Diffusion limitation vs perfusion limitation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diffusion limitation vs perfusion limitation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diffusion limitation vs perfusion limitation US Medical PG Question 1: A research scientist attempts to understand the influence of carbon dioxide content in blood on its oxygen binding. The scientist adds carbon dioxide to dog blood and measures the uptake of oxygen in the blood versus oxygen pressure in the peripheral tissue. He notes in one dog that with the addition of carbon dioxide with a pressure of 90 mmHg, the oxygen pressure in the peripheral tissue rose from 26 to 33 mmHg. How can this phenomenon be explained?
- A. High partial pressure of CO2 in tissues decreases peripheral blood volume
- B. Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin
- C. High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading
- D. High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues (Correct Answer)
- E. The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood
Diffusion limitation vs perfusion limitation Explanation: **High partial pressure of CO2 in tissues facilitates O2 unloading in peripheral tissues**
- An increase in **PCO2** leads to a decrease in pH (acidosis) in the tissues, which **decreases hemoglobin's affinity for oxygen**, promoting oxygen release.
- This phenomenon is known as the **Bohr effect**, where an acidic environment (from CO2) shifts the oxygen dissociation curve to the right, enhancing O2 unloading to meet tissue metabolic demands.
*High partial pressure of CO2 in tissues decreases peripheral blood volume*
- **Increased CO2** generally causes vasodilation in peripheral tissues, which would lead to an **increase**, not a decrease, in peripheral blood flow.
- Decreased blood volume is typically associated with conditions like hypovolemia or intense vasoconstriction, not elevated tissue CO2.
*Binding of O2 to hemoglobin in lungs drives release of CO2 from hemoglobin*
- This statement describes the **Haldane effect**, which occurs primarily in the lungs, where oxygen binding to hemoglobin facilitates the release of CO2.
- While true, it does not explain the **increased oxygen pressure in peripheral tissue** observed with added CO2, which is related to O2 unloading.
*High partial pressure of CO2 in tissues causes alkalemia, which is necessary for O2 unloading*
- High **PCO2** in tissues leads to the formation of carbonic acid and H+ ions, resulting in a **decrease in pH (acidosis)**, not alkalemia.
- **Acidosis** facilitates O2 unloading (Bohr effect), whereas alkalemia would increase hemoglobin's affinity for O2, inhibiting unloading.
*The sum of the partial pressures of CO2 and O2 cannot exceed a known threshold in blood*
- There is **no fixed threshold** for the sum of partial pressures of CO2 and O2 in the blood; these gases are independently regulated and their partial pressures fluctuate with metabolic activity.
- The partial pressure of a gas reflects its concentration and does not have an upper limit when considering the sum of different gases.
Diffusion limitation vs perfusion limitation US Medical PG Question 2: A 60-year-old woman with a history of emphysema has been referred by her pulmonologist for follow-up pulmonary function testing. During the test, the patient reaches a point where her airway pressure is equal to the atmospheric pressure. Which of the following is most likely to be found during this respiratory state?
- A. Pulmonary vascular resistance is at a maximum
- B. Transmural pressure of the lung-chest wall system is at a maximum
- C. Transmural pressure of the chest wall is at a minimum
- D. Pulmonary vascular resistance is at a minimum (Correct Answer)
- E. Transmural pressure of the lung-chest wall system is at a minimum
Diffusion limitation vs perfusion limitation Explanation: ***Pulmonary vascular resistance is at a minimum***
- When airway pressure equals atmospheric pressure during a pulmonary function test, the lungs are at **functional residual capacity (FRC)** or resting state.
- At FRC, **pulmonary vascular resistance (PVR)** is at its lowest point due to the optimal balance between alveolar and extra-alveolar vessel compression/distension.
- Extra-alveolar vessels are compressed at low lung volumes, while alveolar vessels are compressed at high lung volumes. At FRC, both are optimally distended, resulting in **minimal PVR**.
