Carbohydrate digestion and absorption US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Carbohydrate digestion and absorption. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Carbohydrate digestion and absorption US Medical PG Question 1: A 45-year-old man is brought to the emergency department by ambulance after vomiting blood. The patient reports that he only ate a small snack the morning before and had not eaten anything for over 24 hours. At the hospital, the patient is stabilized. He is admitted to a surgical floor and placed on NPO with a nasogastric tube set to intermittent suction. He has been previously diagnosed with liver cirrhosis. An esophagogastroduodenoscopy (EGD) has been planned for the next afternoon. At the time of endoscopy, some pathways were generating glucose to maintain serum glucose levels. Which of the following enzymes catalyzes the irreversible biochemical reaction of this process?
- A. Glucose-6-phosphate dehydrogenase
- B. Glycogen phosphorylase
- C. Enolase
- D. Glyceraldehyde-3-phosphate dehydrogenase
- E. Fructose-1,6-bisphosphatase (Correct Answer)
Carbohydrate digestion and absorption Explanation: ***Fructose-1,6-bisphosphatase***
- The scenario describes a patient in a fasting state for over 24 hours, during which **gluconeogenesis** is crucial for maintaining blood glucose levels.
- **Fructose-1,6-bisphosphatase** is one of the key regulatory enzymes in gluconeogenesis, catalyzing an **irreversible reaction** that bypasses the phosphofructokinase-1 step of glycolysis.
*Glucose-6-phosphate dehydrogenase*
- This enzyme is involved in the **pentose phosphate pathway**, which generates NADPH and precursors for nucleotide synthesis.
- It does not directly participate in gluconeogenesis to produce glucose from non-carbohydrate sources.
*Glycogen phosphorylase*
- This enzyme is involved in **glycogenolysis**, the breakdown of glycogen into glucose-1-phosphate.
- While it releases glucose, the body's glycogen stores would likely be depleted after over 24 hours of fasting, making gluconeogenesis the primary pathway for glucose production.
*Enolase*
- Enolase is an enzyme in the glycolytic pathway, catalyzing the reversible conversion of 2-phosphoglycerate to phosphoenolpyruvate.
- It is not an enzyme of gluconeogenesis, nor does it catalyze an irreversible step in the glucose production process during fasting.
*Glyceraldehyde-3-phosphate dehydrogenase*
- This enzyme is also part of glycolysis, catalyzing the reversible oxidation and phosphorylation of glyceraldehyde-3-phosphate to 1,3-bisphosphoglycerate.
- Like enolase, it is not an irreversible enzyme in gluconeogenesis that would be generating glucose under fasting conditions.
Carbohydrate digestion and absorption US Medical PG Question 2: A 3-week-old male is brought to the emergency department because of increasing lethargy. He was born at home without prenatal care or neonatal screening and appeared to be normal at birth. Despite this, his parents noticed that he would vomit after breastfeeding. He then progressively became more lethargic and began to have a few episodes of diarrhea after feeding. His parents do not recall any significant family history and neither of his siblings have had similar symptoms. Upon presentation, the infant is found to be generally unresponsive with mild hepatomegaly. Physical exam further reveals signs of clouding in the lenses of his eyes bilaterally. The levels of which of the following metabolites will be most dramatically elevated in this patient?
