Muscle fiber types and recruitment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Muscle fiber types and recruitment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Muscle fiber types and recruitment US Medical PG Question 1: A 24-year-old professional athlete is advised to train in the mountains to enhance his performance. After 5 months of training at an altitude of 1.5 km (5,000 feet), he is able to increase his running pace while competing at sea-level venues. Which of the following changes would produce the same effect on the oxygen-hemoglobin dissociation curve as this athlete's training did?
- A. Decreased 2,3-bisphosphoglycerate (Correct Answer)
- B. Increased carbon monoxide inhalation
- C. Decreased temperature
- D. Decreased pH
- E. Increased partial pressure of oxygen
Muscle fiber types and recruitment Explanation: ***Decreased 2,3-bisphosphoglycerate***
- This is **NOT** the correct physiological adaptation from altitude training, making this question conceptually flawed.
- Altitude training causes **increased erythropoietin → polycythemia → increased total hemoglobin**, which increases oxygen-carrying capacity.
- 2,3-BPG is **initially increased** at altitude (right shift) to facilitate O2 release, and remains elevated or returns to normal with acclimatization, **not decreased**.
- While decreased 2,3-BPG would cause a left shift (increased O2 affinity), this does NOT replicate altitude training adaptations.
*Increased carbon monoxide inhalation*
- Carbon monoxide binds hemoglobin with **200-250× higher affinity** than oxygen, forming carboxyhemoglobin.
- This **reduces oxygen-carrying capacity** and causes a left shift for remaining hemoglobin.
- This is harmful and does NOT replicate beneficial altitude adaptations.
*Decreased temperature*
- Decreases metabolic rate and causes a **left shift** (increased O2 affinity).
- Oxygen is held more tightly and released less readily to tissues.
- This does NOT replicate altitude training benefits.
*Decreased pH*
- Acidosis causes the **Bohr effect**: **right shift** (decreased O2 affinity).
- Facilitates O2 release to tissues during exercise.
- This is beneficial during exercise but does NOT replicate the chronic altitude adaptation of increased oxygen-carrying capacity.
*Increased partial pressure of oxygen*
- Higher PO2 increases hemoglobin saturation but does NOT shift the curve.
- This increases oxygen availability but does NOT replicate the physiological adaptation (polycythemia) from altitude training.
**Note:** This question is conceptually problematic as none of the options accurately replicate the primary altitude training adaptation (increased RBC mass/hemoglobin concentration).
Muscle fiber types and recruitment US Medical PG Question 2: A 15-year-old boy is sent from gym class with a chief complaint of severe muscle aches. In class today he was competing with his friends and therefore engaged in weightlifting for the first time. A few hours later he was extremely sore and found that his urine was red when he went to urinate. This concerned him and he was sent to the emergency department for evaluation.
Upon further questioning, you learn that since childhood he has always had muscle cramps with exercise. Physical exam was unremarkable. Upon testing, his creatine kinase level was elevated and his urinalysis was negative for blood and positive for myoglobin.
Thinking back to biochemistry you suspect that he may be suffering from a hereditary glycogen disorder. Given this suspicion, what would you expect to find upon examination of his cells?
- A. Normal glycogen structure (Correct Answer)
- B. Short outer glycogen chains
- C. Accumulation of glycogen in lysosomes forming dense granules
- D. Glycogen without normal branching pattern
- E. Absence of glycogen in muscles
Muscle fiber types and recruitment Explanation: ***Normal glycogen structure***
- The patient's symptoms (exercise-induced muscle cramps, myoglobinuria, and elevated CK) are classic for **McArdle disease** (Glycogen Storage Disease Type V), caused by a deficiency in **muscle glycogen phosphorylase**.
- In McArdle disease, the enzyme responsible for breaking down glycogen (glycogen phosphorylase) is deficient, but the enzymes involved in synthesizing glycogen are normal. Therefore, the **structure of glycogen is normal**, but it accumulates in muscle cells because it cannot be catabolized.
*Short outer glycogen chains*
- **Short outer glycogen chains** are characteristic of **Cori disease** (Glycogen Storage Disease Type III), caused by a deficiency in **debranching enzyme**.
