Hemoglobin-oxygen binding US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hemoglobin-oxygen binding. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hemoglobin-oxygen binding US Medical PG Question 1: A 33-year-old woman is brought to the emergency department 30 minutes after being rescued from a fire in her apartment. She reports nausea, headache, and dizziness. Physical examination shows black discoloration of her oral mucosa. Pulse oximetry shows an oxygen saturation of 99% on room air. The substance most likely causing symptoms in this patient primarily produces toxicity by which of the following mechanisms?
- A. Inhibition of mitochondrial complex V
- B. Degradation of 2,3-bisphosphoglycerate
- C. Oxidation of Fe2+
- D. Rise in serum pH
- E. Competitive binding to heme (Correct Answer)
Hemoglobin-oxygen binding Explanation: ***Competitive binding to heme***
- The patient's symptoms (nausea, headache, dizziness, black oral mucosa) and history of being rescued from a fire strongly suggest **carbon monoxide (CO) poisoning** [1].
- **Carbon monoxide** primarily exerts its toxicity by competitively binding to the **heme iron** in hemoglobin with an affinity 200-250 times greater than oxygen, forming **carboxyhemoglobin (COHb)** and displacing oxygen [2].
*Inhibition of mitochondrial complex V*
- **Cyanide poisoning** inhibits **mitochondrial complex IV (cytochrome c oxidase)**, not complex V, leading to impaired cellular respiration.
- While both cyanide and CO poisoning can occur in fires, CO is more common due to incomplete combustion, and the specific presentation points toward CO.
*Degradation of 2,3-bisphosphoglycerate*
- **2,3-BPG** is an important regulator of oxygen affinity for hemoglobin, promoting oxygen release to tissues [2]. Its degradation would increase hemoglobin's affinity for oxygen, thus reducing oxygen unloading, but this is not the primary mechanism of toxicity for CO or common fire-related toxins.
- No common toxin directly causes widespread degradation of 2,3-BPG as its primary mechanism of acute toxicity or symptoms.
*Oxidation of Fe2+*
- The oxidation of **ferrous iron (Fe2+)** to **ferric iron (Fe3+)** in hemoglobin leads to the formation of **methemoglobin**, which cannot bind oxygen. This occurs in **methemoglobinemia** induced by certain drugs or toxins (e.g., nitrites, dapsone).
- While **methemoglobinemia** impairs oxygen transport, it does not explain the black oral mucosa or the strong association with fire smoke toxicity in the context of CO.
*Rise in serum pH*
- A rise in serum pH (alkalosis) is not a direct or primary mechanism of toxicity for common fire-related toxins like carbon monoxide or cyanide.
- Most severe forms of toxicity, including CO and cyanide poisoning, tend to cause **lactic acidosis** due to cellular hypoxia and anaerobic metabolism, leading to a
