Respiratory adaptations during exercise US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory adaptations during exercise. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory adaptations during exercise US Medical PG Question 1: A 25-year-old male athlete undergoes a cardiopulmonary exercise test. As exercise intensity increases from rest to moderate levels, which of the following best describes the relationship between oxygen consumption and cardiac output?
- A. Linear increase until anaerobic threshold (Correct Answer)
- B. Exponential increase throughout exercise
- C. Plateau at low exercise intensities
- D. No change until anaerobic threshold
Respiratory adaptations during exercise Explanation: ***Linear increase until anaerobic threshold***
- During incremental exercise, both **oxygen consumption (VO2)** and **cardiac output (CO)** increase proportionally with work rate.
- This **linear relationship** continues until the body reaches the **anaerobic threshold**, beyond which other physiological responses begin to dominate.
*Exponential increase throughout exercise*
- An **exponential increase** would imply a disproportionately rapid rise in oxygen consumption and cardiac output even at low-to-moderate exercise intensities, which is not physiologically accurate.
- While both parameters do increase, the initial increase is typically linear, reflecting the immediate physiological demands.
*Plateau at low exercise intensities*
- A **plateau** would suggest that the body's demand for oxygen and the heart's pumping capacity stabilize despite an increase in exercise intensity, which contradicts the need for increased energy supply during exercise.
- The cardiovascular system actively responds to even low-intensity exercise to meet metabolic demands.
*No change until anaerobic threshold*
- **No change** would mean that the cardiovascular system is not responding to the increased metabolic demands of exercise, which is incorrect.
- Both VO2 and CO begin to rise almost immediately upon starting exercise to meet the muscles' increasing oxygen requirements.
Respiratory adaptations during exercise US Medical PG Question 2: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Respiratory adaptations during exercise Explanation: ***Correct: Treadmill exercise***
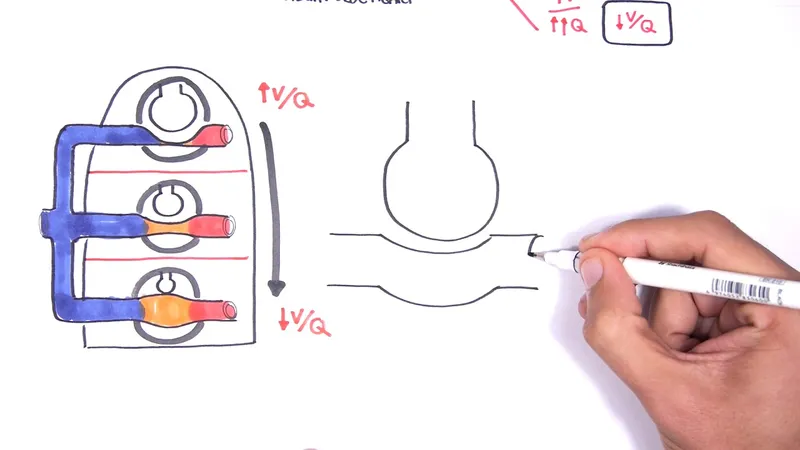
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Respiratory adaptations during exercise US Medical PG Question 3: A 24-year-old woman presents to the emergency department after she was found agitated and screaming for help in the middle of the street. She says she also has dizziness and tingling in the lips and hands. Her past medical history is relevant for general anxiety disorder, managed medically with paroxetine. At admission, her pulse is 125/min, respiratory rate is 25/min, and body temperature is 36.5°C (97.7°F). Physical examination is unremarkable. An arterial blood gas sample is taken. Which of the following results would you most likely expect to see in this patient?
- A. pH: increased, HCO3-: increased, Pco2: increased
- B. pH: decreased, HCO3-: decreased, Pco2: decreased
- C. pH: decreased, HCO3-: increased, Pco2: increased
- D. pH: increased, HCO3-: decreased, Pco2: decreased (Correct Answer)
- E. pH: normal, HCO3-: increased, Pco2: increased
Respiratory adaptations during exercise Explanation: ***pH: increased, HCO3-: decreased, Pco2: decreased***
- The patient's presentation with **agitation**, **dizziness**, **paresthesias** (tingling in lips and hands), and **tachypnea** (respiratory rate 25/min) is highly suggestive of **hyperventilation** due to an anxiety attack.
