Altitude physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Altitude physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Altitude physiology US Medical PG Question 1: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Altitude physiology Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
Altitude physiology US Medical PG Question 2: What is the primary stimulus for erythropoietin production?
- A. Increased temperature
- B. Decreased blood pressure
- C. Decreased plasma proteins
- D. Tissue hypoxia (Correct Answer)
Altitude physiology Explanation: ***Tissue hypoxia***
- Erythropoietin (EPO) production is primarily stimulated by sensing **low oxygen levels** in the kidneys.
- This response is crucial for maintaining adequate oxygen delivery to tissues by increasing **red blood cell mass**.
*Increased temperature*
- An increase in body temperature is a stimulus for processes like **sweating** and **vasodilation**, to regulate body temperature.
- It does not directly affect erythropoietin production or red blood cell synthesis.
*Decreased blood pressure*
- A decrease in blood pressure primarily stimulates the **renin-angiotensin-aldosterone system** and the release of **ADH** to regulate blood volume and pressure.
- It does not directly cause an increase in erythropoietin release as its primary function is not related to oxygen sensing.
*Decreased plasma proteins*
- A decrease in plasma proteins primarily affects **oncotic pressure** and can lead to edema.
- It is not a direct stimulus for erythropoietin production.
Altitude physiology US Medical PG Question 3: A healthy 20-year-old male college student attempts to climb Mount Everest and travels to the Tibetan plateau by plane. Upon landing, he feels increasingly dizzy and fatigued. He notices that he is breathing faster than usual. What is the initial stimulus for the most likely acid-base disorder?
- A. Decreased partial pressure of alveolar oxygen (Correct Answer)
- B. Undiagnosed atrial septal defect
- C. Increasing arterial partial pressure of carbon dioxide
- D. Worsened diffusion limitation of oxygen
- E. Hypoxic pulmonary vasoconstriction
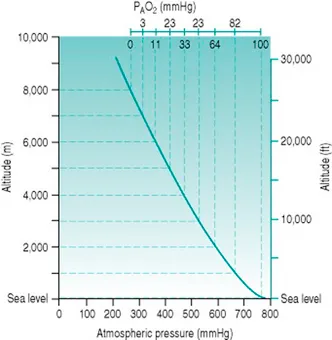
Altitude physiology Explanation: ***Decreased partial pressure of alveolar oxygen***
- Upon rapid ascent to high altitude (like the Tibetan plateau), the ambient atmospheric pressure decreases, leading to a significant drop in the **partial pressure of inspired oxygen (PiO2)**.
- This reduction in PiO2 directly causes a decrease in the **partial pressure of alveolar oxygen (PAO2)**, which is the primary stimulus for activation of peripheral chemoreceptors, leading to hyperventilation and a respiratory alkalosis.
*Undiagnosed atrial septal defect*
- An atrial septal defect (ASD) would cause a **left-to-right shunt** in a healthy young adult, not typically presenting with acute dizziness and fatigue immediately upon high-altitude exposure.
- While an ASD can lead to cyanosis and dyspnea with exertion, it would not be the initial stimulus for the observed hyperventilation response to high altitude.
*Increasing arterial partial pressure of carbon dioxide*
- An increasing **arterial partial pressure of carbon dioxide (PaCO2)** would stimulate central chemoreceptors and increase ventilation, but it is not the initial trigger in this scenario.
- In response to **hypoxia** at high altitude, the body *hyperventilates*, which would lead to a *decrease* in PaCO2, not an increase.
*Worsened diffusion limitation of oxygen*
- **Diffusion limitation** of oxygen refers to impaired gas exchange across the alveolar-capillary membrane, usually due to conditions like fibrosis or edema.
- While gas exchange can be affected at extreme altitudes, it is not the primary initial physiological trigger for the body's acute response (hyperventilation) in a healthy individual.
*Hypoxic pulmonary vasodilation*
- **Hypoxic pulmonary vasoconstriction** (not vasodilation) is a physiological response in the lungs where pulmonary arterioles constrict in areas of low oxygen, redirecting blood flow to better-ventilated areas.
- This mechanism aims to optimize V/Q matching and is a *response* to hypoxia, not the initial stimulus for the systemic acid-base derangement leading to symptoms like dizziness and increased breathing rate.