**decrease** in serum pH.
Hemoglobin-oxygen binding US Medical PG Question 2: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Hemoglobin-oxygen binding Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
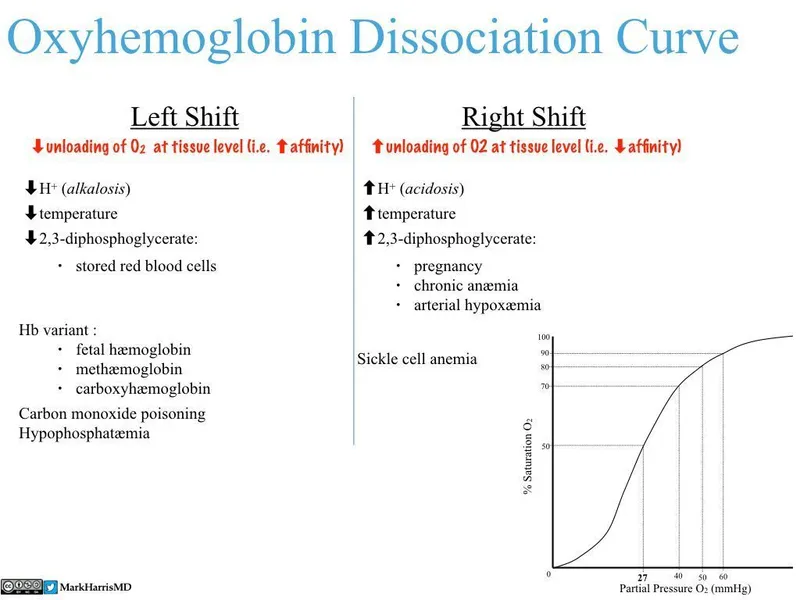
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
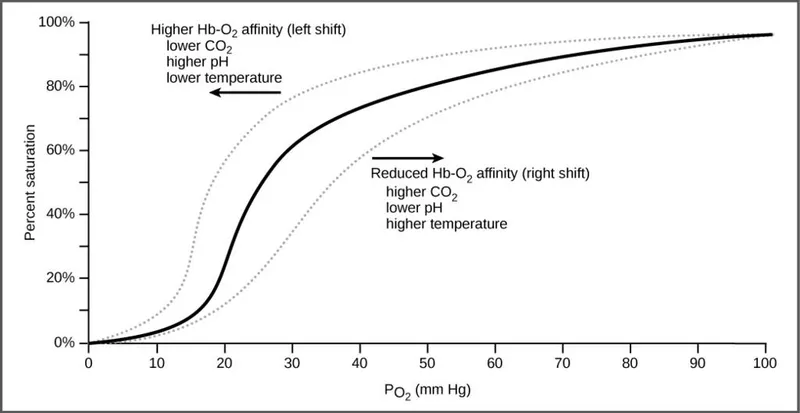
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
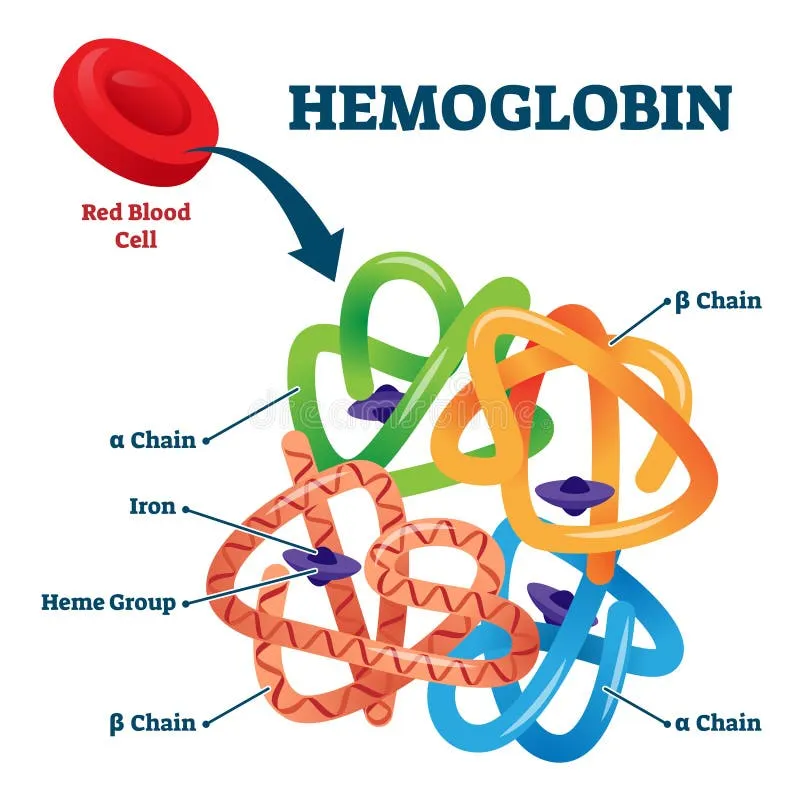
Hemoglobin-oxygen binding US Medical PG Question 3: An investigator is studying the changes that occur in the oxygen-hemoglobin dissociation curve of different types of hemoglobin under various conditions. The blood obtained from a male infant shows decreased affinity for 2,3-bisphosphoglyceric acid. Which of the following is the most likely composition of the hemoglobin molecule in this sample?