- A. Fructose
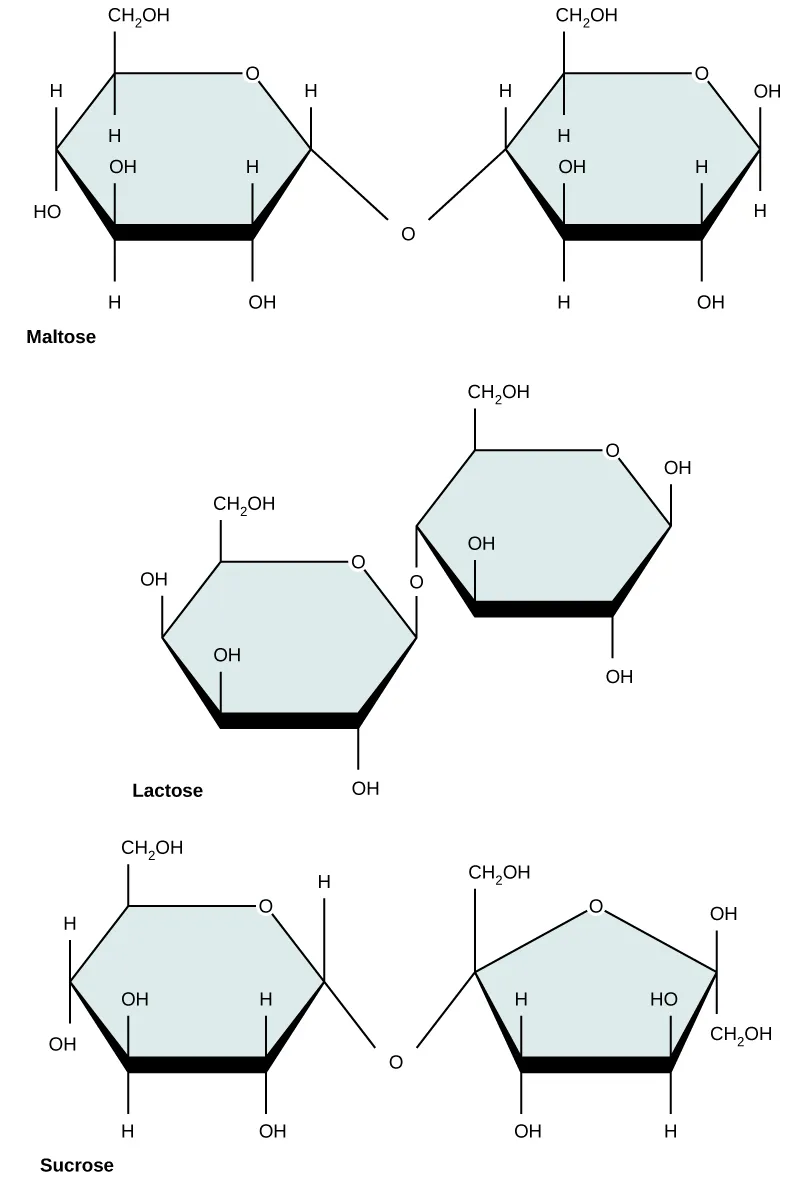
- B. Lactose
- C. Galactose
- D. Galactose-1-phosphate (Correct Answer)
- E. Fructose-1-phosphate
Carbohydrate digestion and absorption Explanation: ***Galactose-1-phosphate***
- This patient's presentation with **vomiting after breastfeeding**, progressive **lethargy**, hepatomegaly, and **bilateral cataracts** is highly suggestive of **classic galactosemia**. This autosomal recessive disorder results from a deficiency in **galactose-1-phosphate uridylyltransferase (GALT)**.
- The deficiency of GALT leads to an accumulation of **galactose-1-phosphate** in various tissues, causing toxicity to the liver, brain, and eyes.
*Fructose*
- **Fructose intolerance** (hereditary fructose intolerance) is caused by a deficiency of **aldolase B**, leading to the accumulation of **fructose-1-phosphate**.
- While it can cause similar symptoms like vomiting, lethargy, and hepatomegaly, it is typically triggered by **fructose ingestion** (fruits, sucrose), which is not the primary carbohydrate source for a 3-week-old exclusively fed breast milk (containing lactose).
*Lactose*
- **Lactose intolerance** is due to a deficiency of lactase, leading to the malabsorption of lactose.
- Symptoms are primarily gastrointestinal, including **diarrhea, bloating, and abdominal pain**, but do not typically involve severe lethargy, hepatomegaly, or cataracts. The unmetabolized lactose itself does not accumulate to toxic levels.
*Galactose*
- While galactose is the substrate for the deficient enzyme in galactosemia, the most dramatically elevated and toxic metabolite is **galactose-1-phosphate**, not free galactose.
- Galactose is converted to galactose-1-phosphate before the metabolic block occurs.
*Fructose-1-phosphate*
- As mentioned, this metabolite accumulates in **hereditary fructose intolerance**, not galactosemia.