Altitude physiology US Medical PG Question 4: A 34-year-old woman comes to a physician for a routine health maintenance examination. She moved to Denver 1 week ago after having lived in New York City all her life. She has no history of serious illness and takes no medications. Which of the following sets of changes is most likely on analysis of a blood sample obtained now compared to prior to her move?
Erythropoietin level | O2 saturation | Plasma volume
- A. ↑ unchanged unchanged
- B. ↑ ↓ ↓ (Correct Answer)
- C. Unchanged ↓ unchanged
- D. ↓ unchanged ↑
- E. Unchanged unchanged ↓
Altitude physiology Explanation: ***↑ ↓ ↓***
- Moving to a high altitude like Denver (from sea level NYC) leads to **hypoxia**, which triggers increased **erythropoietin (EPO)** production to stimulate red blood cell formation.
- The immediate physiological response to high altitude is a **decrease in arterial PO2** and thus **oxygen saturation**, along with a **reduction in plasma volume** due to increased diuresis and fluid shifts.
*↑ unchanged unchanged*
- While **erythropoietin** would increase due to hypoxia at higher altitudes, **oxygen saturation** would decrease, not remain unchanged.
- **Plasma volume** also tends to decrease acutely at high altitudes, rather than staying unchanged.
*Unchanged ↓ unchanged*
- **Erythropoietin** would be expected to increase, not remain unchanged, as a compensatory mechanism to hypoxia.
- While **oxygen saturation** would decrease, **plasma volume** typically decreases acutely, not remaining unchanged.
*↓ unchanged ↑*
- **Erythropoietin** would increase, not decrease, in response to the lower atmospheric oxygen.
- Both **oxygen saturation** and **plasma volume** would decrease, not remain unchanged or increase, respectively.
*Unchanged unchanged ↓*
- **Erythropoietin** would increase, not remain unchanged, to stimulate red blood cell production in response to hypoxia.
- **Oxygen saturation** would decrease, not remain unchanged, at higher altitudes.
Altitude physiology US Medical PG Question 5: A 27-year-old man presents to the emergency department after being hit by a car while riding his bike. The patient was brought in with his airway intact, vitals stable, and with a C-collar on. Physical exam is notable for bruising over the patient’s head and a confused man with a Glasgow coma scale of 11. It is noticed that the patient has a very irregular pattern of breathing. Repeat vitals demonstrate his temperature is 97.5°F (36.4°C), blood pressure is 172/102 mmHg, pulse is 55/min, respirations are 22/min and irregular, and oxygen saturation is 94% on room air. Which of the following interventions are most likely to improve this patient's vital signs?
- A. Head elevation, sedation, hypertonic saline, hypoventilation
- B. Lower head, sedation, hypertonic saline, hypoventilation
- C. Head elevation, sedation, mannitol, hyperventilation (Correct Answer)
- D. Head elevation, norepinephrine, mannitol, hyperventilation
- E. Lower head, sedation, hypertonic saline, hyperventilation
Altitude physiology Explanation: ***Head elevation, sedation, mannitol, hyperventilation***
- This patient presents with signs of **increased intracranial pressure (ICP)**, indicated by **Cushing's triad** (hypertension, bradycardia, irregular respirations) and a decreased Glasgow Coma Scale (GCS) after head trauma. **Head elevation** to 30 degrees promotes venous outflow from the brain, reducing ICP.
- **Sedation** lowers metabolic demand and reduces agitation, which can otherwise increase ICP. **Mannitol** is an osmotic diuretic that rapidly draws fluid from the brain, decreasing cerebral edema. **Hyperventilation** temporarily reduces ICP by causing cerebral vasoconstriction through decreased pCO2.
*Head elevation, sedation, hypertonic saline, hypoventilation*
- While **head elevation**, **sedation**, and **hypertonic saline** (an alternative osmotic agent to mannitol) are appropriate for ICP management, **hypoventilation** would increase pCO2, causing cerebral vasodilation and worsening ICP.
- The combination of effective and ineffective ICP-reducing strategies makes this an incorrect option.
*Lower head, sedation, hypertonic saline, hypoventilation*
- **Lowering the head** would impede venous drainage from the brain and increase ICP, which is detrimental in this scenario.
