Hypoxemia mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypoxemia mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypoxemia mechanisms US Medical PG Question 1: A 21-year-old man presents to his physician because he has been feeling increasingly tired and short of breath at work. He has previously had these symptoms but cannot recall the diagnosis he was given. Chart review reveals the following results:
Oxygen tension in inspired air = 150 mmHg
Alveolar carbon dioxide tension = 50 mmHg
Arterial oxygen tension = 71 mmHg
Respiratory exchange ratio = 0.80
Diffusion studies reveal normal diffusion distance. The patient is administered 100% oxygen but the patient's blood oxygen concentration does not improve. Which of the following conditions would best explain this patient's findings?
- A. Septal defect since birth (Correct Answer)
- B. Use of opioid medications
- C. Pulmonary fibrosis
- D. Pulmonary embolism
- E. Vacation at the top of a mountain
Hypoxemia mechanisms Explanation: ***Septal defect since birth***
- A congenital heart disease like a **septal defect** causes a right-to-left **shunt**, meaning deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- This type of shunt leads to **hypoxemia that is refractory to 100% oxygen** because the shunted blood will never pick up oxygen from the lungs.
*Use of opioid medications*
- Opioid use causes **respiratory depression**, leading to **hypoventilation** and increased arterial CO2 with decreased arterial O2.
- However, the hypoxemia from hypoventilation would typically improve significantly with **100% oxygen administration**, unlike in this case.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** causes thickening of the alveolar-capillary membrane, leading to impaired gas exchange and **diffusion limitation**.
- While it causes hypoxemia, the diffusion studies are stated to be **normal**, and hypoxemia due to diffusion limitation often improves with supplemental oxygen.
*Pulmonary embolism*
- A **pulmonary embolism** leads to V/Q mismatch by blocking blood flow to a portion of the lung, causing ventilation with no perfusion.
- Hypoxemia from V/Q mismatch generally **responds well to supplemental oxygen**, as the non-affected lung areas can compensate, unlike the scenario described.
*Vacation at the top of a mountain*
- Being at a high altitude causes **hypobaric hypoxia**, meaning there is a reduced partial pressure of oxygen in the inspired air.
- This type of hypoxemia typically **improves with supplemental oxygen** as it increases the inspired oxygen tension, which is contrary to the patient's findings.
Hypoxemia mechanisms US Medical PG Question 2: A 32-year-old woman presents with progressive shortness of breath and a dry cough. She says that her symptoms onset recently after a 12-hour flight. Past medical history is unremarkable. Current medications are oral estrogen/progesterone containing contraceptive pills. Her vital signs include: blood pressure 110/60 mm Hg, pulse 101/min, respiratory rate 22/min, oxygen saturation 88% on room air, and temperature 37.9℃ (100.2℉). Her weight is 94 kg (207.2 lb) and height is 170 cm (5 ft 7 in). On physical examination, she is acrocyanotic. There are significant swelling and warmth over the right calf. There are widespread bilateral rales present. Cardiac auscultation reveals accentuation of the pulmonic component of the second heart sound (P2) and an S3 gallop. Which of the following ventilation/perfusion (V/Q) ratios most likely corresponds to this patient’s condition?
- A. 1.3 (Correct Answer)
- B. 1
- C. 0.8
- D. 0.5
- E. 0.3
Hypoxemia mechanisms Explanation: ***1.3***
- This value represents an increased V/Q ratio, or **dead space ventilation**, which is characteristic of a **pulmonary embolism (PE)**. In PE, a portion of the lung is ventilated but not perfused due to the embolism blocking blood flow, leading to wasted ventilation.
- The patient's symptoms (sudden onset dyspnea after a long flight, use of oral contraceptives, calf swelling, hypoxia, and accentuated P2) are highly suggestive of a PE, which is the most likely cause of increased V/Q mismatch.
*1*
- A V/Q ratio of 1 indicates **perfect matching** of ventilation and perfusion, which is an ideal state not typically achieved throughout the entire lung, especially in disease.
- This value would not explain the patient's severe **hypoxia** and overall clinical picture of respiratory distress.
*0.8*
- This is the **average normal V/Q ratio** for the lung as a whole, representing slightly more perfusion than ventilation.