- A. α2βS2
- B. α2β2
- C. α2δ2
- D. α2γ2 (Correct Answer)
- E. β4
Hemoglobin-oxygen binding Explanation: ***α2γ2***
- This formula represents **fetal hemoglobin (HbF)**, which is the predominant hemoglobin in infants.
- HbF has **decreased affinity for 2,3-bisphosphoglyceric acid (2,3-BPG)** compared to adult hemoglobin (HbA) because 2,3-BPG binds less avidly to the gamma chains.
- This decreased 2,3-BPG binding results in HbF having **higher oxygen affinity** than HbA (left-shifted oxygen-hemoglobin dissociation curve).
- The higher oxygen affinity allows fetal blood to efficiently extract oxygen from maternal blood across the placenta.
*α2βS2*
- This represents **hemoglobin S (HbS)**, found in **sickle cell disease**.
- HbS has similar 2,3-BPG binding to HbA, not decreased affinity.
- Its primary characteristic is polymerization and red blood cell sickling under deoxygenated conditions.
*α2β2*
- This represents **adult hemoglobin (HbA)**, the most common type of hemoglobin in adults.
- HbA has **higher affinity for 2,3-BPG** compared to HbF because 2,3-BPG binds strongly to the beta chains.
- The binding of 2,3-BPG to HbA decreases oxygen affinity, facilitating oxygen release to tissues.
*α2δ2*
- This represents **hemoglobin A2 (HbA2)**, a minor component of adult hemoglobin (typically <3.5%).
- HbA2 has normal 2,3-BPG binding similar to HbA, not decreased affinity.
- This doesn't fit the clinical description of an infant with decreased 2,3-BPG affinity.
*β4*
- This represents **hemoglobin H (HbH)**, which occurs in **alpha-thalassemia** where there is an excess of beta chains that form tetramers.
- HbH has **extremely high oxygen affinity** and does not release oxygen well to tissues.
- While HbH also has decreased 2,3-BPG binding, it is not found in healthy infants and represents a pathological condition.
Hemoglobin-oxygen binding US Medical PG Question 4: A 45-year-old man is found dead in his garage. His skin appears bright cherry red, and initial toxicology screening reveals elevated carboxyhemoglobin levels. The garage door was closed, and his car's engine was running. During the autopsy, which of the following patterns of lividity would most likely be observed?
- A. Cherry red-colored lividity concentrated in dependent areas (Correct Answer)
- B. Yellow-colored lividity in extremities
- C. Blue-purple lividity in dependent areas
- D. Brown-colored lividity in non-dependent areas
Hemoglobin-oxygen binding Explanation: ***Cherry red-colored lividity concentrated in dependent areas***
- The **bright cherry red skin** and **elevated carboxyhemoglobin levels** are classic signs of **carbon monoxide poisoning**, which causes this specific color of **livor mortis**.
- **Lividity** (livor mortis) occurs in dependent areas due to the gravitational settling of blood after circulation ceases.
*Yellow-colored lividity in extremities*
- **Yellow lividity** is not a typical presentation of **livor mortis** and is not associated with carbon monoxide poisoning.
- While jaundice can cause yellow discoloration, it's a systemic condition, not a post-mortem dependent discoloration.
*Blue-purple lividity in dependent areas*
- **Blue-purple lividity** is the most common presentation of **livor mortis** in cases without carbon monoxide or other specific toxic exposures.
- This color is due to the deoxygenated hemoglobin settling in the capillaries, which is distinct from the **carboxyhemoglobin** seen here.