- As mentioned, **hypoventilation** is contraindicated as it exacerbates cerebral edema and elevated ICP.
*Head elevation, norepinephrine, mannitol, hyperventilation*
- While **head elevation**, **mannitol**, and **hyperventilation** are appropriate, **norepinephrine** is primarily used to treat hypotension and maintain cerebral perfusion pressure (CPP) if blood pressure is dangerously low.
- In this case, the patient is hypertensive (**blood pressure 172/102 mmHg**), so norepinephrine would further increase blood pressure and ICP.
*Lower head, sedation, hypertonic saline, hyperventilation*
- **Lowering the head** is contraindicated as it directly increases ICP by hindering venous outflow from the brain.
- Although **sedation**, **hypertonic saline**, and **hyperventilation** are useful for ICP control, the incorrect positioning makes this option less suitable.
Altitude physiology US Medical PG Question 6: A 37-year-old G1P0 woman presents to her primary care physician for a routine checkup. She has a history of diabetes and hypertension but has otherwise been healthy with no change in her health status since the last visit. She is expecting her first child 8 weeks from now. She also enrolled in a study about pregnancy where serial metabolic panels and arterial blood gases are obtained. Partial results from these studies are shown below:
Serum:
Na+: 141 mEq/L
Cl-: 108 mEq/L
pH: 7.47
pCO2: 30 mmHg
HCO3-: 21 mEq/L
Which of the following disease processes would most likely present with a similar panel of metabolic results?
- A. Diarrheal disease
- B. Loop diuretic abuse
- C. Living at high altitude (Correct Answer)
- D. Ingestion of metformin
- E. Anxiety attack
Altitude physiology Explanation: ***Living at high altitude***
- Chronic exposure to **high altitude** leads to sustained **hypoxia**, which stimulates **hyperventilation** as a compensatory mechanism.
- This persistent hyperventilation causes a **respiratory alkalosis** (high pH, low pCO2) and a compensatory **metabolic acidosis** (low HCO3-) to normalize pH, mimicking the presented metabolic panel.
*Diarrheal disease*
- Severe **diarrhea** leads to the loss of bicarbonate from the gastrointestinal tract, causing a **non-anion gap metabolic acidosis**.
- This would present with a **low pH**, **low HCO3-**, and a **compensatory drop in pCO2**, not a respiratory alkalosis with a high pH.
*Loop diuretic abuse*
- Chronic abuse of **loop diuretics** can cause **metabolic alkalosis** due to increased renal excretion of hydrogen ions and potassium, leading to volume contraction.
- This would typically present with a **high pH**, high HCO3-, and a compensatory rise in pCO2, which is different from the given values.
*Ingestion of metformin*
- **Metformin** can cause **lactic acidosis** (a type of high anion gap metabolic acidosis), especially in patients with renal impairment.
- This would manifest as a **low pH**, **low HCO3-**, and a **compensatory decrease in pCO2**, along with an elevated anion gap, not the respiratory alkalosis seen here.
*Anxiety attack*
- An **anxiety attack** causes acute **hyperventilation**, leading to **acute respiratory alkalosis** (high pH, low pCO2).
- However, in an acute setting, there is insufficient time for significant renal compensation, so the HCO3- would remain near normal, unlike the compensated state shown in the panel.
Altitude physiology US Medical PG Question 7: A 25-year-old man is in the middle of an ascent up a mountain, at an elevation of about 4,500 meters. This is the 4th day of his expedition. His friend notices that in the last few hours, he has been coughing frequently and appears to be short of breath. He has used his albuterol inhaler twice in the past 4 hours, but it does not seem to help. Within the past hour, he has coughed up some frothy, slightly pink sputum and is now complaining of nausea and headache. Other than his asthma, which has been well-controlled on a steroid inhaler, he is healthy. Which of the following is the most likely cause of this man’s symptoms?
- A. An acute asthma exacerbation
- B. Non-cardiogenic pulmonary edema (Correct Answer)
- C. Pneumothorax
- D. Pulmonary embolism
- E. Acute heart failure
Altitude physiology Explanation: ***Non-cardiogenic pulmonary edema***
- The patient's symptoms of **dyspnea**, cough, and **frothy, pink sputum** at high altitude (4,500 meters) are classic signs of **High-Altitude Pulmonary Edema (HAPE)**, a form of non-cardiogenic pulmonary edema.