- While it's a normal physiological state, it does not account for the significant V/Q mismatch indicated by the patient's severe hypoxemia (SpO2 88%) and clinical symptoms.
*0.5*
- This value represents a **low V/Q ratio**, indicating relatively more perfusion than ventilation, often seen in conditions like **shunt physiology** (e.g., pneumonia, atelectasis, pulmonary edema).
- While the patient has rales and an S3 gallop suggesting potential pulmonary edema or heart failure secondary to increased right heart strain, the primary pathophysiology in PE is increased V/Q due to unperfused but ventilated lung regions.
*0.3*
- This is a severely **low V/Q ratio**, approaching a **shunt**, where blood passes through the lungs without being adequately oxygenated. This is typical of conditions like **severe pneumonia, ARDS, or significant atelectasis**.
- While PE can cause some degree of bronchoconstriction leading to areas of low V/Q, the predominant and most impactful V/Q mismatch in PE is the high V/Q ratio in areas of unperfused lung.
Hypoxemia mechanisms US Medical PG Question 3: A healthy 20-year-old male college student attempts to climb Mount Everest and travels to the Tibetan plateau by plane. Upon landing, he feels increasingly dizzy and fatigued. He notices that he is breathing faster than usual. What is the initial stimulus for the most likely acid-base disorder?
- A. Decreased partial pressure of alveolar oxygen (Correct Answer)
- B. Undiagnosed atrial septal defect
- C. Increasing arterial partial pressure of carbon dioxide
- D. Worsened diffusion limitation of oxygen
- E. Hypoxic pulmonary vasoconstriction
Hypoxemia mechanisms Explanation: ***Decreased partial pressure of alveolar oxygen***
- Upon rapid ascent to high altitude (like the Tibetan plateau), the ambient atmospheric pressure decreases, leading to a significant drop in the **partial pressure of inspired oxygen (PiO2)**.
- This reduction in PiO2 directly causes a decrease in the **partial pressure of alveolar oxygen (PAO2)**, which is the primary stimulus for activation of peripheral chemoreceptors, leading to hyperventilation and a respiratory alkalosis.
*Undiagnosed atrial septal defect*
- An atrial septal defect (ASD) would cause a **left-to-right shunt** in a healthy young adult, not typically presenting with acute dizziness and fatigue immediately upon high-altitude exposure.
- While an ASD can lead to cyanosis and dyspnea with exertion, it would not be the initial stimulus for the observed hyperventilation response to high altitude.
*Increasing arterial partial pressure of carbon dioxide*
- An increasing **arterial partial pressure of carbon dioxide (PaCO2)** would stimulate central chemoreceptors and increase ventilation, but it is not the initial trigger in this scenario.
- In response to **hypoxia** at high altitude, the body *hyperventilates*, which would lead to a *decrease* in PaCO2, not an increase.
*Worsened diffusion limitation of oxygen*
- **Diffusion limitation** of oxygen refers to impaired gas exchange across the alveolar-capillary membrane, usually due to conditions like fibrosis or edema.
- While gas exchange can be affected at extreme altitudes, it is not the primary initial physiological trigger for the body's acute response (hyperventilation) in a healthy individual.
*Hypoxic pulmonary vasodilation*
- **Hypoxic pulmonary vasoconstriction** (not vasodilation) is a physiological response in the lungs where pulmonary arterioles constrict in areas of low oxygen, redirecting blood flow to better-ventilated areas.
- This mechanism aims to optimize V/Q matching and is a *response* to hypoxia, not the initial stimulus for the systemic acid-base derangement leading to symptoms like dizziness and increased breathing rate.
Hypoxemia mechanisms US Medical PG Question 4: A 48-year-old man is brought to the emergency department 20 minutes after being rescued from a house fire. He reports headache, metallic taste, abdominal pain, and nausea. He appears confused and agitated. His pulse is 125/min, respirations are 33/min, and blood pressure is 100/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination shows a bright red color of the skin. His breath smells of bitter almonds. Hyperbaric oxygen therapy and appropriate pharmacotherapy are initiated. The expected beneficial effect of this drug is most likely due to which of the following mechanisms?