- **Hyperventilation** leads to excessive **CO2 expulsion**, causing a decrease in Pco2, which results in respiratory alkalosis (increased pH) and a compensatory decrease in HCO3-.
*pH: increased, HCO3-: increased, Pco2: increased*
- An **increased pH** coupled with **increased HCO3-** and **increased Pco2** would suggest a **metabolic alkalosis with respiratory compensation**, which is not consistent with the patient's acute hyperventilation.
- While pH is increased, the other values contradict the primary respiratory cause suggested by the symptoms.
*pH: decreased, HCO3-: decreased, Pco2: decreased*
- This profile describes **metabolic acidosis with respiratory compensation**, which would typically present with **Kussmaul breathing** and other signs of acidosis, not acute hyperventilation and agitation.
- Symptoms such as dizziness and tingling are associated with alkalosis, not acidosis.
*pH: decreased, HCO3-: increased, Pco2: increased*
- This pattern is characteristic of **respiratory acidosis with metabolic compensation**, often seen in conditions like **COPD exacerbation** or **opioid overdose** with hypoventilation.
- The patient's rapid breathing and clinical picture are not consistent with respiratory acidosis.
*pH: normal, HCO3-: increased, Pco2: increased*
- A **normal pH** with **increased HCO3-** and **increased Pco2** would indicate a **compensated metabolic alkalosis**.
- Her acute symptoms point to an uncompensated or acutely compensated respiratory disorder, not a compensated metabolic issue.
Respiratory adaptations during exercise US Medical PG Question 4: Which mechanism is primarily responsible for the increase in pulmonary diffusing capacity during exercise?
- A. Decreased airway resistance
- B. Reduced membrane thickness
- C. Increased alveolar ventilation
- D. Pulmonary capillary recruitment (Correct Answer)
Respiratory adaptations during exercise Explanation: ***Pulmonary capillary recruitment***
- During exercise, more **pulmonary capillaries** that were previously unperfused or poorly perfused open up, increasing the **surface area available for gas exchange**.
- This **recruitment** directly enhances the pulmonary diffusing capacity by providing more sites for oxygen to cross from the alveoli into the blood.
*Decreased airway resistance*
- While airway resistance can decrease during exercise due to **bronchodilation**, this primarily affects **airflow** and ventilation, not the efficiency of gas diffusion across the alveolar-capillary membrane.
- Reduced airway resistance facilitates getting air into and out of the lungs but does not expand the surface area for diffusion or thin the membrane.
*Reduced membrane thickness*
- The thickness of the **alveolar-capillary membrane** is a structural characteristic that does not significantly change acutely during exercise.
- While a thinner membrane would improve diffusion, this is not the primary mechanism behind the exercise-induced increase in diffusing capacity.
*Increased alveolar ventilation*
- Increased alveolar ventilation ensures a higher **partial pressure of oxygen** in the alveoli.
- While essential for delivering oxygen, it primarily affects the **driving pressure for diffusion** rather than the physical capacity of the diffusion barrier itself.
Respiratory adaptations during exercise US Medical PG Question 5: A 21-year-old man is admitted to the intensive care unit for respiratory failure requiring mechanical ventilation. His minute ventilation is calculated to be 7.0 L/min, and his alveolar ventilation is calculated to be 5.1 L/min. Which of the following is most likely to decrease the difference between minute ventilation and alveolar ventilation?