*Pulmonary vascular resistance is at a maximum*
- PVR increases at very low lung volumes (due to extra-alveolar vessel compression) and very high lung volumes (due to alveolar vessel compression).
- The resting state (airway pressure equals atmospheric pressure) corresponds to FRC, where PVR is **minimal, not maximal**.
*Transmural pressure of the lung-chest wall system is at a maximum*
- Transmural pressure of the lung-chest wall system represents the pressure difference across the entire respiratory system.
- This pressure is higher during inspiration or forced expiration when the system is stretched or compressed.
- At FRC (airway pressure equals atmospheric pressure), the system is at **resting equilibrium**, not at maximal transmural pressure.
*Transmural pressure of the chest wall is at a minimum*
- Transmural pressure across the chest wall is the difference between intrapleural pressure and atmospheric pressure.
- This pressure is not at a minimum when airway pressure equals atmospheric pressure.
- Chest wall transmural pressure is actually minimal near **residual volume (RV)**, where the chest wall recoils inward most strongly.
*Transmural pressure of the lung-chest wall system is at a minimum*
- Transmural pressure of the lung-chest wall system reflects the elastic recoil forces of the combined system.
- At FRC (airway pressure equals atmospheric pressure), elastic recoil forces are balanced at equilibrium, but transmural pressure is **not at a minimum**—it represents the neutral resting state.
Diffusion limitation vs perfusion limitation US Medical PG Question 3: A 62-year-old woman with hypertension and type 2 diabetes mellitus comes to the physician because of increasing shortness of breath and a dry cough over the past 6 months. She has smoked 1 pack of cigarettes daily for the past 40 years. Chest auscultation shows scattered expiratory wheezes in both lung fields. Spirometry shows an FEV1:FVC ratio of 65% and an FEV1 of 70% of predicted. Her diffusing capacity for carbon monoxide (DLCO) is 42% of predicted. Which of the following is the most likely diagnosis?
- A. Pulmonary fibrosis
- B. Bronchial asthma
- C. Emphysema (Correct Answer)
- D. Bronchiectasis
- E. Chronic bronchitis
Diffusion limitation vs perfusion limitation Explanation: ***Emphysema***
- The patient's history of **40 pack-years of smoking**, combined with **obstructive lung disease (FEV1:FVC ratio of 65%)** and a **markedly reduced DLCO (42% of predicted)**, strongly indicates emphysema.
- **DLCO reduction** is characteristic of emphysema due to the destruction of alveolar-capillary membranes, which impairs gas exchange.
*Pulmonary fibrosis*
- Pulmonary fibrosis presents with shortness of breath and dry cough, but it is a **restrictive lung disease**, meaning both FEV1 and FVC would be reduced proportionally, leading to a **normal or increased FEV1:FVC ratio**.
- While DLCO is reduced in pulmonary fibrosis, the **obstructive pattern on spirometry** rules out this diagnosis.
*Bronchial asthma*
- Asthma is characterized by **reversible airway obstruction** and often presents with wheezing and shortness of breath.
- However, asthma typically has a **normal DLCO**, as the diffusion capacity of the lung is usually preserved.
*Bronchiectasis*
- Bronchiectasis involves **permanent dilation of the bronchi** and can cause chronic cough, sputum production, and obstructive lung physiology.
- While it can cause some airflow obstruction and reduced DLCO in severe cases, the **primary features often include chronic productive cough** and recurrent infections, and the DLCO reduction is typically less severe than seen in emphysema, unless it's very advanced.
*Chronic bronchitis*
- Chronic bronchitis is defined by a **chronic productive cough** for at least 3 months in each of 2 consecutive years, in a patient for whom other causes have been excluded.
- It causes **obstructive lung disease** and can present with wheezing but typically has a **normal or only slightly reduced DLCO**, as the primary issue is inflammation and mucus production in the airways, not destruction of the alveolar-capillary membrane.