- The combination of breastfeeding and cataracts points strongly to a disorder of galactose metabolism rather than fructose metabolism.
Carbohydrate digestion and absorption US Medical PG Question 3: A 3-week-old newborn is brought to the pediatrician by his mother. His mother is concerned about her son’s irritability and vomiting, particularly after breastfeeding him. The infant was born at 39 weeks via spontaneous vaginal delivery. His initial physical was benign. Today the newborn appears mildly jaundiced with palpable hepatomegaly, and his eyes appear cloudy, consistent with the development of cataracts. The newborn is also in the lower weight-age percentile. The physician considers a hereditary enzyme deficiency and orders blood work and a urinalysis to confirm his diagnosis. He recommends that milk and foods high in galactose and/or lactose be eliminated from the diet. Which of the following is the most likely deficient enzyme in this metabolic disorder?
- A. Aldose reductase
- B. Galactose-1-phosphate uridyl transferase (Correct Answer)
- C. UDP-galactose-4-epimerase
- D. Galactokinase
- E. Glucose-6-phosphate dehydrogenase
Carbohydrate digestion and absorption Explanation: ***Galactose-1-phosphate uridyl transferase***
- The constellation of symptoms including **vomiting**, **irritability**, **jaundice**, **hepatomegaly**, **cataracts**, and **failure to thrive** in a neonate, with improvement upon eliminating galactose/lactose from the diet, is highly characteristic of **classic galactosemia**.
- **Classic galactosemia** is caused by a deficiency in **galactose-1-phosphate uridyl transferase (GALT)**, leading to the accumulation of galactose-1-phosphate, which is toxic to various tissues.
*Aldose reductase*
- This enzyme converts galactose to **galactitol**, which can accumulate in the lens and cause **cataracts** in all forms of galactosemia if left untreated.
- However, isolated aldose reductase deficiency does not explain the full spectrum of severe systemic symptoms like hepatomegaly, jaundice, and failure to thrive observed in this neonate, which are indicative of classic galactosemia.
*UDP-galactose-4-epimerase*
- Deficiency in **UDP-galactose-4-epimerase (GALE)**, also known as epimerase deficiency galactosemia, has a wide range of severity.
- While it can present with similar symptoms to GALT deficiency, its severe form is rarer, and the classic, pronounced presentation described here is more commonly associated with GALT deficiency.
*Galactokinase*
- Deficiency in **galactokinase (GALK)** causes **Type II galactosemia**, which primarily manifests as **cataracts** due to galactitol accumulation.
- It typically does not present with the severe hepatic (jaundice, hepatomegaly) or systemic symptoms (vomiting, failure to thrive) seen in classic galactosemia.
*Glucose-6-phosphate dehydrogenase*
- **Glucose-6-phosphate dehydrogenase (G6PD) deficiency** primarily causes **hemolytic anemia** triggered by certain drugs, infections, or fava beans.
- It does not present with the specific constellation of symptoms related to galactose metabolism, such as cataracts, hepatomegaly, and vomiting upon milk ingestion, as described in this case.
Carbohydrate digestion and absorption US Medical PG Question 4: A 54-year-old man presents to his primary care physician with a 2-month-history of diarrhea. He says that he feels the urge to defecate 3-4 times per day and that his stools have changed in character since the diarrhea began. Specifically, they now float, stick to the side of the toilet bowl, and smell extremely foul. His past medical history is significant for several episodes of acute pancreatitis secondary to excessive alcohol consumption. His symptoms are found to be due to a deficiency in an enzyme. Which of the following enzymes is most likely deficient in this patient?
- A. Enterokinase
- B. Amylase
- C. Colipase
- D. Lipase (Correct Answer)
- E. Chymotrypsin
Carbohydrate digestion and absorption Explanation: ***Lipase***
- The patient's history of **recurrent pancreatitis** likely led to **exocrine pancreatic insufficiency**, reducing the production of digestive enzymes, particularly **lipase**.
- **Steatorrhea** (foul-smelling, floating, sticky stools) is a classic symptom of **fat malabsorption**, which occurs due to insufficient lipase for triglyceride digestion.
*Enterokinase*
- **Enterokinase** is an enzyme produced in the **duodenum** that activates trypsinogen to trypsin, which then activates other pancreatic proteases.
