fibers" is incorrect.
- The abnormal nerve fibers are typically hypertrophic, and this finding from specialized staining on a biopsy supports the diagnosis but is not the primary confirmatory feature itself; the **absence of ganglion cells** is paramount.
*Rectal manometry demonstrating relaxation of the internal anal sphincter with distension of the rectum*
- **Rectal manometry** is used to assess the neuromuscular function of the rectum and anal sphincter. In **Hirschsprung disease**, there is a characteristic **failure of the internal anal sphincter to relax** when the rectum is distended.
- Demonstrating normal *relaxation* of the internal anal sphincter would effectively *rule out* **Hirschsprung disease**, as the **failure of relaxation** is a key physiological abnormality.
*Genetic testing confirming mutation in the RET oncogene*
- Mutations in the **RET oncogene** are associated with **Hirschsprung disease**, especially in familial cases and those associated with syndromic forms like **MEN2A**.
- While a positive genetic test can support the diagnosis and guide genetic counseling, it is **not sufficient for a definitive diagnosis** on its own, as penetrance is variable and the definitive diagnosis relies on histological confirmation of aganglionosis.
Defecation reflex US Medical PG Question 7: Which mechanism primarily regulates sodium reabsorption in the collecting duct?
- A. Glomerulotubular balance
- B. Atrial natriuretic peptide
- C. Antidiuretic hormone
- D. Aldosterone (Correct Answer)
Defecation reflex Explanation: ***Aldosterone***
- **Aldosterone** is the primary hormone that stimulates **sodium reabsorption** and **potassium secretion** in the principal cells of the collecting duct.
- It acts by increasing the synthesis and activity of **ENaC channels** on the apical membrane and **Na+/K+-ATPase pumps** on the basolateral membrane.
*Glomerulotubular balance*
- **Glomerulotubular balance** refers to the mechanism by which the **proximal tubule** reabsorbs a constant fraction of the filtered load, regardless of changes in glomerular filtration rate (GFR).
- This mechanism maintains a relatively constant delivery of fluid and solutes to downstream segments but does not primarily regulate sodium in the collecting duct.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** primarily **inhibits sodium reabsorption** in the collecting duct, leading to **natriuresis** and **diuresis**, which is the opposite of sodium reabsorption.
- ANP is released in response to atrial stretch, indicating increased blood volume.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)** primarily regulates **water reabsorption** in the collecting duct by increasing the insertion of **aquaporin-2 channels** into the apical membrane, making the collecting duct permeable to water.
- While ADH can indirectly affect sodium concentration by influencing water movement, it does not directly regulate sodium transport to the same extent as aldosterone.
Defecation reflex US Medical PG Question 8: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Defecation reflex Explanation: ***Glossopharyngeal***
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
Defecation reflex US Medical PG Question 9: A 50-year-old woman with long-standing diabetes presents with severe, watery diarrhea that wakes her at night. Stool studies show normal osmotic gap and negative stool cultures. Colonoscopy is normal. Trial of fasting does not improve diarrhea. Gastric emptying study shows delayed emptying. What neurotransmitter deficiency in the enteric nervous system best explains both her gastric and colonic dysmotility?
- A. Acetylcholine
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Substance P
- E. Vasoactive intestinal peptide
Defecation reflex Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is the primary **inhibitory neurotransmitter** in the enteric nervous system responsible for mediating **receptive relaxation** of the stomach and smooth muscle inhibition during peristalsis.
- In **diabetic autonomic neuropathy**, loss of nitrergic neurons leads to **gastroparesis** (failed pyloric relaxation) and **diabetic diarrhea** due to uncoordinated colonic motility and loss of descending inhibition.
*Acetylcholine*
- **Acetylcholine** is the primary **excitatory neurotransmitter** responsible for muscle contraction; a deficiency would likely lead to paralytic ileus rather than secretory-pattern diarrhea.
- Though diabetic neuropathy affects cholinergic fibers, the hallmark of the inhibitory dysmotility seen in **gastroparesis** is specifically linked to the NO pathway.
*Serotonin*
- **Serotonin (5-HT)** is predominantly involved in the initiation of the **peristaltic reflex** and intestinal secretion via enterochromaffin cells.
- While 5-HT levels can be altered in IBS, it is not the classic neurotransmitter deficiency cited for the specific combination of **delayed gastric emptying** and autonomic diarrhea in diabetics.
*Substance P*
- **Substance P** acts as a **co-transmitter** with acetylcholine to promote smooth muscle contraction and pain transmission.
- Deficiency of Substance P would impair motor activity but does not explain the loss of **inhibitory control** and relaxation necessary for normal gastric emptying.
*Vasoactive intestinal peptide*
- **Vasoactive intestinal peptide (VIP)** is an inhibitory neurotransmitter that promotes intestinal secretion and smooth muscle relaxation.
- While VIP is involved in relaxation, **Nitric oxide** is considered the more critical mediator for the **pyloric and fundal relaxation** that is specifically impaired in diabetic gastropathy.
Defecation reflex US Medical PG Question 10: A 25-year-old man undergoes extensive small bowel resection following trauma, leaving 40 cm of jejunum anastomosed to the ascending colon. The ileocecal valve is removed. Six months postoperatively, he requires total parenteral nutrition. Despite this, he develops calcium oxalate kidney stones. Evaluate the mechanism linking his intestinal resection to nephrolithiasis.
- A. Decreased urinary citrate from chronic metabolic acidosis
- B. Hyperparathyroidism from vitamin D malabsorption causing hypercalciuria
- C. Increased colonic absorption of oxalate due to enhanced permeability from bile salts
- D. Dehydration from chronic diarrhea concentrating urinary oxalate
- E. Increased enteric oxalate absorption from calcium binding to malabsorbed fatty acids (Correct Answer)
Defecation reflex Explanation: ***Increased enteric oxalate absorption from calcium binding to malabsorbed fatty acids***
- In **short bowel syndrome**, unabsorbed **fatty acids** in the gut compete with oxalate by binding to **calcium**, forming calcium soaps.
- This leaves **oxalate** free and unbound in the intestinal lumen, significantly increasing its absorption in the **intact colon**, leading to **enteric hyperoxaluria**.
*Decreased urinary citrate from chronic metabolic acidosis*
- While **hypocitraturia** is a risk factor for stones due to diarrhea-induced metabolic acidosis, it is not the primary mechanism of **enteric hyperoxaluria** following fat malabsorption.
- **Citrate** normally inhibits stone formation by binding calcium, but its absence does not explain the high levels of **urinary oxalate** seen in these patients.
*Hyperparathyroidism from vitamin D malabsorption causing hypercalciuria*
- Vitamin D malabsorption typically leads to **hypocalciuria**, as the body attempts to conserve calcium due to low levels and **secondary hyperparathyroidism**.
- Stone formation in this context is driven by high **oxalate excretion**, not by high calcium levels in the urine.
*Increased colonic absorption of oxalate due to enhanced permeability from bile salts*
- While unabsorbed **bile salts** can irritate the colonic mucosa and slightly increase permeability, this is a secondary phenomenon.
- The fundamental metabolic driver for stone formation is the **loss of calcium-oxalate binding** in the lumen due to fat malabsorption.
*Dehydration from chronic diarrhea concentrating urinary oxalate*
- Chronic diarrhea causes **low urine volume**, which concentrates all solutes, but this is a non-specific factor for all stone types.
- The specific development of **calcium oxalate stones** in this patient is uniquely tied to the **malabsorptive biochemistry** resulting from the loss of the ileum.
More Defecation reflex US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.