Diffusion limitation vs perfusion limitation US Medical PG Question 4: A 35-year-old man presents to pulmonary function clinic for preoperative evaluation for a right pneumonectomy. His arterial blood gas at room air is as follows:
pH: 7.34
PaCO2: 68 mmHg
PaO2: 56 mmHg
Base excess: +1
O2 saturation: 89%
What underlying condition most likely explains these findings?
- A. Cystic fibrosis
- B. Bronchiectasis
- C. Chronic obstructive pulmonary disease (Correct Answer)
- D. Obesity
- E. Acute respiratory distress syndrome
Diffusion limitation vs perfusion limitation Explanation: ***Chronic obstructive pulmonary disease***
- This patient exhibits **compensated respiratory acidosis** (low pH, high PaCO2, slightly elevated base excess) and **hypoxemia** (low PaO2), which are characteristic findings in chronic obstructive pulmonary disease (COPD) with underlying respiratory failure.
- The history of a planned **pneumonectomy** also suggests a significant pre-existing lung pathology often seen in patients with severe COPD.
*Cystic fibrosis*
- While cystic fibrosis can lead to chronic lung disease, it typically presents at a younger age and is associated with a history of recurrent infections and exocrine gland dysfunction.
- While it can manifest similarly in ABG, the age and the planned pneumonectomy make COPD a more likely primary cause in this context.
*Bronchiectasis*
- Bronchiectasis involves permanent dilation of the bronchi, often leading to chronic cough, sputum production, and recurrent infections.
- While it can cause respiratory compromise, the ABG findings are more classically associated with the widespread air trapping and V/Q mismatch seen in COPD.
*Obesity*
- Severe obesity can lead to **obesity hypoventilation syndrome**, presenting with hypercapnia and hypoxemia.
- However, the patient's age and the context of a planned pneumonectomy make an underlying primary lung disease like COPD a more focused explanation for the ABG pattern.
*Acute respiratory distress syndrome*
- Acute respiratory distress syndrome (ARDS) is an **acute** and severe form of respiratory failure characterized by severe hypoxemia and bilateral opacities on chest imaging.
- The ABG findings in ARDS typically show **severe hypoxemia** with **respiratory alkalosis** early on, evolving to acidosis, and it is an acute process, not a chronic pre-existing condition suitable for elective surgery.