- A. Increasing the partial pressure of inhaled oxygen
- B. Decreasing the affinity of hemoglobin for oxygen
- C. Increasing the respiratory depth
- D. Decreasing the physiologic dead space (Correct Answer)
- E. Increasing the respiratory rate
Respiratory adaptations during exercise Explanation: ***Decreasing the physiologic dead space***
- The difference between **minute ventilation (VE)** and **alveolar ventilation (VA)** is the **dead space ventilation (VD)**, calculated as: VE - VA = VD
- In this case: 7.0 L/min - 5.1 L/min = 1.9 L/min of dead space ventilation
- Decreasing the **physiologic dead space** directly reduces this difference by allowing a greater proportion of each breath to participate in gas exchange
- This is the most direct way to narrow the gap between VE and VA
*Increasing the partial pressure of inhaled oxygen*
- This intervention primarily affects **oxygenation** by increasing the driving pressure for oxygen diffusion into the blood
- It does not directly change the volume of air participating in alveolar ventilation or reduce dead space ventilation
- The distribution of ventilation between alveolar and dead space remains unchanged
*Decreasing the affinity of hemoglobin for oxygen*
- A decrease in hemoglobin affinity for oxygen facilitates **oxygen unloading** to the tissues (rightward shift of the oxygen-hemoglobin dissociation curve)
- This effect is related to **oxygen delivery** and does not alter the proportion of minute ventilation that reaches the alveoli for gas exchange
- Dead space ventilation remains unchanged
*Increasing the respiratory depth*
- Increasing respiratory depth increases **tidal volume (VT)**, which improves the **ratio** of alveolar ventilation to minute ventilation (VA/VE efficiency)
- However, the **absolute difference** (VE - VA) in L/min depends on the **total dead space volume**, which is not changed by increasing tidal volume alone
- While this improves ventilation efficiency, it does not directly reduce the dead space ventilation measured in L/min unless physiologic dead space itself decreases
*Increasing the respiratory rate*
- While increasing respiratory rate increases **minute ventilation (VE)**, it also increases the frequency of ventilating the **dead space** with each breath
- Since dead space ventilation (VD) = respiratory rate × dead space volume, increasing rate while keeping tidal volume constant will proportionally increase both VE and VD
- This can actually widen the absolute gap between VE and VA, making it less efficient
Respiratory adaptations during exercise US Medical PG Question 6: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Respiratory adaptations during exercise Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Respiratory adaptations during exercise US Medical PG Question 7: A 21-year-old lacrosse player comes to the doctor for an annual health assessment. She does not smoke or drink alcohol. She is 160 cm (5 ft 3 in) tall and weighs 57 kg (125 lb); BMI is 22 kg/m2. Pulmonary function tests show an FEV1 of 90% and an FVC of 3600 mL. Whole body plethysmography is performed to measure airway resistance. Which of the following structures of the respiratory tree is likely to have the highest contribution to total airway resistance?
- A. Conducting bronchioles
- B. Terminal bronchioles
- C. Segmental bronchi (Correct Answer)
- D. Respiratory bronchioles
- E. Mainstem bronchi
Respiratory adaptations during exercise Explanation: ***Segmental bronchi***
- In healthy individuals, **medium-sized bronchi** (including segmental and subsegmental bronchi, approximately generations 4-8) contribute approximately **80% of total airway resistance**.
- While **Poiseuille's Law** states resistance is inversely proportional to radius to the fourth power (R ∝ 1/r⁴), the key factor is the **total cross-sectional area** and **degree of branching**.
- Medium-sized bronchi have moderate individual resistance and **limited parallel branching**, making them the dominant site of resistance.
- This is why diseases affecting medium-sized airways (e.g., asthma, bronchitis) cause significant increases in airway resistance.
*Terminal bronchioles*
- Although individual terminal bronchioles have small radii and high individual resistance, there are **millions of them arranged in parallel**.
- With parallel resistances, total resistance decreases: 1/R_total = 1/R₁ + 1/R₂ + 1/R₃...
- The **massive number** of small airways means their collective resistance is actually quite **low** (~10-20% of total).
- This is why small airways disease is called the "**silent zone**" - significant pathology can occur before detection.
*Conducting bronchioles*
- These airways also benefit from extensive **parallel branching**, reducing their contribution to total resistance.
- They contribute less than medium-sized bronchi due to their large cumulative cross-sectional area.
