Ventilation-perfusion matching US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ventilation-perfusion matching. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ventilation-perfusion matching US Medical PG Question 1: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Ventilation-perfusion matching Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Ventilation-perfusion matching US Medical PG Question 2: A 32-year-old woman presents with progressive shortness of breath and a dry cough. She says that her symptoms onset recently after a 12-hour flight. Past medical history is unremarkable. Current medications are oral estrogen/progesterone containing contraceptive pills. Her vital signs include: blood pressure 110/60 mm Hg, pulse 101/min, respiratory rate 22/min, oxygen saturation 88% on room air, and temperature 37.9℃ (100.2℉). Her weight is 94 kg (207.2 lb) and height is 170 cm (5 ft 7 in). On physical examination, she is acrocyanotic. There are significant swelling and warmth over the right calf. There are widespread bilateral rales present. Cardiac auscultation reveals accentuation of the pulmonic component of the second heart sound (P2) and an S3 gallop. Which of the following ventilation/perfusion (V/Q) ratios most likely corresponds to this patient’s condition?
- A. 1.3 (Correct Answer)
- B. 1
- C. 0.8
- D. 0.5
- E. 0.3
Ventilation-perfusion matching Explanation: ***1.3***
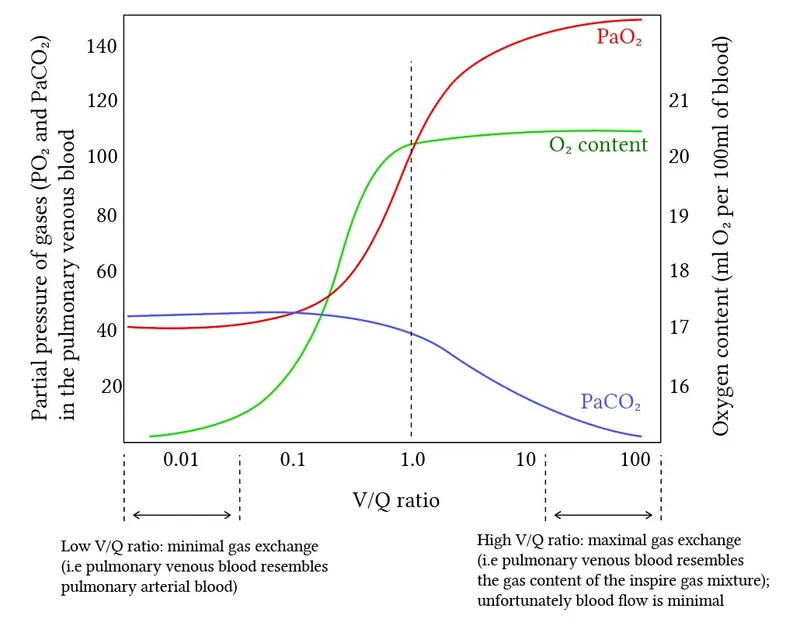
- This value represents an increased V/Q ratio, or **dead space ventilation**, which is characteristic of a **pulmonary embolism (PE)**. In PE, a portion of the lung is ventilated but not perfused due to the embolism blocking blood flow, leading to wasted ventilation.
- The patient's symptoms (sudden onset dyspnea after a long flight, use of oral contraceptives, calf swelling, hypoxia, and accentuated P2) are highly suggestive of a PE, which is the most likely cause of increased V/Q mismatch.
*1*
- A V/Q ratio of 1 indicates **perfect matching** of ventilation and perfusion, which is an ideal state not typically achieved throughout the entire lung, especially in disease.
- This value would not explain the patient's severe **hypoxia** and overall clinical picture of respiratory distress.
*0.8*
- This is the **average normal V/Q ratio** for the lung as a whole, representing slightly more perfusion than ventilation.
- While it's a normal physiological state, it does not account for the significant V/Q mismatch indicated by the patient's severe hypoxemia (SpO2 88%) and clinical symptoms.
*0.5*
- This value represents a **low V/Q ratio**, indicating relatively more perfusion than ventilation, often seen in conditions like **shunt physiology** (e.g., pneumonia, atelectasis, pulmonary edema).
- While the patient has rales and an S3 gallop suggesting potential pulmonary edema or heart failure secondary to increased right heart strain, the primary pathophysiology in PE is increased V/Q due to unperfused but ventilated lung regions.