Diffusion limitation vs perfusion limitation US Medical PG Question 5: A 14-year-old boy is brought to the emergency department by his mom after she found him complaining of headaches, nausea, lightheadedness, and muscle pain. He has had type I diabetes for 3 years with very well managed blood sugars, and he is otherwise healthy. He recently returned from a boy scout skiing trip where he drank from a mountain stream, ate unusual foods, and lived in a lodge with a wood-fired fireplace and cooking stove. On physical exam he has a diffuse redness of his skin. Which of the following changes to this patient's pulmonary system would cause oxygen to exhibit similar tissue hypoxia effects as the most likely cause of this patient's symptoms?
- A. Increasing capillary length
- B. Nitrous oxide administration
- C. Increasing capillary transit time
- D. Interstitial thinning
- E. Interstitial fibrosis (Correct Answer)
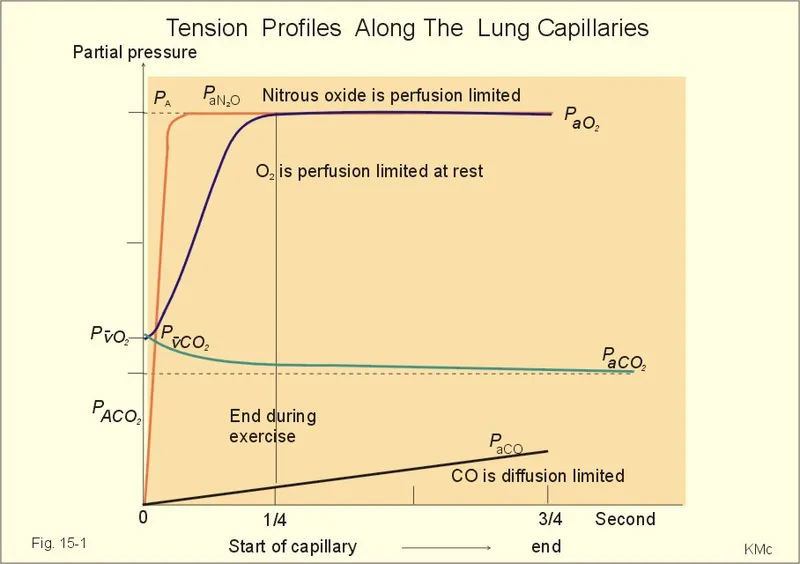
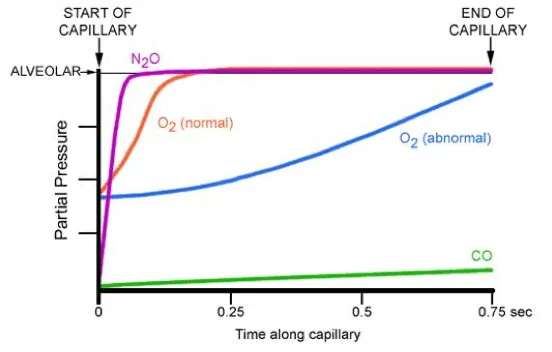
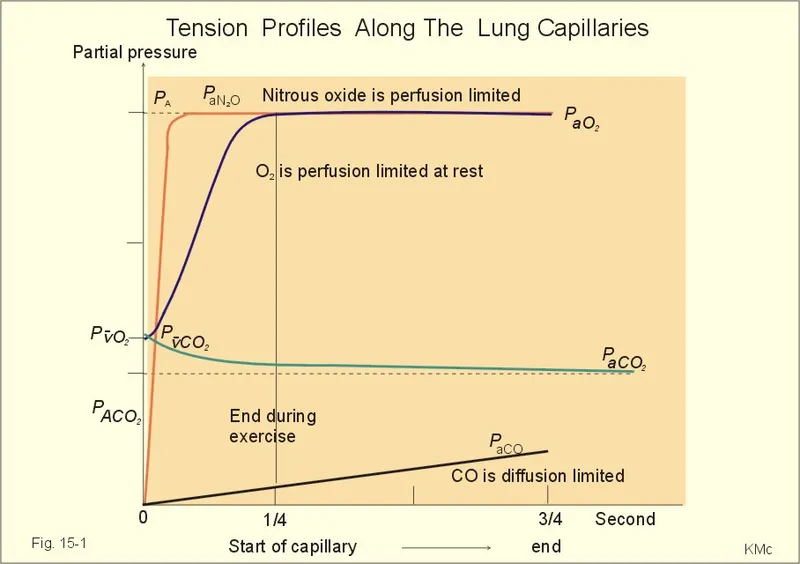
Diffusion limitation vs perfusion limitation Explanation: ***Interstitial fibrosis***
- Carbon monoxide poisoning causes tissue hypoxia by reducing **oxygen-carrying capacity** (CO binds hemoglobin with high affinity, maintaining normal PaO2 but severely reducing oxygen content and delivery to tissues).
- Among the pulmonary changes listed, interstitial fibrosis most closely produces **tissue hypoxia** by impairing oxygen transfer across the thickened alveolar-capillary membrane, resulting in **hypoxemia and reduced tissue oxygen delivery**.
- While the mechanisms differ (CO affects carrying capacity vs. fibrosis affects diffusion), both ultimately result in inadequate oxygen delivery to meet tissue metabolic demands, manifesting as tissue hypoxia.
- Interstitial fibrosis creates a **diffusion barrier** that worsens with increased oxygen demand (exercise), similar to how CO poisoning impairs the ability to meet tissue oxygen requirements.
*Increasing capillary length*
- Increasing capillary length would **improve gas exchange** by providing more surface area and time for oxygen diffusion across the alveolar-capillary membrane.
- This adaptation enhances oxygen delivery to tissues, which is the opposite of the tissue hypoxia seen in CO poisoning.