- A deficiency would primarily cause **protein malabsorption**, not the pronounced fat malabsorption (steatorrhea) seen in this patient.
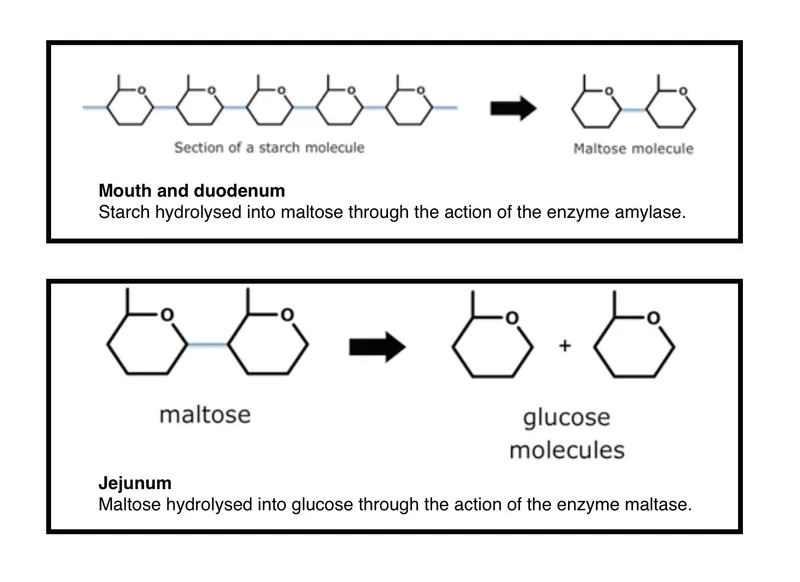
*Amylase*
- **Amylase** is responsible for **carbohydrate digestion**.
- While chronic pancreatitis can lead to amylase deficiency, the primary symptom of this patient's diarrhea, steatorrhea, points more directly to **fat malabsorption** rather than carbohydrate malabsorption.
*Colipase*
- **Colipase** is a co-enzyme that helps **lipase** bind to the fat-water interface to digest triglycerides.
- While essential for fat digestion, lipase itself is the primary enzyme responsible, and a direct deficiency in colipase alone is less commonly implicated as the sole cause of severe steatorrhea than a general pancreatic enzyme insufficiency affecting lipase production.
*Chymotrypsin*
- **Chymotrypsin** is a **protease** primarily involved in **protein digestion**.
- A deficiency would lead to **protein malabsorption**, which typically presents with symptoms like muscle wasting and edema, rather than the prominent steatorrhea described.
Carbohydrate digestion and absorption US Medical PG Question 5: An investigator is studying membranous transport proteins in striated muscle fibers of an experimental animal. An electrode is inserted into the gluteus maximus muscle and a low voltage current is applied. In response to this, calcium is released from the sarcoplasmic reticulum of the muscle fibers and binds to troponin C, which results in a conformational change of tropomyosin and unblocking of the myosin-binding site. The membranous transport mechanism underlying the release of calcium into the cytosol most resembles which of the following processes?