*0.3*
- This is a severely **low V/Q ratio**, approaching a **shunt**, where blood passes through the lungs without being adequately oxygenated. This is typical of conditions like **severe pneumonia, ARDS, or significant atelectasis**.
- While PE can cause some degree of bronchoconstriction leading to areas of low V/Q, the predominant and most impactful V/Q mismatch in PE is the high V/Q ratio in areas of unperfused lung.
Ventilation-perfusion matching US Medical PG Question 3: Four days after undergoing an elective total hip replacement, a 65-year-old woman develops a DVT that embolizes to the lung. Along with tachypnea, tachycardia, and cough, the patient would most likely present with a PaO2 of what?
- A. 120 mmHg
- B. 100 mmHg
- C. 85 mmHg (Correct Answer)
- D. 110 mmHg
- E. 60 mmHg
Ventilation-perfusion matching Explanation: ***85 mmHg***
- A pulmonary embolism (PE) causes a **ventilation-perfusion (V/Q) mismatch**, leading to **hypoxemia** and a reduced PaO2.
- While exact values vary, a PaO2 of 85 mmHg indicates **mild to moderate hypoxemia**, which is common in PE, especially with accompanying symptoms like tachypnea and tachycardia.
*120 mmHg*
- This value is significantly **higher than normal (75-100 mmHg)** and would indicate **hyperoxia**, which is inconsistent with acute pulmonary embolism causing respiratory distress.
- A patient with PE would typically have **reduced oxygenation**, not supernormal levels, unless receiving high-flow supplemental oxygen.
*100 mmHg*
- A PaO2 of 100 mmHg is at the **upper end of the normal range** (75-100 mmHg) and would imply **no significant hypoxemia**.
- Given the patient's symptoms of tachypnea, tachycardia, and cough following a DVT with embolization, a normal or high-normal PaO2 is unlikely without aggressive oxygen therapy (which is not stated).
*110 mmHg*
- This value is **above the normal range** and suggests **hyperoxia**, which is contrary to the pathophysiology of a pulmonary embolism.
- A PE impairs gas exchange, leading to a decrease in PaO2, not an increase.
*60 mmHg*
- A PaO2 of 60 mmHg indicates **significant hypoxemia**, which might occur in a severe, large pulmonary embolism or in a patient with underlying lung disease.
- While possible, 85 mmHg represents a more common, moderate hypoxemia seen in PE, especially given the prompt presentation of symptoms.
Ventilation-perfusion matching US Medical PG Question 4: A 30-year-old patient presents to clinic for pulmonary function testing. With body plethysmography, the patient's functional residual capacity is 3 L, tidal volume is 650 mL, expiratory reserve volume is 1.5 L, total lung capacity is 8 L, and dead space is 150 mL. Respiratory rate is 15 breaths per minute. What is the alveolar ventilation?
- A. 7.5 L/min (Correct Answer)
- B. 7 L/min
- C. 8.5 L/min
- D. 8 L/min
- E. 6.5 L/min
Ventilation-perfusion matching Explanation: ***7.5 L/min***
- Alveolar ventilation (VA) is calculated as (**tidal volume** - **dead space**) x **respiratory rate**.
- In this case, (650 mL - 150 mL) x 15 breaths/min = 500 mL x 15 = 7500 mL/min, which is 7.5 L/min.
*7 L/min*
- This answer would be obtained if the **dead space** was incorrectly subtracted from the **tidal volume** as 200 mL instead of 150 mL, or if there was a calculation error.
- The correct calculation requires accurate use of the provided tidal volume and dead space.
*8.5 L/min*
- This value is not consistent with the correct formula for alveolar ventilation using the given parameters.
- It does not arise from a common miscalculation of **tidal volume**, **dead space**, or **respiratory rate**.
*8 L/min*
- This result might occur from an incorrect addition or subtraction of volumes, or misapplication of the formula for total minute ventilation instead of alveolar ventilation.
- The formula for **total minute ventilation** is **tidal volume** x **respiratory rate**, which would be 0.65 L x 15 = 9.75 L/min, further demonstrating this option is incorrect for alveolar ventilation.
*6.5 L/min*
- This result would be obtained if the **dead space** was incorrectly assumed to be a larger value or if the calculation for subtraction from **tidal volume** was flawed.
- The correct alveolar ventilation calculation precisely accounts for the wasted ventilation in the dead space.