*Nitrous oxide administration*
- Nitrous oxide is an anesthetic gas that acts primarily on the **central nervous system** and does not significantly impair oxygen transport or binding to hemoglobin.
- While it can displace oxygen at very high concentrations, its mechanism does not mimic the impaired oxygen delivery characteristic of CO poisoning.
*Increasing capillary transit time*
- Increased capillary transit time allows **more time for oxygen equilibration** between alveolar gas and capillary blood, thereby improving oxygenation.
- This would enhance tissue oxygen delivery rather than cause tissue hypoxia, opposite to the effect of CO poisoning.
*Interstitial thinning*
- Interstitial thinning **decreases the diffusion distance** for oxygen, facilitating more efficient gas exchange across the alveolar-capillary membrane.
- This would improve oxygen delivery to tissues and is the opposite of what occurs in CO poisoning.
Diffusion limitation vs perfusion limitation US Medical PG Question 6: A 72-year-old obese man presents as a new patient to his primary care physician because he has been feeling tired and short of breath after recently moving to Denver. He is a former 50 pack-year smoker and has previously had deep venous thrombosis. Furthermore, he previously had a lobe of the lung removed due to lung cancer. Finally, he has a family history of a progressive restrictive lung disease. Laboratory values are obtained as follows:
Oxygen tension in inspired air = 130 mmHg
Alveolar carbon dioxide tension = 48 mmHg
Arterial oxygen tension = 58 mmHg
Respiratory exchange ratio = 0.80
Respiratory rate = 20/min
Tidal volume = 500 mL
Which of the following mechanisms is consistent with these values?
- A. Shunt physiology
- B. High altitude
- C. V/Q mismatch
- D. Pulmonary fibrosis
- E. Hypoventilation (Correct Answer)
Diffusion limitation vs perfusion limitation Explanation: ***Hypoventilation***
- The arterial oxygen tension (PaO2) of 58 mmHg is consistent with hypoxemia, and the alveolar carbon dioxide tension (PACO2) of 48 mmHg (normal 35-45 mmHg) indicates **hypercapnia**, a hallmark of hypoventilation.
- The **alveolar-arterial (A-a) gradient** can be calculated using the alveolar gas equation: PAO2 = PiO2 - PACO2/R. Here, PAO2 = 130 mmHg - 48 mmHg/0.8 = 130 - 60 = 70 mmHg. The A-a gradient is PAO2 - PaO2 = 70 - 58 = 12 mmHg, which is within the normal range (5-15 mmHg), indicating that the hypoxemia is primarily due to **decreased alveolar ventilation**.
*Shunt physiology*
- A shunt would cause a significant reduction in PaO2 and a **widened A-a gradient** (typically >15 mmHg) due to deoxygenated blood bypassing ventilated areas.
- While shunts do not typically cause hypercapnia unless very severe, the normal A-a gradient here rules out a significant shunt as the primary mechanism for hypoxemia.
*High altitude*
- Moving to a high altitude (like Denver) causes a decrease in **inspired oxygen tension (PiO2)**, leading to hypoxemia.
- However, the provided inspired oxygen tension (130 mmHg) is above what would be expected for significant high-altitude hypoxemia at sea level equivalent, and the hypoxemia here is associated with hypercapnia, which is not a direct result of high altitude itself.
*V/Q mismatch*
- A V/Q mismatch leads to hypoxemia and a **widened A-a gradient**, as some areas of the lung are either underventilated or underperfused.
- While it can cause hypoxemia, a V/Q mismatch is typically associated with **normal or low PaCO2** due to compensatory hyperventilation, not hypercapnia, and the A-a gradient would be elevated.
*Pulmonary fibrosis*
- Pulmonary fibrosis is a restrictive lung disease that leads to impaired gas exchange, causing hypoxemia primarily due to **V/Q mismatch** and **diffusion limitation**.
- This would result in a **widened A-a gradient** and often a **low PaCO2** due to compensatory hyperventilation, rather than the elevated PaCO2 observed in this patient.