*Respiratory bronchioles*
- Part of the **respiratory zone** with the largest total cross-sectional area in the lungs.
- Minimal contribution to airway resistance due to enormous parallel arrangement.
- Primary function is **gas exchange**, not air conduction.
*Mainstem bronchi*
- These large airways have **low individual resistance** due to large diameter.
- Together with the trachea, they contribute approximately **20% of total airway resistance**.
- Not the primary site despite being early in the airway tree.
Respiratory adaptations during exercise US Medical PG Question 8: A 22-year-old man volunteers for a research study on lung function. He has no history of lung disease or allergies and does not smoke. His pulmonary blood flow is measured in the various labeled segments of the lungs while standing. Then the volunteer, still standing, is given very low continuous positive airway pressure and the blood flow measured again. Which of the following sets of findings are most likely to be present in the second measurements relative to the first?
- A. Increased blood flow in zone 2
- B. Reduced blood flow in zone 3
- C. Reduced blood flow in zone 1
- D. Increased blood flow in zone 3
- E. Increased blood flow in zone 1 (Correct Answer)
Respiratory adaptations during exercise Explanation: ***Increased blood flow in zone 1***
- In healthy standing subjects, **Zone 1** may not exist or is minimal at the apex where alveolar pressure (PA) can exceed arterial pressure (Pa).
- **Very low CPAP** increases alveolar pressure, but when applied at very low levels, it may **recruit collapsed or under-perfused alveoli** by preventing alveolar collapse and improving the pressure gradient.
- The net effect with **very low CPAP** can paradoxically **improve perfusion** in Zone 1 by optimizing alveolar mechanics and reducing vascular resistance through **alveolar recruitment**, particularly in previously under-ventilated apical regions.
*Increased blood flow in zone 2*
- In Zone 2, arterial pressure exceeds alveolar pressure, which exceeds venous pressure (**Pa > PA > Pv**), creating a waterfall effect.
- While CPAP increases alveolar pressure (PA), this would increase the downstream resistance and typically **reduce** the arterial-alveolar pressure gradient (Pa - PA), decreasing flow rather than increasing it.
*Increased blood flow in zone 3*
- **Zone 3** (lung base) normally has the **highest blood flow** where both arterial and venous pressures exceed alveolar pressure (**Pa > Pv > PA**).
- CPAP increases alveolar pressure (PA), which would compress capillaries and **reduce** the pressure gradient, typically decreasing rather than increasing blood flow in this zone.
*Reduced blood flow in zone 1*
- While increasing alveolar pressure with CPAP might be expected to **reduce** Zone 1 perfusion by compressing capillaries, **very low levels of CPAP** can have the opposite effect through **alveolar recruitment** and optimization of lung mechanics.
- The question specifies **very low** CPAP, which is the key—this level improves alveolar patency without significantly compressing capillaries.
*Reduced blood flow in zone 3*
- Zone 3 typically has the highest blood flow due to favorable pressure gradients from gravity.
- CPAP increases PA, which could compress capillaries and reduce the (Pa - PA) gradient, but the **very low level** specified means this effect is minimal and Zone 3 generally maintains adequate perfusion.
Respiratory adaptations during exercise US Medical PG Question 9: A 19-year-old male soccer player undergoes an exercise tolerance test to measure his maximal oxygen uptake during exercise. Which of the following changes are most likely to occur during exercise?
- A. Increased apical ventilation-perfusion ratio
- B. Decreased physiologic dead space (Correct Answer)
- C. Decreased alveolar-arterial oxygen gradient
- D. Increased arterial partial pressure of oxygen
- E. Increased pulmonary vascular resistance
Respiratory adaptations during exercise Explanation: **Decreased physiologic dead space**
- During exercise, there is improved perfusion to previously underperfused areas of the lung, leading to a **more uniform ventilation-perfusion (V/Q) matching** and thus a decrease in physiologic dead space.
- The increased cardiac output helps to perfuse more capillaries, reducing the amount of ventilated air that does not participate in gas exchange.