Ventilation-perfusion matching US Medical PG Question 5: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
Ventilation-perfusion matching Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
Ventilation-perfusion matching US Medical PG Question 6: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Ventilation-perfusion matching Explanation: ***Pulmonary embolism***
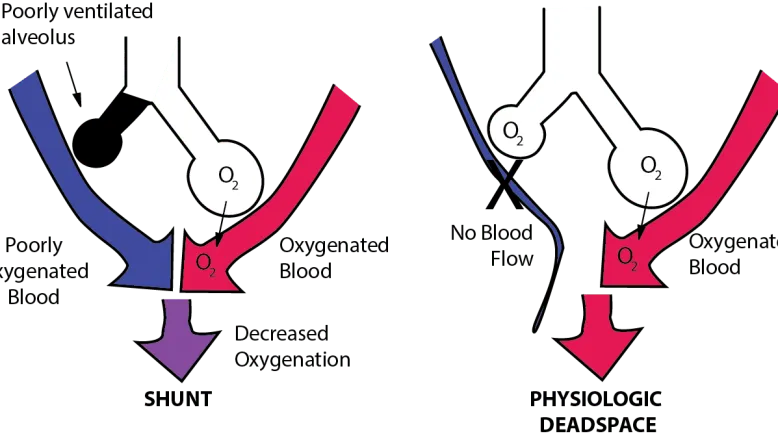
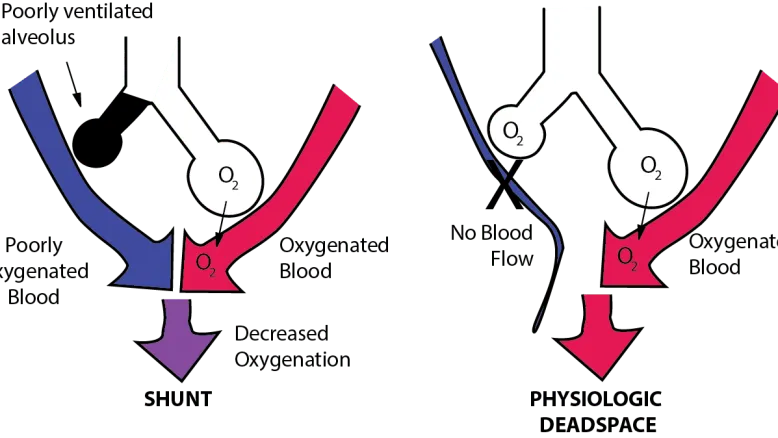
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Ventilation-perfusion matching US Medical PG Question 7: A 19-year-old male soccer player undergoes an exercise tolerance test to measure his maximal oxygen uptake during exercise. Which of the following changes are most likely to occur during exercise?
- A. Increased apical ventilation-perfusion ratio
- B. Decreased physiologic dead space (Correct Answer)
- C. Decreased alveolar-arterial oxygen gradient
- D. Increased arterial partial pressure of oxygen
- E. Increased pulmonary vascular resistance
Ventilation-perfusion matching Explanation: **Decreased physiologic dead space**
- During exercise, there is improved perfusion to previously underperfused areas of the lung, leading to a **more uniform ventilation-perfusion (V/Q) matching** and thus a decrease in physiologic dead space.
- The increased cardiac output helps to perfuse more capillaries, reducing the amount of ventilated air that does not participate in gas exchange.
*Increased apical ventilation-perfusion ratio*
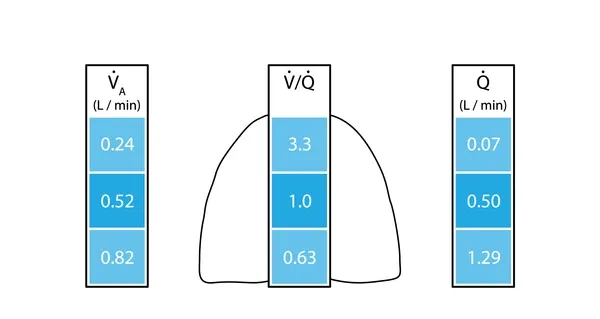
- At rest, the **apical V/Q ratio is already high** due to gravity-dependent differences in blood flow; exercise partially normalizes these differences.
- While overall V/Q matching improves, the relative V/Q differences between apical and basal regions may become less pronounced, not necessarily a further increase in the apical ratio.