- A. Opening of acetylcholine receptors at neuromuscular junction
- B. Reabsorption of glucose by renal tubular cells
- C. Secretion of doxorubicin from dysplastic colonic cells
- D. Uptake of fructose by small intestinal enterocytes (Correct Answer)
- E. Removal of calcium from cardiac myocytes
Carbohydrate digestion and absorption Explanation: **Uptake of fructose by small intestinal enterocytes**
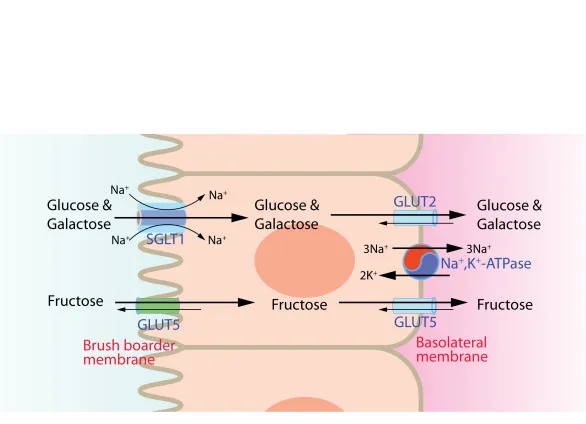
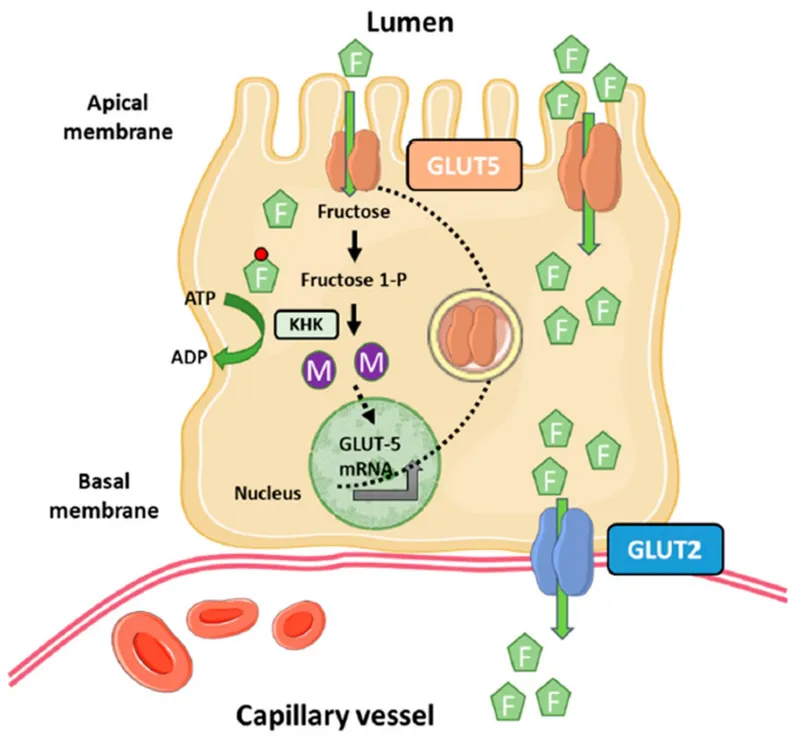
- The release of calcium from the sarcoplasmic reticulum into the cytosol in muscle contraction is primarily mediated by **ryanodine receptors**, which are a type of **facilitated diffusion channel**.
- **Fructose uptake** in the small intestine occurs via **GLUT5 transporters**, which also utilize **facilitated diffusion**, moving fructose down its concentration gradient without direct energy expenditure.
*Opening of acetylcholine receptors at neuromuscular junction*
- The opening of **acetylcholine receptors** is a form of **ligand-gated ion channel** activity, specific to the binding of acetylcholine.
- While it involves channel opening, it's initiated by a chemical signal, whereas sarcoplasmic reticulum calcium release is often voltage-gated or mechanically coupled to voltage sensors.
*Reabsorption of glucose by renal tubular cells*
- Glucose reabsorption in renal tubules primarily involves **secondary active transport** via **SGLT transporters**, which co-transport glucose with sodium.
- This process requires energy indirectly, unlike the facilitated diffusion of calcium from the sarcoplasmic reticulum.
*Secretion of doxorubicin from dysplastic colonic cells*
- The secretion of doxorubicin, an anticancer drug, from cells often involves **ATP-binding cassette (ABC) transporters** (e.g., MDR1), which utilize **primary active transport** to pump substances against their concentration gradient using ATP.
- This is an energy-dependent process, distinct from facilitated diffusion.
*Removal of calcium from cardiac myocytes*
- The removal of calcium from cardiac myocytes occurs primarily via the **SERCA pump** (an **ATP-dependent active transporter**) back into the sarcoplasmic reticulum and the **Na+/Ca2+ exchanger** (a **secondary active transporter**) out of the cell.
- Both mechanisms require energy, either directly or indirectly, to move calcium against its electrochemical gradient.