*Brown-colored lividity in non-dependent areas*
- **Brown lividity** is characteristic of **methemoglobinemia**, a condition where iron in hemoglobin is oxidized, not typical for carbon monoxide poisoning.
- **Lividity** always occurs in **dependent areas** due to gravity, making "non-dependent areas" incorrect for any form of lividity.
Hemoglobin-oxygen binding US Medical PG Question 5: A 48-year-old man is brought to the emergency department 20 minutes after being rescued from a house fire. He reports headache, metallic taste, abdominal pain, and nausea. He appears confused and agitated. His pulse is 125/min, respirations are 33/min, and blood pressure is 100/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination shows a bright red color of the skin. His breath smells of bitter almonds. Hyperbaric oxygen therapy and appropriate pharmacotherapy are initiated. The expected beneficial effect of this drug is most likely due to which of the following mechanisms?
- A. Synthesis of 2,3-bisphosphoglycerate
- B. Formation of methemoglobin (Correct Answer)
- C. Inhibition of cytochrome c oxidase
- D. Dissociation of carboxyhemoglobin
- E. Reduction of ferric iron
Hemoglobin-oxygen binding Explanation: ***Formation of methemoglobin***
- This patient's symptoms (headache, confusion, bright red skin, bitter almond breath, high pulse oximetry despite severe symptoms) are classic for **cyanide poisoning**.
- Many antidotes for cyanide poisoning, such as **nitrites**, work by forming **methemoglobin**, which has a higher affinity for cyanide than cytochrome c oxidase, thus detaching cyanide from the enzyme and allowing cellular respiration to resume.
*Synthesis of 2,3-bisphosphoglycerate*
- **2,3-bisphosphoglycerate (2,3-BPG)** helps regulate oxygen release from hemoglobin in red blood cells.
- While important for oxygen delivery, increasing 2,3-BPG is not a direct therapeutic mechanism for **cyanide poisoning**.
*Inhibition of cytochrome c oxidase*
- **Cyanide** itself inhibits cytochrome c oxidase, leading to cellular hypoxia despite adequate oxygen supply.
- The therapeutic goal is to reverse this inhibition, not to further inhibit the enzyme.
*Dissociation of carboxyhemoglobin*
- **Carbon monoxide poisoning**, not cyanide poisoning, causes carboxyhemoglobin formation and presents with cherry-red skin, but there is no foul-smelling breath.
- Dissociating carboxyhemoglobin is relevant for carbon monoxide poisoning, not cyanide poisoning.
*Reduction of ferric iron*
- Reducing ferric iron (Fe3+) back to ferrous iron (Fe2+) would reverse **methemoglobinemia**, which is often a side effect of some cyanide antidotes.
- The therapeutic strategy for cyanide poisoning involves *inducing* methemoglobinemia to sequester cyanide.
Hemoglobin-oxygen binding US Medical PG Question 6: A man returns home late at night to find his 15-year-old son and 40-year-old wife unconscious in the family room. He immediately summons emergency services. In the field, pulse oximetry shows oxygen saturation at 100% for both patients. 100%, yet they both appear cyanotic. Both patients are provided with 2L of oxygen by way of nasal cannula on the way to the hospital. An arterial blood gas is performed on the teenager and reveals pH of 7.35, PaCO2 of 31.8 mm Hg, PaO2 of 150 mm Hg, HCO3- of 20 mEq/L, SaO2 of 80%, and a COHb of 18%. What is the most likely cause of his condition?
- A. Ischemic hypoxia
- B. Methemoglobinemia
- C. Diffusion-limited hypoxia
- D. Carbon monoxide poisoning (Correct Answer)
- E. Anemic hypoxia
Hemoglobin-oxygen binding Explanation: ***Carbon monoxide poisoning***
- The combination of **cyanosis**, **normal pulse oximetry readings (due to inaccurate readings for CO)**, and a **high COHb level (18%)** is highly indicative of carbon monoxide poisoning.
