Thermoregulation during exercise US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thermoregulation during exercise. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thermoregulation during exercise US Medical PG Question 1: A 35-year-old woman presents to the clinic for a several-month history of heat intolerance. She lives in a small apartment with her husband and reports that she always feels hot and sweaty, even when their air conditioning is on high. On further questioning, she's also had a 4.5 kg (10 lb) unintentional weight loss. The vital signs include: heart rate 102/min and blood pressure 150/80 mm Hg. The physical exam is notable for warm and slightly moist skin. She also exhibits a fine tremor in her hands when her arms are outstretched. Which of the following laboratory values is most likely low in this patient?
- A. Triiodothyronine (T3)
- B. Thyroxine (T4)
- C. Calcitonin
- D. Glucose
- E. Thyroid-stimulating hormone (Correct Answer)
Thermoregulation during exercise Explanation: ***Thyroid-stimulating hormone***
- The patient's symptoms (heat intolerance, weight loss, tachycardia, hypertension, warm/moist skin, fine tremor) are classic for **hyperthyroidism**.
- In primary hyperthyroidism, the thyroid gland overproduces T3 and T4, which **negatively feedbacks** on the pituitary, leading to a **low TSH** level.
*Triiodothyronine (T3)*
- In hyperthyroidism, **T3 levels are typically elevated**, not low, as the thyroid gland is overactive.
- T3 is one of the primary thyroid hormones responsible for the patient's metabolic symptoms.
*Thyroxine (T4)*
- In hyperthyroidism, **T4 levels are typically elevated**, not low, alongside T3.
- T4 is the other key thyroid hormone produced in excess, contributing to the hypermetabolic state.
*Calcitonin*
- Calcitonin is a hormone involved in **calcium regulation** and is produced by the parafollicular C cells of the thyroid gland.
- Its levels are not directly affected by hyperthyroidism and would not be consistently low in this scenario.
*Glucose*
- While hyperthyroidism can affect glucose metabolism, causing increased gluconeogenesis and glycogenolysis, it more commonly leads to **elevated or normal glucose levels**, not consistently low levels.
- Low glucose would typically suggest other conditions like insulinoma or adrenal insufficiency.
Thermoregulation during exercise US Medical PG Question 2: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Thermoregulation during exercise Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
Thermoregulation during exercise US Medical PG Question 3: A 25-year-old man presents to the emergency department after a motor vehicle accident. He was the unrestrained front seat driver in a head on collision. The patient is unresponsive and his medical history is unknown. His temperature is 99.5°F (37.5°C), blood pressure is 67/38 mmHg, pulse is 190/min, respirations are 33/min, and oxygen saturation is 98% on room air. The patient is started on IV fluids, blood products, and norepinephrine. A FAST exam is performed and a pelvic binder is placed. One hour later, his temperature is 98.3°F (36.8°C), blood pressure is 119/66 mmHg, pulse is 110/min, respirations are 15/min, and oxygen saturation is 97% on room air. The patient is currently responsive. Management of the patient's pelvic fracture is scheduled by the orthopedic service. While the patient is waiting in the emergency department he suddenly complains of feeling hot, aches, and a headache. The patient's temperature is currently 101°F (38.3°C). He has not been given any pain medications and his past medical history is still unknown. Which of the following is the most likely diagnosis?
- A. Acute hemolytic transfusion reaction
- B. Febrile non-hemolytic transfusion reaction (Correct Answer)
- C. Sympathetic response to pain
- D. Minor blood group incompatibility
- E. Leukoagglutination reaction
Thermoregulation during exercise Explanation: ***Febrile non-hemolytic transfusion reaction***
- This reaction is characterized by a **fever** and other constitutional symptoms (chills, headache, malaise) developing **within 4 hours of transfusion**, without evidence of hemolysis. The patient's symptoms and temperature rise after blood product administration fit this description.
- It is typically caused by antibodies in the recipient's plasma reacting with **leukocyte antigens** present on donor white blood cells or by **cytokines** released from donor leukocytes during storage.