Carbohydrate digestion and absorption US Medical PG Question 6: A 5-month-old boy presents with increasing weakness for the past 3 months. The patient’s mother says that the weakness is accompanied by dizziness, sweating, and vertigo early in the morning. Physical examination shows hepatomegaly. Laboratory findings show an increased amount of lactate, uric acid, and elevated triglyceride levels. Which of the following enzymes is most likely deficient in this patient?
- A. Hepatic glycogen phosphorylase
- B. Debranching enzyme
- C. Glucose-6-phosphatase (Correct Answer)
- D. Muscle glycogen phosphorylase
- E. Lysosomal α-1,4-glucosidase
Carbohydrate digestion and absorption Explanation: ***Glucose-6-phosphatase***
- The constellation of **hypoglycemia** (weakness, dizziness, sweating, vertigo, especially early morning), **hepatomegaly**, **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia** are classic features of **Type I glycogen storage disease (von Gierke disease)**, which is caused by a deficiency of **glucose-6-phosphatase**.
- This enzyme is crucial for the final step of both **glycogenolysis** and **gluconeogenesis**, releasing free glucose into the bloodstream; its deficiency leads to an inability to maintain normal blood glucose levels during fasting and accumulation of glucose-6-phosphate, which shunts into other metabolic pathways.
*Hepatic glycogen phosphorylase*
- Deficiency in **hepatic glycogen phosphorylase** (Type VI glycogen storage disease, Hers disease) would cause **hepatomegaly** and **hypoglycemia**, but typically does not present with severe **lactic acidosis**, **hyperuricemia**, or **hypertriglyceridemia** to the same degree as von Gierke disease.
- The primary defect is in breaking down glycogen, leading to its accumulation in the liver, but the products of glycolysis can still exit the liver via gluconeogenesis.
*Debranching enzyme*
- Deficiency in **debranching enzyme** (Type III glycogen storage disease, Cori or Forbes disease) causes **hepatomegaly** and **hypoglycemia**, but usually presents with milder symptoms and less severe **lactic acidosis**, **hyperuricemia**, and **hypertriglyceridemia**.
- Patients often present with symptoms similar to Type I, but muscle involvement is also common, and **glycogen structures with short outer branches** are characteristic.
*Muscle glycogen phosphorylase*
- Deficiency in **muscle glycogen phosphorylase** (Type V glycogen storage disease, McArdle disease) primarily affects **skeletal muscle**, leading to exercise intolerance, muscle pain, and myoglobinuria.
- It does not typically cause **hypoglycemia** or **hepatomegaly**, as the liver enzyme is functional, and the symptoms described are systemic rather than muscle-specific.
*Lysosomal α-1,4-glucosidase*
- Deficiency in **lysosomal α-1,4-glucosidase** (Type II glycogen storage disease, Pompe disease) primarily affects the **heart, muscle, and liver**, causing severe **cardiomyopathy**, hypotonia, and **hepatomegaly**.
- While it involves glycogen accumulation, it typically does not present with **hypoglycemia** (as cytoplasmic glycogen metabolism is intact), **lactic acidosis**, or the specific metabolic derangements seen in this patient.
Carbohydrate digestion and absorption US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Carbohydrate digestion and absorption Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Carbohydrate digestion and absorption US Medical PG Question 8: A 7-month-old boy is brought to the pediatrician for a change in his behavior. The patient has been exclusively breastfeeding up until this point and has been meeting his developmental milestones. He is in the 90th percentile for weight and 89th percentile for height. Two weeks ago, his parents began introducing weaning foods including fruit purees and baby formula. This past week, the patient has been increasingly lethargic, vomiting, and has been refusing to eat. The patient's parents state that he had an episode this morning where he was not responsive and was moving his extremities abnormally followed by a period of somnolence. The patient's past medical history is notable for shoulder dystocia and poorly managed maternal diabetes during the pregnancy. His temperature is 99.5°F (37.5°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a lethargic infant with a distinctive sweet, fruity smell to his breath. Which of the following is most likely deficient in this patient?
- A. Branched chain alpha-ketoacid dehydrogenase (Correct Answer)
- B. Galactose-1-phosphate uridyltransferase
- C. Aldolase B
- D. Glucose-6-phosphatase
- E. Ornithine transcarbamolase
Carbohydrate digestion and absorption Explanation: ***Branched chain alpha-ketoacid dehydrogenase***
- This patient's presentation is classic for **maple syrup urine disease (MSUD)**, caused by deficiency of branched chain alpha-ketoacid dehydrogenase complex.