- A. Synthesis of 2,3-bisphosphoglycerate
- B. Formation of methemoglobin (Correct Answer)
- C. Inhibition of cytochrome c oxidase
- D. Dissociation of carboxyhemoglobin
- E. Reduction of ferric iron
Hypoxemia mechanisms Explanation: ***Formation of methemoglobin***
- This patient's symptoms (headache, confusion, bright red skin, bitter almond breath, high pulse oximetry despite severe symptoms) are classic for **cyanide poisoning**.
- Many antidotes for cyanide poisoning, such as **nitrites**, work by forming **methemoglobin**, which has a higher affinity for cyanide than cytochrome c oxidase, thus detaching cyanide from the enzyme and allowing cellular respiration to resume.
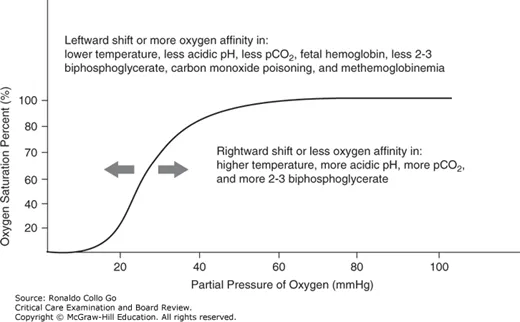
*Synthesis of 2,3-bisphosphoglycerate*
- **2,3-bisphosphoglycerate (2,3-BPG)** helps regulate oxygen release from hemoglobin in red blood cells.
- While important for oxygen delivery, increasing 2,3-BPG is not a direct therapeutic mechanism for **cyanide poisoning**.
*Inhibition of cytochrome c oxidase*
- **Cyanide** itself inhibits cytochrome c oxidase, leading to cellular hypoxia despite adequate oxygen supply.
- The therapeutic goal is to reverse this inhibition, not to further inhibit the enzyme.
*Dissociation of carboxyhemoglobin*
- **Carbon monoxide poisoning**, not cyanide poisoning, causes carboxyhemoglobin formation and presents with cherry-red skin, but there is no foul-smelling breath.
- Dissociating carboxyhemoglobin is relevant for carbon monoxide poisoning, not cyanide poisoning.
*Reduction of ferric iron*
- Reducing ferric iron (Fe3+) back to ferrous iron (Fe2+) would reverse **methemoglobinemia**, which is often a side effect of some cyanide antidotes.
- The therapeutic strategy for cyanide poisoning involves *inducing* methemoglobinemia to sequester cyanide.
Hypoxemia mechanisms US Medical PG Question 5: A 26-year-old woman is brought to the ED by her fiance with cyanosis and shortness of breath. Gradually over the last few days she has also experienced headaches, fatigue, and dizziness. Her past medical history is significant only for mild anemia attributed to menorrhagia, for which she takes an iron supplement. Per her fiance, she was recently laid-off, but is very excited about her new entrepreneurial endeavor of selling silk scarves that she dyes in their basement. She is afebrile, tachypneic, and tachycardic, and her oxygen saturation is 85% on room air, which seems high for her perceived degree of cyanosis. An arterial blood gas is drawn and the patient's blood is chocolate-colored. After a few minutes on 6 liters nasal canula, her oxygen saturation is still 85%. In addition to maintaining her airway, breathing, and circulation, what treatment should this patient also receive?
- A. Deferoxamine
- B. Dimercaprol
- C. Methylene blue (Correct Answer)
- D. Sodium bicarbonate
- E. Pralidoxime
Hypoxemia mechanisms Explanation: ***Methylene blue***
- The patient's symptoms (cyanosis, shortness of breath, headaches, dizziness, fatigue) coupled with **chocolate-colored blood**, **refractory hypoxemia despite oxygen supplementation**, and a history of exposure to **aniline dyes** (from dyeing silk scarves) are highly suggestive of **methemoglobinemia**.
- **Methylene blue** acts as an electron acceptor for NADPH-methemoglobin reductase, converting ferric iron (Fe3+) in methemoglobin back to ferrous iron (Fe2+) in hemoglobin, thus restoring oxygen-carrying capacity.