Diffusion limitation vs perfusion limitation US Medical PG Question 7: A 22-year-old woman presents to the emergency department with a chief concern of shortness of breath. She was hiking when she suddenly felt unable to breathe and had to take slow deep breaths to improve her symptoms. The patient is a Swedish foreign exchange student and does not speak any English. Her past medical history and current medications are unknown. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 90% on room air. Physical exam is notable for poor air movement bilaterally and tachycardia. The patient is started on treatment. Which of the following best describes this patient's underlying pathology?
FEV1 = Forced expiratory volume in 1 second
FVC = Forced vital capacity
DLCO = Diffusing capacity of carbon monoxide
- A. Increased FVC
- B. Increased FEV1
- C. Increased FEV1/FVC
- D. Decreased airway tone
- E. Normal DLCO (Correct Answer)
Diffusion limitation vs perfusion limitation Explanation: ***Normal DLCO***
- This patient presents with an acute exacerbation of what is likely **asthma**, showing symptoms of **shortness of breath**, **tachycardia**, poor air movement bilaterally, and improvement with slow deep breaths. **Asthma** characteristically affects the airways and not the alveoli, thus the **diffusing capacity of carbon monoxide (DLCO)**, which measures gas exchange across the alveolar-capillary membrane, would be expected to be normal.
- In asthma, the primary problem is **bronchoconstriction** and **airway inflammation**, which restricts airflow but does not typically impair the diffusion of gases like carbon monoxide across the alveolar-capillary membrane.
*Increased FVC*
- **Forced vital capacity (FVC)** is often normal or even slightly reduced in asthma due to **air trapping** and early airway closure, not increased.
- An increased FVC is usually not associated with obstructive lung diseases like asthma but could potentially be seen in conditions where lung volumes are pathologically large, which is not the case here.
*Increased FEV1*
- **Forced expiratory volume in 1 second (FEV1)** is typically **decreased** in obstructive lung diseases like asthma due to **airflow limitation**.
- An increased FEV1 would indicate better-than-average expiratory flow, which contradicts the symptoms of shortness of breath and poor air movement in this patient.
*Increased FEV1/FVC*
- The **FEV1/FVC ratio** is characteristically **decreased** in obstructive lung diseases like asthma, indicating that a disproportionately smaller amount of air can be exhaled in the first second relative to the total forced vital capacity.
- An increased FEV1/FVC ratio would be a sign of a restrictive lung disease or normal lung function, not an exacerbation of an obstructive process.
*Decreased airway tone*
- The underlying pathology in asthma is typically **bronchoconstriction**, which means an **increased airway tone** and narrowing of the airways, rather than decreased.
- Decreased airway tone would imply bronchodilation, which would alleviate, not cause, the patient's symptoms of shortness of breath and poor air movement.
Diffusion limitation vs perfusion limitation US Medical PG Question 8: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Diffusion limitation vs perfusion limitation Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Diffusion limitation vs perfusion limitation US Medical PG Question 9: A 19-year-old male soccer player undergoes an exercise tolerance test to measure his maximal oxygen uptake during exercise. Which of the following changes are most likely to occur during exercise?
- A. Increased apical ventilation-perfusion ratio
- B. Decreased physiologic dead space (Correct Answer)
- C. Decreased alveolar-arterial oxygen gradient
- D. Increased arterial partial pressure of oxygen
- E. Increased pulmonary vascular resistance
Diffusion limitation vs perfusion limitation Explanation: **Decreased physiologic dead space**
- During exercise, there is improved perfusion to previously underperfused areas of the lung, leading to a **more uniform ventilation-perfusion (V/Q) matching** and thus a decrease in physiologic dead space.
- The increased cardiac output helps to perfuse more capillaries, reducing the amount of ventilated air that does not participate in gas exchange.
*Increased apical ventilation-perfusion ratio*
- At rest, the **apical V/Q ratio is already high** due to gravity-dependent differences in blood flow; exercise partially normalizes these differences.
- While overall V/Q matching improves, the relative V/Q differences between apical and basal regions may become less pronounced, not necessarily a further increase in the apical ratio.