- Exposure to carbon monoxide forms **carboxyhemoglobin (COHb)**, which has a higher affinity for hemoglobin than oxygen, leading to **tissue hypoxia** despite normal PaO2.
*Ischemic hypoxia*
- This type of hypoxia occurs when there is **reduced blood flow** to a tissue, often due to conditions like **heart failure, shock**, or **arterial occlusion**.
- There is no clinical or lab evidence in the scenario to suggest reduced blood flow as the primary cause of the patient's symptoms.
*Methemoglobinemia*
- While methemoglobinemia can also cause **cyanosis** and an **oxygen saturation gap** (discrepancy between SaO2 and pulse oximetry), it is characterized by a high level of **methemoglobin (MetHb)**.
- The patient's COHb level is elevated at 18%, but there's no information suggesting elevated MetHb, distinguishing it from carbon monoxide poisoning.
*Diffusion-limited hypoxia*
- This occurs when the **diffusion of oxygen from the alveoli to the blood is impaired**, as seen in conditions like **pulmonary fibrosis** or **severe emphysema**.
- The patient's PaO2 of 150 mmHg is very high, indicating excellent oxygen loading in the lungs, which rules out a diffusion limitation.
*Anemic hypoxia*
- Anemic hypoxia results from a **decreased oxygen-carrying capacity of the blood** due to a **low hemoglobin concentration**.
- The scenario does not provide information about the patient's hemoglobin level, and the primary issue is the inability of hemoglobin to release oxygen due to CO binding, not a lack of hemoglobin itself.
Hemoglobin-oxygen binding US Medical PG Question 7: An investigator is conducting a study on hematological factors that affect the affinity of hemoglobin for oxygen. An illustration of two graphs (A and B) that represent the affinity of hemoglobin for oxygen is shown. Which of the following best explains a shift from A to B?
- A. Decreased serum pCO2
- B. Increased serum pH
- C. Decreased serum 2,3-bisphosphoglycerate concentration
- D. Increased body temperature (Correct Answer)
- E. Increased hemoglobin γ-chain synthesis
Hemoglobin-oxygen binding Explanation: ***Increased body temperature***
- A shift from A to B represents a **rightward shift** of the oxygen-hemoglobin dissociation curve, indicating **decreased hemoglobin affinity for oxygen**.
- **Increased body temperature** (e.g., during exercise, fever) reduces hemoglobin's affinity for oxygen, facilitating **oxygen release to tissues**.
*Decreased serum pCO2*
- A **decrease in serum pCO2** leads to an **increase in pH** (alkalosis) and a **leftward shift** of the curve, meaning an increased affinity of hemoglobin for oxygen.
- This is part of the **Bohr effect**, where lower CO2 levels signal decreased tissue metabolic activity, thus reducing oxygen unloading.
*Increased serum pH*
- An **increase in serum pH** (alkalosis) causes a **leftward shift** of the oxygen-hemoglobin dissociation curve, signifying **increased hemoglobin affinity for oxygen**.
- This response is beneficial in the lungs, where higher pH promotes oxygen binding to hemoglobin.
*Decreased serum 2,3-bisphosphoglycerate concentration*
- A **decrease in 2,3-BPG** concentration leads to a **leftward shift** of the curve, representing **increased hemoglobin affinity for oxygen**.
- 2,3-BPG typically binds to deoxyhemoglobin, stabilizing its T-state and promoting oxygen release; thus, less 2,3-BPG means less release.
*Increased hemoglobin γ-chain synthesis*
- Increased **hemoglobin γ-chain synthesis** is characteristic of **fetal hemoglobin (HbF)**, which has a **higher affinity for oxygen** than adult hemoglobin (HbA).
- This would result in a **leftward shift** of the oxygen-hemoglobin dissociation curve, enhancing oxygen uptake by the fetus.