*Decreased alveolar-arterial oxygen gradient*
- During severe exercise, the **A-a gradient often increases slightly** due to increased oxygen diffusion limitations and V/Q mismatch.
- Although overall gas exchange efficiency improves, the sheer volume of oxygen demand can reveal small imbalances, rather than fully eliminating the gradient.
*Increased arterial partial pressure of oxygen*
- Exercise typically leads to **stable or slightly decreased arterial PO2** in healthy individuals due to the increased metabolic demand and potential small V/Q mismatches.
- The body maintains arterial PO2 remarkably well even at high exertion, but it does not usually significantly increase.
*Increased pulmonary vascular resistance*
- During exercise, **pulmonary vascular resistance (PVR) generally decreases** due to recruitment and distension of pulmonary capillaries.
- This decrease in PVR helps to accommodate the increased cardiac output without a significant rise in pulmonary arterial pressure.
Ventilation-perfusion matching US Medical PG Question 8: A 68-year-old man comes to the emergency room with difficulty in breathing. He was diagnosed with severe obstructive lung disease a few years back. He uses his medication but often has to come to the emergency room for intravenous therapy to help him breathe. He was a smoker for 40 years smoking two packs of cigarettes every day. Which of the following best represents the expected changes in his ventilation, perfusion and V/Q ratio?
- A. Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio
- B. Medium ventilation and perfusion, V/Q that equals 0.8
- C. Higher ventilation and perfusion with lower V/Q ratio
- D. Low ventilation, normal perfusion and low V/Q ratio (Correct Answer)
- E. Lower ventilation and perfusion, but higher V/Q ratio
Ventilation-perfusion matching Explanation: ***Low ventilation, normal perfusion and low V/Q ratio***
- In severe **obstructive lung disease** (like COPD), there is airflow limitation, leading to areas of **hypoventilation** in the lungs.
- While ventilation is compromised, blood flow (perfusion) to these areas can remain relatively normal, resulting in a **decreased V/Q ratio**.
*Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio*
- This scenario describes a lung unit with **dead space ventilation**, where there is ventilation but no blood flow (e.g., in a pulmonary embolism).
- The patient's history of **obstructive lung disease** primarily indicates impaired airflow, not a lack of perfusion.
*Medium ventilation and perfusion, V/Q that equals 0.8*
- A **V/Q ratio of 0.8** represents the **ideal normal** ventilation-perfusion matching in a healthy lung.
- The patient has severe obstructive lung disease, which by definition means there is significant mismatch, not normal physiology.
*Higher ventilation and perfusion with lower V/Q ratio*
- While hyperventilation can occur in attempts to compensate, the primary issue in obstructive disease is **impaired ventilation**, not increased ventilation, leading to decreased gas exchange.
- A lower V/Q ratio is expected, but it is driven by **low ventilation**, not higher ventilation and perfusion.
*Lower ventilation and perfusion, but higher V/Q ratio*
- Although both ventilation and perfusion can be affected in severe disease, a **higher V/Q ratio** typically implies areas of increased dead space (more ventilation than perfusion).
- In obstructive disease, the predominant problem is **impaired air entry**, leading to underventilated units with relatively preserved perfusion, thus a **low V/Q ratio**.
Ventilation-perfusion matching US Medical PG Question 9: Two days after undergoing left hemicolectomy for a colonic mass, a 62-year-old man develops shortness of breath. His temperature is 38.1°C (100.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 120/78 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 88%. Cardiopulmonary examination shows decreased breath sounds and decreased fremitus at both lung bases. Arterial blood gas analysis on room air shows:
pH 7.35
PaO2 70 mm Hg
PCO2 40 mm Hg
An x-ray of the chest shows a collapse of the bases of both lungs. Which of the following is the most likely underlying mechanism of this patient's hypoxemia?
- A. Increased anatomic dead space
- B. Decreased hemoglobin oxygen-binding capacity
- C. Decreased chest wall compliance
- D. Increased tidal volume
- E. Decreased ratio of ventilated alveoli (Correct Answer)
Ventilation-perfusion matching Explanation: ***Decreased ratio of ventilated alveoli***
- The patient's presentation with **shortness of breath**, **decreased breath sounds and fremitus at both lung bases**, and **collapsed lung bases on chest x-ray** points to **atelectasis**.