- The headache and nausea are consistent with **acute mountain sickness**, which often precedes HAPE, and the ineffectiveness of albuterol points away from asthma.
*An acute asthma exacerbation*
- While the patient has a history of asthma, the **frothy, pink sputum** is atypical for asthma and strongly suggests alveolar fluid.
- The ineffectiveness of albuterol, a bronchodilator, further suggests a cause other than **bronchoconstriction** as the primary issue.
*Pneumothorax*
- A pneumothorax typically presents with **sudden onset unilateral pleuritic chest pain** and dyspnea, which can be severe.
- It would not usually cause frothy, pink sputum and is not directly linked to high altitude in the absence of trauma.
*Pulmonary embolism*
- A pulmonary embolism often causes **sudden onset dyspnea, pleuritic chest pain, and sometimes hemoptysis**, but **pink, frothy sputum** is less common.
- There are no risk factors for PE mentioned, such as prolonged immobility or recent surgery.
*Acute heart failure*
- While acute heart failure can cause **pulmonary edema with frothy, pink sputum**, the patient is a young, otherwise healthy man with no cardiac risk factors.
- The context of **high altitude** strongly points to HAPE over acute heart failure as the cause of pulmonary edema.
Altitude physiology US Medical PG Question 8: An investigator is conducting a study on hematological factors that affect the affinity of hemoglobin for oxygen. An illustration of two graphs (A and B) that represent the affinity of hemoglobin for oxygen is shown. Which of the following best explains a shift from A to B?
- A. Decreased serum pCO2
- B. Increased serum pH
- C. Decreased serum 2,3-bisphosphoglycerate concentration
- D. Increased body temperature (Correct Answer)
- E. Increased hemoglobin γ-chain synthesis
Altitude physiology Explanation: ***Increased body temperature***
- A shift from A to B represents a **rightward shift** of the oxygen-hemoglobin dissociation curve, indicating **decreased hemoglobin affinity for oxygen**.
- **Increased body temperature** (e.g., during exercise, fever) reduces hemoglobin's affinity for oxygen, facilitating **oxygen release to tissues**.
*Decreased serum pCO2*
- A **decrease in serum pCO2** leads to an **increase in pH** (alkalosis) and a **leftward shift** of the curve, meaning an increased affinity of hemoglobin for oxygen.
- This is part of the **Bohr effect**, where lower CO2 levels signal decreased tissue metabolic activity, thus reducing oxygen unloading.
*Increased serum pH*
- An **increase in serum pH** (alkalosis) causes a **leftward shift** of the oxygen-hemoglobin dissociation curve, signifying **increased hemoglobin affinity for oxygen**.
- This response is beneficial in the lungs, where higher pH promotes oxygen binding to hemoglobin.
*Decreased serum 2,3-bisphosphoglycerate concentration*
- A **decrease in 2,3-BPG** concentration leads to a **leftward shift** of the curve, representing **increased hemoglobin affinity for oxygen**.
- 2,3-BPG typically binds to deoxyhemoglobin, stabilizing its T-state and promoting oxygen release; thus, less 2,3-BPG means less release.
*Increased hemoglobin γ-chain synthesis*
- Increased **hemoglobin γ-chain synthesis** is characteristic of **fetal hemoglobin (HbF)**, which has a **higher affinity for oxygen** than adult hemoglobin (HbA).
- This would result in a **leftward shift** of the oxygen-hemoglobin dissociation curve, enhancing oxygen uptake by the fetus.
Altitude physiology US Medical PG Question 9: A 67-year-old man presents to the surgical clinic with swelling of his right leg, fever, and chills for 2 days. The maximum recorded temperature was 38.3°C (101.0°F) at home. His right leg is red and swollen from the dorsum of the foot to the thigh with an ill-defined edge. Venous stasis ulcers are present in both of his limbs, but those on the right have a yellow discharge. His vitals include the following: blood pressure is 120/78 mm Hg, heart rate is 94/min, temperature is 38.3°C (101.0°F), and respiratory rate is 16/min. On physical examination, there is tenderness and warmth compared with his normal leg. Dorsalis pedis pulses are present on both of the ankles. What is the most likely cause of the right shift of the hemoglobin dissociation curve for his condition?