Hemoglobin-oxygen binding US Medical PG Question 8: A 67-year-old man presents to the surgical clinic with swelling of his right leg, fever, and chills for 2 days. The maximum recorded temperature was 38.3°C (101.0°F) at home. His right leg is red and swollen from the dorsum of the foot to the thigh with an ill-defined edge. Venous stasis ulcers are present in both of his limbs, but those on the right have a yellow discharge. His vitals include the following: blood pressure is 120/78 mm Hg, heart rate is 94/min, temperature is 38.3°C (101.0°F), and respiratory rate is 16/min. On physical examination, there is tenderness and warmth compared with his normal leg. Dorsalis pedis pulses are present on both of the ankles. What is the most likely cause of the right shift of the hemoglobin dissociation curve for his condition?
- A. Decrease in temperature
- B. Increase in CO2 production
- C. Increase in pH
- D. Increase in temperature (Correct Answer)
- E. Decrease in 2,3-DPG
Hemoglobin-oxygen binding Explanation: ***Increase in temperature***
- The patient presents with **fever (38.3°C)**, which is explicitly mentioned multiple times in the clinical scenario and represents a **systemic response** to infection.
- **Increased temperature** directly causes a **right shift** in the oxygen-hemoglobin dissociation curve by **decreasing hemoglobin's affinity for oxygen**.
- This facilitates oxygen release to metabolically active tissues, particularly important in areas of infection and inflammation.
- While multiple factors can cause right shifts during infection, the **fever is the most prominently featured clinical finding** in this case and represents a measurable systemic change.
*Decrease in temperature*
- A **decrease in temperature** causes a **left shift** in the oxygen-hemoglobin dissociation curve, **increasing hemoglobin's affinity for oxygen**.
- This would impair oxygen release to tissues, which is counterproductive during infection when tissues require increased oxygen delivery.
*Increase in CO2 production*
- While **increased CO2 production** does occur during infection due to increased tissue metabolism and does cause a **right shift** via the **Bohr effect** (CO2 + H2O → H2CO3 → H+ + HCO3-, leading to decreased pH), this is not the primary factor being highlighted in this clinical presentation.
- The Bohr effect (acidosis from increased CO2 and metabolic acids) is an important physiological response, but the question emphasizes the **fever** as the key feature of this patient's condition.
- In the context of this question asking about "his condition," the **temperature elevation is the most direct and measurable systemic change** presented.
*Increase in pH*
- An **increase in pH** (alkalosis) causes a **left shift** in the oxygen-hemoglobin dissociation curve, **increasing hemoglobin's oxygen affinity**.
- This would hinder oxygen delivery to tissues, which is not beneficial during infection when tissue oxygen demand is elevated.
*Decrease in 2,3-DPG*
- A **decrease in 2,3-bisphosphoglycerate (2,3-DPG)** causes a **left shift** in the oxygen-hemoglobin dissociation curve.
- This increases hemoglobin's affinity for oxygen, making oxygen release to tissues more difficult.
- During infection, 2,3-DPG levels typically remain stable or may increase slightly, not decrease.
Hemoglobin-oxygen binding US Medical PG Question 9: A male infant is born at 27 weeks following premature rupture of membranes and a precipitous labor to a G4P3 female. Given the speed of delivery steroids are not given. Shortly after delivery he develops respiratory distress and the decision is made to administer surfactant replacement therapy. While the components of the surfactant used in surfactant therapy may vary based on institution, what is the main component of pulmonary surfactant produced by type II pneumocytes?
- A. Cholesterol
- B. Protein S
- C. Surfactant-associated proteins
- D. Phospholipids (Correct Answer)
- E. Zinc finger protein
Hemoglobin-oxygen binding Explanation: ***Phospholipids***
- The main component of **pulmonary surfactant** produced by **type II pneumocytes** is **dipalmitoylphosphatidylcholine (DPPC)**, a type of **phospholipid**.