*Deferoxamine*
- **Deferoxamine** is a **chelating agent** primarily used to treat **iron toxicity** or iron overload disorders like hemochromatosis.
- While the patient has mild anemia and takes iron supplements, her presentation is not consistent with acute iron poisoning.
*Dimercaprol*
- **Dimercaprol** is a chelating agent used to treat poisoning by **heavy metals** such as arsenic, mercury, and lead.
- There is no indication in the patient's history or symptoms to suggest heavy metal poisoning.
*Sodium bicarbonate*
- **Sodium bicarbonate** is primarily used to treat **metabolic acidosis**, hyperkalemia, or certain drug overdoses (e.g., tricyclic antidepressants).
- Although the patient is tachypneic, there is no direct evidence of severe acidosis warranting bicarbonate, and it does not address the underlying cause of her hypoxemia.
*Pralidoxime*
- **Pralidoxime** (2-PAM) is a **cholinesterase reactivator** used as an antidote in conjunction with atropine for **organophosphate poisoning**.
- The patient's symptoms are not consistent with cholinergic crisis from organophosphate exposure.
Hypoxemia mechanisms US Medical PG Question 6: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Hypoxemia mechanisms Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Hypoxemia mechanisms US Medical PG Question 7: A man returns home late at night to find his 15-year-old son and 40-year-old wife unconscious in the family room. He immediately summons emergency services. In the field, pulse oximetry shows oxygen saturation at 100% for both patients. 100%, yet they both appear cyanotic. Both patients are provided with 2L of oxygen by way of nasal cannula on the way to the hospital. An arterial blood gas is performed on the teenager and reveals pH of 7.35, PaCO2 of 31.8 mm Hg, PaO2 of 150 mm Hg, HCO3- of 20 mEq/L, SaO2 of 80%, and a COHb of 18%. What is the most likely cause of his condition?
- A. Ischemic hypoxia
- B. Methemoglobinemia
- C. Diffusion-limited hypoxia
- D. Carbon monoxide poisoning (Correct Answer)
- E. Anemic hypoxia
Hypoxemia mechanisms Explanation: ***Carbon monoxide poisoning***
- The combination of **cyanosis**, **normal pulse oximetry readings (due to inaccurate readings for CO)**, and a **high COHb level (18%)** is highly indicative of carbon monoxide poisoning.
- Exposure to carbon monoxide forms **carboxyhemoglobin (COHb)**, which has a higher affinity for hemoglobin than oxygen, leading to **tissue hypoxia** despite normal PaO2.
*Ischemic hypoxia*
- This type of hypoxia occurs when there is **reduced blood flow** to a tissue, often due to conditions like **heart failure, shock**, or **arterial occlusion**.
- There is no clinical or lab evidence in the scenario to suggest reduced blood flow as the primary cause of the patient's symptoms.
*Methemoglobinemia*
- While methemoglobinemia can also cause **cyanosis** and an **oxygen saturation gap** (discrepancy between SaO2 and pulse oximetry), it is characterized by a high level of **methemoglobin (MetHb)**.
- The patient's COHb level is elevated at 18%, but there's no information suggesting elevated MetHb, distinguishing it from carbon monoxide poisoning.
*Diffusion-limited hypoxia*
- This occurs when the **diffusion of oxygen from the alveoli to the blood is impaired**, as seen in conditions like **pulmonary fibrosis** or **severe emphysema**.
- The patient's PaO2 of 150 mmHg is very high, indicating excellent oxygen loading in the lungs, which rules out a diffusion limitation.
*Anemic hypoxia*
- Anemic hypoxia results from a **decreased oxygen-carrying capacity of the blood** due to a **low hemoglobin concentration**.
- The scenario does not provide information about the patient's hemoglobin level, and the primary issue is the inability of hemoglobin to release oxygen due to CO binding, not a lack of hemoglobin itself.