*Acute hemolytic transfusion reaction*
- This reaction typically presents with more severe symptoms such as **hypotension**, **hemoglobinuria**, flank pain, and diffuse bleeding, indicating widespread intravascular hemolysis due to **ABO incompatibility**.
- Although the patient received blood products, his symptoms (feeling hot, aches, headache, mild fever) are not indicative of the severe, life-threatening nature of an acute hemolytic reaction.
*Sympathetic response to pain*
- While pain can cause a sympathetic response (tachycardia, hypertension), it typically does **not cause a fever** as seen in this patient.
- The patient's initial presentation included signs of shock, and after resuscitation, his vital signs normalized before the new symptoms appeared, suggesting a new process rather than ongoing pain alone.
*Minor blood group incompatibility*
- Reactions to minor blood group incompatibilities are usually **milder and delayed** compared to ABO incompatibilities.
- They often involve **extravascular hemolysis**, which might not present with the acute febrile reaction seen here, and are less common a cause of immediate febrile reactions.
*Leukoagglutination reaction*
- This is an older term for what is now often considered a type of **febrile non-hemolytic transfusion reaction (FNHTR)** caused by recipient antibodies to donor leukocyte antigens leading to leukocyte clumping.
- While related to FNHTR, the term "febrile non-hemolytic transfusion reaction" is the more encompassing and appropriate diagnosis given the typical symptom complex of fever, chills, and headache.
Thermoregulation during exercise US Medical PG Question 4: A 19-year-old woman is brought to the emergency department by ambulance 30 minutes after her neighbor found her unconscious on a running trail. Her neighbor reports that she has been training for a marathon since the beginning of the summer. She is alert and oriented but becomes irritable when realizing that she is at a hospital and refuses to answer questions. She appears tired. She is 174 cm (5 ft 7 in) tall and weighs 51 kg (112 lb). Her temperature is 35.5°C (96°F), pulse is 44/min, respirations are 20/min, and blood pressure is 84/48 mm Hg. Examination shows dry, scaly skin and dry mucous membranes. Cardiopulmonary examination shows a high-frequency, mid-to-late systolic murmur that is heard best at the apex. Her hemoglobin concentration is 11.9 g/dL. Which of the following is the most likely diagnosis?
- A. Heat exhaustion
- B. Hypertrophic obstructive cardiomyopathy
- C. Hypothyroidism
- D. Amphetamine use
- E. Anorexia nervosa (Correct Answer)
Thermoregulation during exercise Explanation: ***Anorexia nervosa***
- The patient's **low BMI** (16.9 kg/m^2), **bradycardia**, **hypotension**, **hypothermia**, and **dry, scaly skin** are classic signs of anorexia nervosa, exacerbated by intense exercise (marathon training).
- The **mid-to-late systolic murmur** heard best at the apex is likely due to **mitral valve prolapse**, a common cardiac finding in patients with severe anorexia nervosa due to decreased ventricular size and structural changes.