- The **distinctive sweet, fruity smell to the breath** (and urine) is pathognomonic for MSUD, resulting from accumulation of branched chain amino acids (leucine, isoleucine, valine) and their ketoacid metabolites.
- Symptoms typically manifest upon introduction of **increased protein load** (baby formula), presenting with **lethargy, vomiting, poor feeding, seizures, and encephalopathy** due to neurotoxicity from elevated leucine and other metabolites.
- The timing (introduced weaning foods including formula) and clinical picture of acute metabolic crisis with characteristic odor make this the most likely diagnosis.
*Ornithine transcarbamylase*
- OTC deficiency causes **hyperammonemic crisis** with similar neurological symptoms (lethargy, vomiting, seizures) triggered by protein intake.
- However, hyperammonemia typically produces a **musty or ammonia-like odor**, NOT the sweet, fruity smell described in this case.
- While the clinical timing fits, the **characteristic breath odor is inconsistent** with urea cycle disorders.
*Galactose-1-phosphate uridyltransferase*
- Deficiency causes **classic galactosemia**, presenting with **vomiting, lethargy, jaundice, hepatomegaly, and cataracts** after lactose exposure (milk/formula).
- The **sweet, fruity breath odor is NOT characteristic** of galactosemia.
- While formula introduction could trigger symptoms, the specific odor and predominant neurological presentation point away from this diagnosis.
*Aldolase B*
- **Hereditary fructose intolerance** manifests upon fructose exposure (fruit purees) with **vomiting, hypoglycemia, jaundice, hepatomegaly, and renal dysfunction**.
- The patient did consume fruit purees, but the **sweet, fruity breath odor is NOT a feature** of fructose intolerance.
- The severe acute encephalopathy and characteristic odor make MSUD more likely.
*Glucose-6-phosphatase*
- **Von Gierke disease (Type I GSD)** presents with **severe fasting hypoglycemia, lactic acidosis, hepatomegaly, and hyperlipidemia**.
- The **sweet, fruity odor is NOT characteristic**, and symptoms are primarily related to fasting/glucose homeostasis rather than acute protein-induced metabolic crisis.
- The clinical picture does not fit a glycogen storage disorder.
Carbohydrate digestion and absorption US Medical PG Question 9: A 39-year-old woman presents to her primary care physician because she has been experiencing intermittent abdominal pain for the last 2 weeks. She says that the pain is squeezing in nature, is located in the right upper quadrant, and is particularly severe after eating a meal. After a diagnosis is made, the patient asks why the pain gets worse after eating. The physician explains that food is detected by the gastrointestinal tract through numerous receptors and that this information is transmitted to other parts of the body to cause compensatory changes. The neurons responsible for transmitting this information are most likely located in a layer of the intestine that has which of the following characteristics?
- A. Contracts to generate local movement in mucosa
- B. Contains cells that primarily absorb nutrients
- C. Connective tissue that envelops the other layers
- D. Contracts to generate peristaltic waves (Correct Answer)
- E. Contains large blood vessels and large lymphatic vessels
Carbohydrate digestion and absorption Explanation: ***Contracts to generate peristaltic waves***
- This describes the **muscularis propria** (external muscle layer), which contains the **myenteric plexus (Auerbach's plexus)** between its inner circular and outer longitudinal smooth muscle layers.
- The **myenteric plexus is the primary neural network** responsible for detecting food through mechanoreceptors and chemoreceptors, transmitting sensory information, and coordinating both local reflexes and systemic compensatory responses throughout the gastrointestinal tract.
- These neurons communicate with the **autonomic nervous system** and coordinate the release of hormones like **cholecystokinin (CCK)** after eating, which causes gallbladder contraction (relevant to this patient's postprandial pain from cholecystitis).
- While this layer's most obvious function is generating peristalsis, it contains the most extensive enteric nervous system network for sensory integration and motor coordination.