Hypoxemia mechanisms US Medical PG Question 8: A 72-year-old man with coronary artery disease comes to the emergency department because of chest pain and shortness of breath for the past 3 hours. Troponin levels are elevated and an ECG shows ST-elevations in the precordial leads. Revascularization with percutaneous coronary intervention is performed, and a stent is successfully placed in the left anterior descending artery. Two days later, he complains of worsening shortness of breath. Pulse oximetry on 3L of nasal cannula shows an oxygen saturation of 89%. An x-ray of the chest shows distended pulmonary veins, small horizontal lines at the lung bases, and blunting of the costophrenic angles bilaterally. Which of the following findings would be most likely on a ventilation-perfusion scan of this patient?
- A. Matched ventilation and perfusion bilaterally
- B. Normal ventilation with multiple, bilateral perfusion defects
- C. Normal perfusion with bilateral ventilation defects (Correct Answer)
- D. Normal perfusion with decreased ventilation at the right base
- E. Increased apical ventilation with normal perfusion bilaterally
Hypoxemia mechanisms Explanation: ***Normal perfusion with bilateral ventilation defects***
- The patient's presentation with **worsening shortness of breath** after an acute coronary event, along with chest x-ray findings of **distended pulmonary veins, Kerley B lines (small horizontal lines at the lung bases), and blunting of the costophrenic angles**, is highly suggestive of **pulmonary edema** due to heart failure.
- In pulmonary edema, the alveoli fill with fluid, impeding gas exchange. This leads to **impaired ventilation** in the affected areas, while **pulmonary blood flow (perfusion) remains intact**. This results in **ventilation-perfusion (V/Q) mismatch** with impaired ventilation.
*Matched ventilation and perfusion bilaterally*
- This pattern would indicate a **normal ventilation-perfusion scan**, which is inconsistent with the patient's severe shortness of breath, hypoxemia, and radiographic signs of pulmonary edema.
- A matched V/Q scan suggests **healthy lung function** and gas exchange.
*Normal ventilation with multiple, bilateral perfusion defects*
- This pattern is characteristic of **pulmonary embolism**, where blood clots obstruct pulmonary arteries, leading to areas of the lung being ventilated but not perfused.
- The clinical picture and chest x-ray findings in this patient are not consistent with pulmonary embolism.
*Normal perfusion with decreased ventilation at the right base*
- While a focal ventilation defect could occur, the patient's symptoms and chest x-ray findings (distended pulmonary veins, Kerley B lines, bilateral blunting of costophrenic angles) suggest **generalized rather than localized pulmonary edema**.
- This option describes a unilateral and focal issue, whereas heart failure typically causes bilateral findings.
*Increased apical ventilation with normal perfusion bilaterally*
- This finding is not typical in any common pulmonary pathology. Increased apical ventilation is not a characteristic of pulmonary edema or other V/Q mismatch disorders.
- This scenario does not align with the patient's symptoms or imaging findings.
Hypoxemia mechanisms US Medical PG Question 9: Two days after undergoing left hemicolectomy for a colonic mass, a 62-year-old man develops shortness of breath. His temperature is 38.1°C (100.6°F), pulse is 80/min, respirations are 22/min, and blood pressure is 120/78 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 88%. Cardiopulmonary examination shows decreased breath sounds and decreased fremitus at both lung bases. Arterial blood gas analysis on room air shows:
pH 7.35
PaO2 70 mm Hg
PCO2 40 mm Hg
An x-ray of the chest shows a collapse of the bases of both lungs. Which of the following is the most likely underlying mechanism of this patient's hypoxemia?
- A. Increased anatomic dead space
- B. Decreased hemoglobin oxygen-binding capacity
- C. Decreased chest wall compliance
- D. Increased tidal volume
- E. Decreased ratio of ventilated alveoli (Correct Answer)
Hypoxemia mechanisms Explanation: ***Decreased ratio of ventilated alveoli***
- The patient's presentation with **shortness of breath**, **decreased breath sounds and fremitus at both lung bases**, and **collapsed lung bases on chest x-ray** points to **atelectasis**.
- **Atelectasis** is a common cause of hypoxemia post-surgery. It occurs when alveoli collapse, leading to areas of the lung that are perfused but not ventilated, resulting in a **ventilation-perfusion (V/Q) mismatch** with a decreased ratio of ventilated alveoli.
*Increased anatomic dead space*
- **Anatomic dead space** refers to the conducting airways where gas exchange does not occur. This value is relatively constant and would not increase significantly to cause such profound hypoxemia in this context.