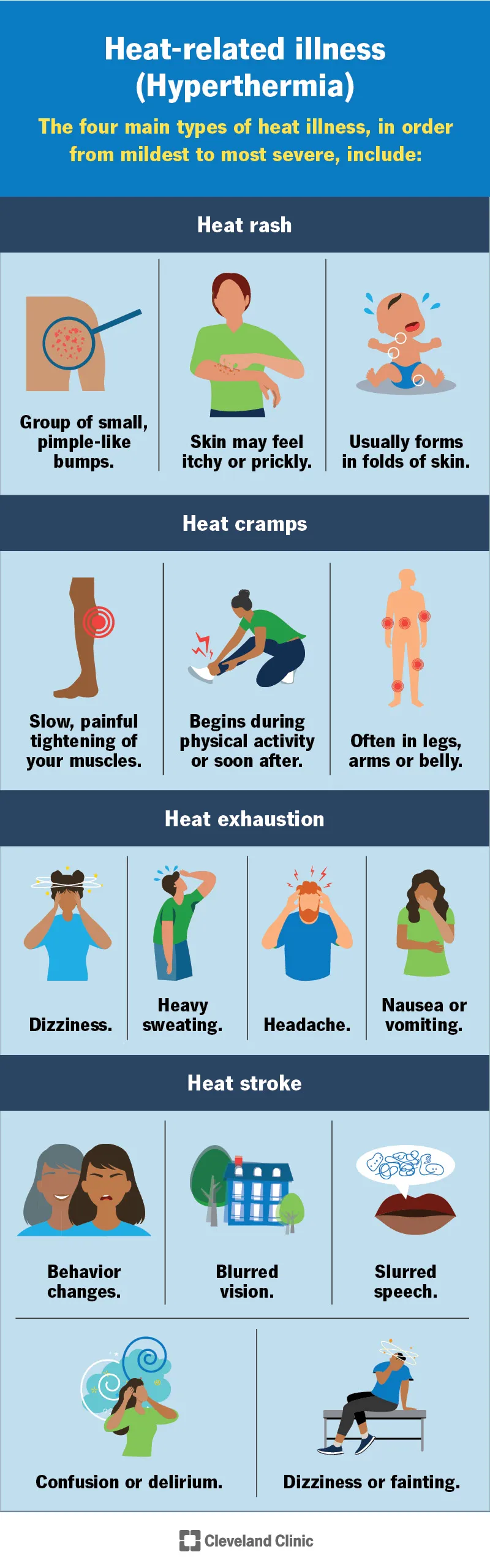
*Heat exhaustion*
- Although the patient was exercising, her **temperature is low (96°F)**, which contradicts the expected elevated temperature in heat exhaustion.
- Heat exhaustion typically presents with profuse sweating, not **dry mucous membranes** or **dry, scaly skin**.
*Hypertrophic obstructive cardiomyopathy*
- While it can cause a **systolic murmur** and exercise-induced syncope, it usually presents with a **loud S4**, and the patient's other symptoms like **hypothermia**, **bradycardia**, and severe **cachexia** are not typical.
- It would not explain the **low body weight**, **dry skin**, or **hypotension** as primary symptoms.
*Hypothyroidism*
- Hypothyroidism can cause **fatigue**, **bradycardia**, **hypothermia**, and **dry skin**, but it does not typically lead to such extreme **weight loss** or **hypotension** in a young, active individual.
- It doesn't explain the specific cardiac murmur described or the history of intense marathon training contributing to the presentation.
*Amphetamine use*
- Amphetamine use typically causes **tachycardia**, **hypertension**, **dilation of pupils**, and **hyperthermia**, which are opposite to this patient's presentation of bradycardia, hypotension, and hypothermia.
- The patient's **cachectic appearance** could be associated with stimulant use, but the vital signs and overall clinical picture strongly contradict it.
Thermoregulation during exercise US Medical PG Question 5: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Thermoregulation during exercise Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Thermoregulation during exercise US Medical PG Question 6: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Thermoregulation during exercise Explanation: ***Anterior hypothalamus***
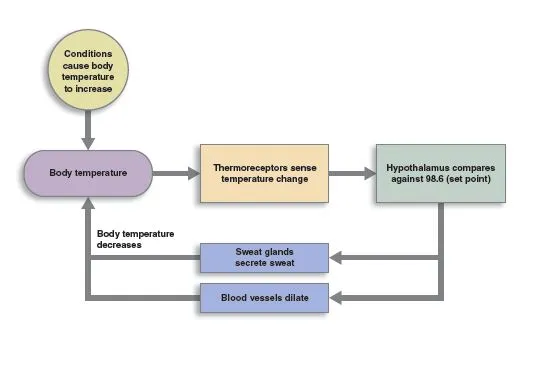
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Thermoregulation during exercise US Medical PG Question 7: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Thermoregulation during exercise Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
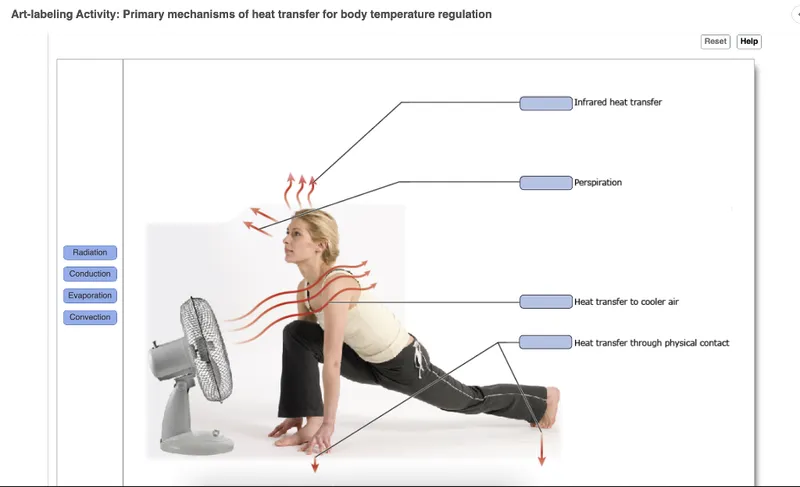
Thermoregulation during exercise US Medical PG Question 8: A group of investigators is studying thermoregulatory adaptations of the human body. A subject is seated in a thermally insulated isolation chamber with an internal temperature of 48°C (118°F), a pressure of 1 atmosphere, and a relative humidity of 10%. Which of the following is the primary mechanism of heat loss in this subject?
- A. Convection
- B. Evaporation (Correct Answer)
- C. Conduction
- D. Piloerection
- E. Radiation
Thermoregulation during exercise Explanation: ***Evaporation***