*Decreased alveolar-arterial oxygen gradient*
- During severe exercise, the **A-a gradient often increases slightly** due to increased oxygen diffusion limitations and V/Q mismatch.
- Although overall gas exchange efficiency improves, the sheer volume of oxygen demand can reveal small imbalances, rather than fully eliminating the gradient.
*Increased arterial partial pressure of oxygen*
- Exercise typically leads to **stable or slightly decreased arterial PO2** in healthy individuals due to the increased metabolic demand and potential small V/Q mismatches.
- The body maintains arterial PO2 remarkably well even at high exertion, but it does not usually significantly increase.
*Increased pulmonary vascular resistance*
- During exercise, **pulmonary vascular resistance (PVR) generally decreases** due to recruitment and distension of pulmonary capillaries.
- This decrease in PVR helps to accommodate the increased cardiac output without a significant rise in pulmonary arterial pressure.
Diffusion limitation vs perfusion limitation US Medical PG Question 10: A 58-year-old woman comes to the physician because of a 2-year history of progressively worsening pain in her knees and fingers. The knee pain is worse when she walks for longer than 30 minutes. When she wakes up in the morning, her fingers and knees are stiff for about 15 minutes. She cannot recall any trauma to the joints. She was treated with amoxicillin following a tick bite 2 years ago. She is otherwise healthy and only takes a multivitamin and occasionally acetaminophen for the pain. She drinks 1–2 glasses of wine daily. She is 160 cm (5 ft 3 in) tall and weighs 79 kg (174 lb); BMI is 31 kg/m2. Her temperature is 36.9°C (98.4°F), pulse is 70/min, and blood pressure is 133/78 mm Hg. Examination of the lower extremities reveals mild genu varum. Range of motion of both knees is limited; there is palpable crepitus. Complete flexion and extension elicit pain. Tender nodules are present on the proximal and distal interphalangeal joints of the index, ring, and little fingers bilaterally. Which of the following is the most likely diagnosis?
- A. Septic arthritis
- B. Lyme arthritis
- C. Gout
- D. Pseudogout
- E. Osteoarthritis (Correct Answer)
Diffusion limitation vs perfusion limitation Explanation: ***Osteoarthritis***
- The patient's presentation with **joint pain worse with activity**, **morning stiffness lasting less than 30 minutes**, **crepitus**, **limited range of motion**, **obesity**, and involvement of **DIP and PIP joints** (Heberden's and Bouchard's nodes) is classic for **osteoarthritis**.
- **Genu varum** (bow-leggedness) is also a common feature of long-standing knee osteoarthritis.
*Septic arthritis*
- Septic arthritis typically presents acutely with **severe, acute pain**, swelling, warmth, and systemic symptoms like **fever and chills**, which are absent here.
- It usually affects a **single joint** and is unlikely to present with chronic, bilateral, and polyarticular involvement over two years.
*Lyme arthritis*
- While the patient had a tick bite and received amoxicillin, **Lyme arthritis** often presents with **monoarticular** or **oligoarticular** large joint involvement, typically the knee, and usually has more significant effusions.
- The chronic, progressive, and polyarticular nature involving DIPs and PIPs, along with short morning stiffness, is not typical for Lyme arthritis.
*Gout*
- Gout typically presents with **acute, excruciating pain** in a single joint (often the **first MTP joint**), intense inflammation, and rapid resolution of attacks.
- The patient's chronic, symmetrical, and progressive pain, and morning stiffness are inconsistent with the typical presentation of gout.
*Pseudogout*
- Pseudogout (calcium pyrophosphate deposition disease) typically presents as **acute attacks** of pain and swelling, often in larger joints like the knee, wrist or shoulder, similar to gout.
- While it can involve multiple joints, the chronic, progressive nature with specific involvement of DIPs and PIPs with osteoarthritic features (crepitus, activity-related pain, short morning stiffness) is more consistent with osteoarthritis.
More Diffusion limitation vs perfusion limitation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.