*Contains large blood vessels and large lymphatic vessels*
- This describes the **submucosa**, which contains the **submucosal plexus (Meissner's plexus)**.
- While the submucosal plexus does contain sensory neurons, it primarily regulates **local functions** such as mucosal secretion, absorption, and blood flow rather than the broader systemic compensatory responses described in the question.
- The submucosa's neural network is more limited compared to the myenteric plexus.
*Contracts to generate local movement in mucosa*
- This describes the **muscularis mucosae**, a thin layer of smooth muscle within the mucosa that causes local folding and movement of the mucosal surface.
- This layer lacks significant neural plexuses and is not involved in transmitting sensory information for systemic responses.
*Contains cells that primarily absorb nutrients*
- This refers to the **mucosa**, specifically the epithelial cells lining the intestinal surface.
- While the mucosa contains chemoreceptors and mechanoreceptors, the question asks about the neurons that **transmit** this information, which are located in the deeper neural plexuses (primarily myenteric), not in the absorptive epithelium itself.
*Connective tissue that envelops the other layers*
- This describes the **serosa** (or adventitia), the outermost protective layer.
- The serosa contains minimal neural tissue and is not involved in sensory detection or transmission of gastrointestinal information.
Carbohydrate digestion and absorption US Medical PG Question 10: A 65-year-old woman comes to the physician because of progressive weight loss for 3 months. Physical examination shows jaundice and a nontender, palpable gallbladder. A CT scan of the abdomen shows an ill-defined mass in the pancreatic head. She is scheduled for surgery to resect the pancreatic head, distal stomach, duodenum, early jejunum, gallbladder, and common bile duct and anastomose the jejunum to the remaining stomach, pancreas, and bile duct. Following surgery, this patient is at the greatest risk for which of the following?
- A. Wide-based gait
- B. Calcium oxalate kidney stones
- C. Microcytic anemia (Correct Answer)
- D. Increased bile production
- E. Hypercoagulable state
Carbohydrate digestion and absorption Explanation: ***Microcytic anemia***
- The surgical procedure described is a **Whipple procedure**, which involves partial gastrectomy and duodenectomy. This significant alteration to the upper GI tract can lead to **iron malabsorption**, as iron is primarily absorbed in the duodenum and proximal jejunum, and gastric acid is crucial for converting dietary iron to its absorbable ferrous form.
- **Iron deficiency** is the most common cause of **microcytic anemia**, characterized by small, pale red blood cells, due to impaired hemoglobin synthesis as a result of insufficient iron availability for the heme component.
*Wide-based gait*
- A **wide-based gait** is typically associated with **ataxia** or conditions affecting cerebellar function or proprioception, which are not direct complications of a Whipple procedure.
- While nutritional deficiencies can occur post-surgery, a wide-based gait specifically points to neurological impairment rather than postsurgical metabolic issues.
*Calcium oxalate kidney stones*
- **Calcium oxalate kidney stones** are often associated with conditions causing **hypercalciuria** or malabsorption of fat, which leads to increased oxalate absorption in the colon. While fat malabsorption can occur after a Whipple due to pancreatic insufficiency, dietary oxalate intake and hydration status are generally more significant determinants of stone formation.
- The surgery itself does not directly increase the risk for calcium oxalate kidney stones more than other listed complications.
*Increased bile production*
- A Whipple procedure involves the removal of the **gallbladder** and rerouting of the **bile duct** directly into the jejunum. This does not lead to increased bile production, but rather a different regulation and flow of bile.
- In fact, the absence of the gallbladder means there is no storage for bile, leading to a continuous, unregulated flow of bile into the small intestine, potentially contributing to maldigestion or diarrhea, but not "increased production."
*Hypercoagulable state*
- While surgery, including a Whipple procedure, can transiently increase the risk of a **hypercoagulable state** (e.g., deep vein thrombosis, pulmonary embolism) in the immediate postoperative period due to immobility and tissue injury, this risk is generally mitigated with prophylactic anticoagulation.
- The question asks about the **greatest risk** post-surgery, and long-term complications related to altered anatomy and malabsorption, such as microcytic anemia, are more direct and sustained consequences unique to the extent of the resection.
More Carbohydrate digestion and absorption US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.