- In an environment where the ambient temperature (48°C) is **higher than body temperature**, heat gain by convection, conduction, and radiation occurs. Therefore, **evaporation** of sweat is the only significant mechanism for heat loss.
- The relatively low humidity (10%) at this high temperature facilitates efficient sweat **evaporation**, which cools the body as it converts liquid sweat into water vapor.
*Convection*
- **Convection** involves heat transfer through the movement of air or fluid over the body surface.
- Since the ambient temperature (48°C) is significantly **above body temperature**, the body would gain heat via convection, not lose it.
*Conduction*
- **Conduction** is direct heat transfer between objects in contact.
- As the ambient temperature (48°C) is much **higher than the skin temperature**, the body would actually **gain heat** through conduction from any surfaces it touched if they were at ambient temperature.
*Piloerection*
- **Piloerection** (goosebumps) is a mechanism for minimizing heat loss by trapping a layer of warm air close to the skin.
- This response is activated in **cold environments** to conserve heat, not in hot environments to dissipate it.
*Radiation*
- **Radiation** is heat transfer via electromagnetic waves without direct contact.
- Since the ambient temperature (48°C) is **higher than body surface temperature**, the body would **gain heat** by radiation, not lose it efficiently, from the surrounding environment.
Thermoregulation during exercise US Medical PG Question 9: A 34-year-old woman comes to a physician for a routine health maintenance examination. She moved to Denver 1 week ago after having lived in New York City all her life. She has no history of serious illness and takes no medications. Which of the following sets of changes is most likely on analysis of a blood sample obtained now compared to prior to her move?
Erythropoietin level | O2 saturation | Plasma volume
- A. ↑ unchanged unchanged
- B. ↑ ↓ ↓ (Correct Answer)
- C. Unchanged ↓ unchanged
- D. ↓ unchanged ↑
- E. Unchanged unchanged ↓
Thermoregulation during exercise Explanation: ***↑ ↓ ↓***
- Moving to a high altitude like Denver (from sea level NYC) leads to **hypoxia**, which triggers increased **erythropoietin (EPO)** production to stimulate red blood cell formation.
- The immediate physiological response to high altitude is a **decrease in arterial PO2** and thus **oxygen saturation**, along with a **reduction in plasma volume** due to increased diuresis and fluid shifts.
*↑ unchanged unchanged*
- While **erythropoietin** would increase due to hypoxia at higher altitudes, **oxygen saturation** would decrease, not remain unchanged.