- These **phospholipids** reduce **alveolar surface tension**, preventing alveolar collapse at the end of expiration.
*Cholesterol*
- While **cholesterol** is present in biological membranes, it is a minor component of pulmonary surfactant and does not primarily determine its function.
- Its role is mainly in regulating the fluidity of the **surfactant film**, rather than reducing surface tension.
*Protein S*
- **Protein S** is a **vitamin K-dependent plasma protein** that functions as a **natural anticoagulant**; it is not a component of pulmonary surfactant.
- Its deficiency is associated with **thrombotic disorders**.
*Surfactant-associated proteins*
- **Surfactant-associated proteins (SPs)**, such as SP-A, SP-B, SP-C, and SP-D, are crucial for the **function and regulation** of pulmonary surfactant.
- However, they constitute a much smaller proportion by mass compared to **phospholipids**, which are the main structural and functional components.
*Zinc finger protein*
- **Zinc finger proteins** are a diverse class of proteins that bind to DNA, RNA, or other proteins and are involved in various cellular processes, including **gene regulation**.
- They are not a structural or functional component of **pulmonary surfactant**.
Hemoglobin-oxygen binding US Medical PG Question 10: A 30-year-old woman presents to clinic for a routine checkup. She reports that she is in good health but that she felt short of breath on her hiking and skiing trip to Colorado the week prior. She explains that this was the first time she has gone that high into the mountains and was slightly concerned for the first few days because she felt chronically short of breath. She reports a history of childhood asthma, but this experience did not feel the same. She was on the verge of seeking medical attention, but it resolved three days later, and she has felt fine ever since. What other listed physiological change results in a physiologic alteration similar to that which occurred in this patient?
- A. Increase in partial pressure of water in air
- B. Increase in blood pH
- C. Increase in concentration of dissolved carbon dioxide in blood
- D. Increase in concentration of 2,3-bisphosphoglycerate in blood (Correct Answer)
- E. Decreased body temperature
Hemoglobin-oxygen binding Explanation: ***Increase in concentration of 2,3-bisphosphoglycerate in blood***
- At high altitude, the body **increases 2,3-BPG production** as a key acclimatization mechanism over several days, which is why the patient's symptoms resolved after 3 days.
- Increased 2,3-BPG shifts the **oxygen-hemoglobin dissociation curve to the right**, decreasing hemoglobin's affinity for oxygen and facilitating **oxygen unloading at tissues**.
- This is one of the primary chronic adaptations to high altitude hypoxia, along with increased erythropoietin production.
*Increase in partial pressure of water in air*
- An increase in the partial pressure of water vapor in the air would decrease the partial pressure of inspired oxygen (PiO2 = FiO2 × (Patm - PH2O)).
- This would worsen hypoxia rather than represent an adaptive response to altitude.
*Decreased body temperature*
- Decreased body temperature shifts the oxygen-hemoglobin dissociation curve to the **left**, increasing hemoglobin's affinity for oxygen.
- This would **impair oxygen unloading** at tissues, which is the opposite effect of increased 2,3-BPG.
- This is not a physiological response to high altitude.
*Increase in blood pH*
- An increase in blood pH (respiratory alkalosis) does occur acutely at high altitude due to hyperventilation in response to hypoxia.
- However, this shifts the curve to the **left** (Bohr effect), increasing oxygen affinity, which is the **opposite effect** of increased 2,3-BPG.
- While this occurs as an immediate response, the body compensates through renal bicarbonate excretion and increased 2,3-BPG production to maintain tissue oxygen delivery.
*Increase in concentration of dissolved carbon dioxide in blood*
- At high altitude, hyperventilation leads to **decreased CO2** (hypocapnia), not increased CO2.
- Increased CO2 would cause acidosis and shift the curve to the right (decreasing oxygen affinity), but this does not occur at high altitude.
- The opposite physiological change (decreased CO2) actually occurs.
More Hemoglobin-oxygen binding US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.