- **Atelectasis** is a common cause of hypoxemia post-surgery. It occurs when alveoli collapse, leading to areas of the lung that are perfused but not ventilated, resulting in a **ventilation-perfusion (V/Q) mismatch** with a decreased ratio of ventilated alveoli.
*Increased anatomic dead space*
- **Anatomic dead space** refers to the conducting airways where gas exchange does not occur. This value is relatively constant and would not increase significantly to cause such profound hypoxemia in this context.
- Conditions like chronic obstructive pulmonary disease (COPD) can increase dead space, but the patient's acute postoperative presentation and chest X-ray findings do not support this as the primary cause.
*Decreased hemoglobin oxygen-binding capacity*
- This would involve issues like **carbon monoxide poisoning** or specific hemoglobinopathies, which are not indicated by the clinical picture or ABG results (normal pH, PaO2 70 mmHg, PCO2 40 mmHg).
- The PaO2 and SaO2 values indicate a problem with oxygen uptake, not oxygen transport by hemoglobin once bound.
*Decreased chest wall compliance*
- While surgery can cause **pain leading to splinting** and reduced chest wall expansion, which impacts compliance, the primary mechanism of hypoxemia in atelectasis is the **collapse of alveoli**, not solely reduced chest wall movement.
- The **collapsed lung bases** on X-ray directly point to alveolar collapse rather than a general decrease in chest wall compliance as the primary problem.
*Increased tidal volume*
- **Increased tidal volume** would typically improve ventilation and oxygenation, not lead to hypoxemia.
- The patient's **hypoxemia (SaO2 88%, PaO2 70 mmHg)** clearly indicates a problem with oxygen uptake, not an enhancement of respiratory function.
Ventilation-perfusion matching US Medical PG Question 10: A 21-year-old man is admitted to the intensive care unit for respiratory failure requiring mechanical ventilation. His minute ventilation is calculated to be 7.0 L/min, and his alveolar ventilation is calculated to be 5.1 L/min. Which of the following is most likely to decrease the difference between minute ventilation and alveolar ventilation?
- A. Increasing the partial pressure of inhaled oxygen
- B. Decreasing the affinity of hemoglobin for oxygen
- C. Increasing the respiratory depth
- D. Decreasing the physiologic dead space (Correct Answer)
- E. Increasing the respiratory rate
Ventilation-perfusion matching Explanation: ***Decreasing the physiologic dead space***
- The difference between **minute ventilation (VE)** and **alveolar ventilation (VA)** is the **dead space ventilation (VD)**, calculated as: VE - VA = VD
- In this case: 7.0 L/min - 5.1 L/min = 1.9 L/min of dead space ventilation
- Decreasing the **physiologic dead space** directly reduces this difference by allowing a greater proportion of each breath to participate in gas exchange
- This is the most direct way to narrow the gap between VE and VA
*Increasing the partial pressure of inhaled oxygen*
- This intervention primarily affects **oxygenation** by increasing the driving pressure for oxygen diffusion into the blood
- It does not directly change the volume of air participating in alveolar ventilation or reduce dead space ventilation
- The distribution of ventilation between alveolar and dead space remains unchanged
*Decreasing the affinity of hemoglobin for oxygen*
- A decrease in hemoglobin affinity for oxygen facilitates **oxygen unloading** to the tissues (rightward shift of the oxygen-hemoglobin dissociation curve)
- This effect is related to **oxygen delivery** and does not alter the proportion of minute ventilation that reaches the alveoli for gas exchange
- Dead space ventilation remains unchanged
*Increasing the respiratory depth*
- Increasing respiratory depth increases **tidal volume (VT)**, which improves the **ratio** of alveolar ventilation to minute ventilation (VA/VE efficiency)
- However, the **absolute difference** (VE - VA) in L/min depends on the **total dead space volume**, which is not changed by increasing tidal volume alone
- While this improves ventilation efficiency, it does not directly reduce the dead space ventilation measured in L/min unless physiologic dead space itself decreases
*Increasing the respiratory rate*
- While increasing respiratory rate increases **minute ventilation (VE)**, it also increases the frequency of ventilating the **dead space** with each breath
- Since dead space ventilation (VD) = respiratory rate × dead space volume, increasing rate while keeping tidal volume constant will proportionally increase both VE and VD
- This can actually widen the absolute gap between VE and VA, making it less efficient
More Ventilation-perfusion matching US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.