- **Plasma volume** also tends to decrease acutely at high altitudes, rather than staying unchanged.
*Unchanged ↓ unchanged*
- **Erythropoietin** would be expected to increase, not remain unchanged, as a compensatory mechanism to hypoxia.
- While **oxygen saturation** would decrease, **plasma volume** typically decreases acutely, not remaining unchanged.
*↓ unchanged ↑*
- **Erythropoietin** would increase, not decrease, in response to the lower atmospheric oxygen.
- Both **oxygen saturation** and **plasma volume** would decrease, not remain unchanged or increase, respectively.
*Unchanged unchanged ↓*
- **Erythropoietin** would increase, not remain unchanged, to stimulate red blood cell production in response to hypoxia.
- **Oxygen saturation** would decrease, not remain unchanged, at higher altitudes.
Thermoregulation during exercise US Medical PG Question 10: A 28-year-old woman presents to her primary care physician with recurring muscle cramps that have lasted for the last 2 weeks. She mentions that she commonly has these in her legs and back. She also has a constant tingling sensation around her mouth. On physical examination, her vital signs are stable. The Trousseau sign and Chvostek sign are present with exaggerated deep tendon reflexes. A comprehensive blood test reveals the following:
Na+ 140 mEq/L
K+ 4.5 mEq/L
Chloride 100 mEq/L
Bicarbonate 24 mEq/L
Creatinine 0.9 mg/dL
Ca2+ 7.0 mg/dL
Which of the following electrophysiologic mechanisms best explain this woman’s clinical features?
- A. Decreased firing threshold for action potential (Correct Answer)
- B. Reduction of afterhyperpolarization
- C. Inhibition of sodium current through sodium leak channels (NALCN)
- D. Inhibition of Na+ and Ca2+ currents through cyclic nucleotide-gated (CNG) channels
- E. Stimulation of GABA (γ-aminobutyric acid) receptors
Thermoregulation during exercise Explanation: ***Decreased firing threshold for action potential***
- The patient exhibits symptoms of **hypocalcemia** (muscle cramps, perioral tingling, positive Trousseau and Chvostek signs), indicated by her **low serum Ca2+ (7.0 mg/dL)**.
- **Hypocalcemia** leads to increased neuronal excitability by **decreasing the threshold for action potential firing**.
- **Mechanism**: Extracellular calcium ions normally bind to negatively charged groups on voltage-gated sodium channels, stabilizing them in the closed state and increasing the threshold for opening.
- With **low calcium**, this stabilization is reduced, allowing sodium channels to open more easily at less negative membrane potentials, effectively **lowering the firing threshold**.
- This results in spontaneous depolarizations and the neuromuscular hyperexcitability seen clinically as tetany, muscle cramps, and hyperreflexia.
*Stimulation of GABA (γ-aminobutyric acid) receptors*
- **GABA receptor stimulation** leads to **inhibition of neuronal activity** by increasing chloride influx, hyperpolarizing the cell, and reducing excitability.
- This would **decrease muscle cramps and excitability**, opposite to the patient's symptoms.
*Reduction of afterhyperpolarization*
- While hypocalcemia does affect membrane excitability, the **primary mechanism** is the decreased threshold for sodium channel activation, not afterhyperpolarization changes.
- Reduction of afterhyperpolarization would affect repetitive firing patterns but does not explain the initial hyperexcitability at the sodium channel level.
*Inhibition of sodium current through sodium leak channels (NALCN)*
- **NALCN channels** contribute to resting membrane potential; their inhibition would lead to **hyperpolarization** and reduced excitability.
- This is opposite to the **hypocalcemic hyperexcitability** observed in this patient.
*Inhibition of Na+ and Ca2+ currents through cyclic nucleotide-gated (CNG) channels*
- **CNG channels** are primarily involved in sensory signal transduction (vision, olfaction).
- Their inhibition would cause specific sensory deficits, not the generalized neuromuscular hyperexcitability seen in **hypocalcemia**.
More Thermoregulation during exercise US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.