- A. Decrease in temperature
- B. Increase in CO2 production
- C. Increase in pH
- D. Increase in temperature (Correct Answer)
- E. Decrease in 2,3-DPG
Altitude physiology Explanation: ***Increase in temperature***
- The patient presents with **fever (38.3°C)**, which is explicitly mentioned multiple times in the clinical scenario and represents a **systemic response** to infection.
- **Increased temperature** directly causes a **right shift** in the oxygen-hemoglobin dissociation curve by **decreasing hemoglobin's affinity for oxygen**.
- This facilitates oxygen release to metabolically active tissues, particularly important in areas of infection and inflammation.
- While multiple factors can cause right shifts during infection, the **fever is the most prominently featured clinical finding** in this case and represents a measurable systemic change.
*Decrease in temperature*
- A **decrease in temperature** causes a **left shift** in the oxygen-hemoglobin dissociation curve, **increasing hemoglobin's affinity for oxygen**.
- This would impair oxygen release to tissues, which is counterproductive during infection when tissues require increased oxygen delivery.
*Increase in CO2 production*
- While **increased CO2 production** does occur during infection due to increased tissue metabolism and does cause a **right shift** via the **Bohr effect** (CO2 + H2O → H2CO3 → H+ + HCO3-, leading to decreased pH), this is not the primary factor being highlighted in this clinical presentation.
- The Bohr effect (acidosis from increased CO2 and metabolic acids) is an important physiological response, but the question emphasizes the **fever** as the key feature of this patient's condition.
- In the context of this question asking about "his condition," the **temperature elevation is the most direct and measurable systemic change** presented.
*Increase in pH*
- An **increase in pH** (alkalosis) causes a **left shift** in the oxygen-hemoglobin dissociation curve, **increasing hemoglobin's oxygen affinity**.
- This would hinder oxygen delivery to tissues, which is not beneficial during infection when tissue oxygen demand is elevated.
*Decrease in 2,3-DPG*
- A **decrease in 2,3-bisphosphoglycerate (2,3-DPG)** causes a **left shift** in the oxygen-hemoglobin dissociation curve.
- This increases hemoglobin's affinity for oxygen, making oxygen release to tissues more difficult.
- During infection, 2,3-DPG levels typically remain stable or may increase slightly, not decrease.
Altitude physiology US Medical PG Question 10: A male infant is born at 27 weeks following premature rupture of membranes and a precipitous labor to a G4P3 female. Given the speed of delivery steroids are not given. Shortly after delivery he develops respiratory distress and the decision is made to administer surfactant replacement therapy. While the components of the surfactant used in surfactant therapy may vary based on institution, what is the main component of pulmonary surfactant produced by type II pneumocytes?
- A. Cholesterol
- B. Protein S
- C. Surfactant-associated proteins
- D. Phospholipids (Correct Answer)
- E. Zinc finger protein
Altitude physiology Explanation: ***Phospholipids***
- The main component of **pulmonary surfactant** produced by **type II pneumocytes** is **dipalmitoylphosphatidylcholine (DPPC)**, a type of **phospholipid**.
- These **phospholipids** reduce **alveolar surface tension**, preventing alveolar collapse at the end of expiration.
*Cholesterol*
- While **cholesterol** is present in biological membranes, it is a minor component of pulmonary surfactant and does not primarily determine its function.
- Its role is mainly in regulating the fluidity of the **surfactant film**, rather than reducing surface tension.
*Protein S*
- **Protein S** is a **vitamin K-dependent plasma protein** that functions as a **natural anticoagulant**; it is not a component of pulmonary surfactant.
- Its deficiency is associated with **thrombotic disorders**.
*Surfactant-associated proteins*
- **Surfactant-associated proteins (SPs)**, such as SP-A, SP-B, SP-C, and SP-D, are crucial for the **function and regulation** of pulmonary surfactant.
- However, they constitute a much smaller proportion by mass compared to **phospholipids**, which are the main structural and functional components.
*Zinc finger protein*
- **Zinc finger proteins** are a diverse class of proteins that bind to DNA, RNA, or other proteins and are involved in various cellular processes, including **gene regulation**.
- They are not a structural or functional component of **pulmonary surfactant**.
More Altitude physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.