*Increased apical ventilation-perfusion ratio*
- At rest, the **apical V/Q ratio is already high** due to gravity-dependent differences in blood flow; exercise partially normalizes these differences.
- While overall V/Q matching improves, the relative V/Q differences between apical and basal regions may become less pronounced, not necessarily a further increase in the apical ratio.
*Decreased alveolar-arterial oxygen gradient*
- During severe exercise, the **A-a gradient often increases slightly** due to increased oxygen diffusion limitations and V/Q mismatch.
- Although overall gas exchange efficiency improves, the sheer volume of oxygen demand can reveal small imbalances, rather than fully eliminating the gradient.
*Increased arterial partial pressure of oxygen*
- Exercise typically leads to **stable or slightly decreased arterial PO2** in healthy individuals due to the increased metabolic demand and potential small V/Q mismatches.
- The body maintains arterial PO2 remarkably well even at high exertion, but it does not usually significantly increase.
*Increased pulmonary vascular resistance*
- During exercise, **pulmonary vascular resistance (PVR) generally decreases** due to recruitment and distension of pulmonary capillaries.
- This decrease in PVR helps to accommodate the increased cardiac output without a significant rise in pulmonary arterial pressure.
Respiratory adaptations during exercise US Medical PG Question 10: A 64-year-old man presents to his primary care physician for follow-up of a severe, unrelenting, productive cough of 2 years duration. The medical history includes type 2 diabetes mellitus, which is well-controlled with insulin. He has a 25-pack-year smoking history and is an active smoker. The blood pressure is 135/88 mm Hg, the pulse is 94/min, the temperature is 36.9°C (98.5°F), and the respiratory rate is 18/min. Bilateral wheezes and crackles are heard on auscultation. A chest X-ray reveals cardiomegaly, increased lung markings, and a flattened diaphragm. Which of the following is most likely in this patient?
- A. Increased pH of the arterial blood
- B. Increased cerebral vascular resistance
- C. Increased pulmonary arterial resistance (Correct Answer)
- D. Decreased carbon dioxide content of the arterial blood
- E. Increased right ventricle compliance
Respiratory adaptations during exercise Explanation: ***Increased pulmonary arterial resistance***
- This patient's long-standing **smoking history**, chronic productive cough, **wheezes**, and **crackles** suggest **Chronic Obstructive Pulmonary Disease (COPD)**, likely including chronic bronchitis and emphysema.
- **COPD** often leads to **hypoxia**, causing **pulmonary vasoconstriction** and subsequent increase in **pulmonary arterial resistance**, eventually leading to **pulmonary hypertension** and **cor pulmonale** (right-sided heart failure).
*Increased pH of the arterial blood*
- Patients with severe COPD and chronic respiratory insufficiency often develop **chronic hypercapnia** (increased **PaCO2**), leading to **respiratory acidosis** and a tendency towards a **decreased pH** or a normal pH with compensation.
- An **increased pH** (alkalosis) would be less likely in the context of chronic ventilatory compromise.
*Increased cerebral vascular resistance*
- In chronic hypercapnia and hypoxia, **cerebral blood vessels** typically **dilate** to maintain cerebral perfusion, leading to **decreased cerebral vascular resistance**, not increased.
- This vasodilation can contribute to symptoms like headaches and altered mental status in severe cases.
*Decreased carbon dioxide content of the arterial blood*
- Patients with chronic obstructive lung disease often have impaired gas exchange, leading to **CO2 retention** (**hypercapnia**).
- Therefore, the **arterial carbon dioxide content** would typically be **increased**, not decreased.
*Increased right ventricle compliance*
- In the setting of chronic **pulmonary hypertension**, the right ventricle is subjected to increased pressure overload, leading to **ventricular hypertrophy** and eventually **decreased compliance** and **ventricular dysfunction**.
- **Increased compliance** (meaning the ventricle stretches more easily) is contrary to the expected response in chronic pressure overload.
More Respiratory adaptations during exercise US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.