- Conditions like chronic obstructive pulmonary disease (COPD) can increase dead space, but the patient's acute postoperative presentation and chest X-ray findings do not support this as the primary cause.
*Decreased hemoglobin oxygen-binding capacity*
- This would involve issues like **carbon monoxide poisoning** or specific hemoglobinopathies, which are not indicated by the clinical picture or ABG results (normal pH, PaO2 70 mmHg, PCO2 40 mmHg).
- The PaO2 and SaO2 values indicate a problem with oxygen uptake, not oxygen transport by hemoglobin once bound.
*Decreased chest wall compliance*
- While surgery can cause **pain leading to splinting** and reduced chest wall expansion, which impacts compliance, the primary mechanism of hypoxemia in atelectasis is the **collapse of alveoli**, not solely reduced chest wall movement.
- The **collapsed lung bases** on X-ray directly point to alveolar collapse rather than a general decrease in chest wall compliance as the primary problem.
*Increased tidal volume*
- **Increased tidal volume** would typically improve ventilation and oxygenation, not lead to hypoxemia.
- The patient's **hypoxemia (SaO2 88%, PaO2 70 mmHg)** clearly indicates a problem with oxygen uptake, not an enhancement of respiratory function.
Hypoxemia mechanisms US Medical PG Question 10: A 30-year-old woman presents to the emergency department with breathlessness for the last hour. She is unable to provide any history due to her dyspnea. Her vitals include: respiratory rate 20/min, pulse 100/min, and blood pressure 144/84 mm Hg. On physical examination, she is visibly obese, and her breathing is labored. There are decreased breath sounds and hyperresonance to percussion across all lung fields bilaterally. An arterial blood gas is drawn, and the patient is placed on inhaled oxygen. Laboratory findings reveal:
pH 7.34
pO2 63 mm Hg
pCO2 50 mm Hg
HCO3 22 mEq/L
Her alveolar partial pressure of oxygen is 70 mm Hg. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Right to left shunt
- B. Alveolar hypoventilation (Correct Answer)
- C. Ventricular septal defect
- D. Impaired gas diffusion
- E. Ventilation/perfusion mismatch
Hypoxemia mechanisms Explanation: ***Alveolar hypoventilation***
- The patient exhibits features of **obesity** and **labored breathing** with decreased breath sounds and hyperresonance, along with arterial blood gas results showing **respiratory acidosis** (pH 7.34, pCO2 50 mmHg) and **hypoxia** (pO2 63 mmHg).
- The calculated A-a gradient (Alveolar O2 - arterial O2) is low (70 mmHg - 63 mmHg = 7 mmHg), indicating that the problem is primarily with **overall ventilation** rather than a defect in gas exchange across the alveolar-capillary membrane.
*Right to left shunt*
- A right-to-left shunt would cause a **large A-a gradient**, as deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- While it causes **hypoxemia**, it would not typically be associated with hypercapnia unless very severe, and the A-a gradient calculation here does not support a significant shunt.
*Ventricular septal defect*
- A ventricular septal defect is a **structural heart abnormality** that can cause a left-to-right shunt initially, leading to pulmonary hypertension and eventually a right-to-left shunt (Eisenmenger syndrome).
- While it can cause hypoxemia due to shunting, it would not primarily manifest with increased pCO2 or the specific lung physical exam findings of decreased breath sounds and hyperresonance in the absence of other cardiac signs.
*Impaired gas diffusion*
- Impaired gas diffusion would lead to a **large A-a gradient** and **hypoxemia**, but typically not significant hypercapnia unless the impairment is extremely severe.
- Conditions like **pulmonary fibrosis** or **emphysema** cause impaired diffusion, but the patient's presentation and particularly the low A-a gradient do not support this.
*Ventilation/perfusion mismatch*
- A V/Q mismatch also causes a **large A-a gradient** and **hypoxemia**, as some areas of the lung are either poorly ventilated or poorly perfused.
- While it can cause hypercapnia in severe cases, the primary issue indicated by the low A-a gradient here is one of overall inadequate ventilation, not selective areas of ventilation-perfusion imbalance.
More Hypoxemia mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.