- This condition also presents with hypoglycemia and hepatomegaly, which are not described in the patient's presentation.
*Accumulation of glycogen in lysosomes forming dense granules*
- **Accumulation of glycogen in lysosomes** and the formation of **dense granules** is characteristic of **Pompe disease** (Glycogen Storage Disease Type II), caused by a deficiency in **lysosomal alpha-glucosidase (acid maltase)**.
- Pompe disease typically presents as a severe infantile form with cardiomegaly and hypotonia, or a later-onset form with proximal muscle weakness, which differs from the patient's primary complaint of exercise intolerance and myoglobinuria.
*Glycogen without normal branching pattern*
- **Glycogen without a normal branching pattern** (very long unbranched chains) is characteristic of **Andersen disease** (Glycogen Storage Disease Type IV), caused by a deficiency in **branching enzyme**.
- This condition typically leads to cirrhosis and liver failure in infancy, which is not consistent with the patient's presentation.
*Absence of glycogen in muscles*
- While McArdle disease involves an inability to break down muscle glycogen, it does not result in the **absence of glycogen** in muscles; rather, there is an **over-accumulation** of normal-structured glycogen because it cannot be utilized.
- The defect is in **glycogenolysis**, not glycogen synthesis, so glycogen is formed but not broken down.
Muscle fiber types and recruitment US Medical PG Question 3: A healthy 22-year-old male participates in a research study you are leading to compare the properties of skeletal and cardiac muscle. You conduct a 3-phased experiment with the participant. In the first phase, you get him to lift up a 2.3 kg (5 lb) weight off a table with his left hand. In the second phase, you get him to do 20 burpees, taking his heart rate to 150/min. In the third phase, you electrically stimulate his gastrocnemius with a frequency of 50 Hz. You are interested in the tension and electrical activity of specific muscles as follows: Biceps in phase 1, cardiac muscle in phase 2, and gastrocnemius in phase 3. What would you expect to be happening in the phases and the respective muscles of interest?
- A. Increase of tension in experiments 2 and 3, with the same underlying mechanism
- B. Increase of tension in all phases (Correct Answer)
- C. Recruitment of large motor units followed by small motor units in experiment 1
- D. Fused tetanic contraction at the end of all three experiments
- E. Recruitment of small motor units at the start of experiments 1 and 2
Muscle fiber types and recruitment Explanation: ***Increase of tension in all phases***
- In **phase 1**, lifting a 2.3 kg weight requires the **biceps** to contract, generating sufficient force (**tension**) to overcome gravity.
- In **phase 2**, the **cardiac muscle** increases its contractile force (**tension**) to meet the metabolic demands of **exercise**, leading to a heart rate of 150/min.
- In **phase 3**, electrical stimulation of the **gastrocnemius** at 50 Hz triggers muscle contraction, leading to an increase in **tension**.
*Increase of tension in experiments 2 and 3, with the same underlying mechanism*
- While tension increases in phases 2 and 3, the **underlying mechanisms differ**: cardiac muscle tension increases due to increased sympathetic stimulation and preload, while skeletal muscle tension increases due to unfused or fused tetanus from electrical stimulation.
- Cardiac muscle contraction is regulated by **calcium-induced calcium release**, while skeletal muscle involves direct coupling of DHP receptor and ryanodine receptor.
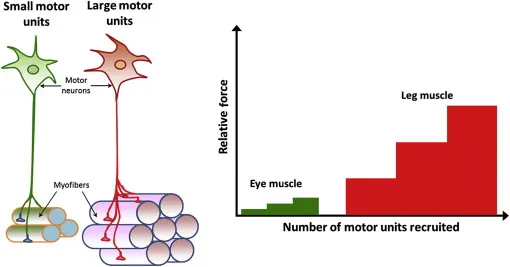
*Recruitment of large motor units followed by small motor units in experiment 1*
- **Motor unit recruitment** follows the **size principle**, meaning smaller, more easily excitable motor units are activated first, followed by larger ones as more force is needed.
- Therefore, in phase 1, **small motor units** would be recruited first, not large ones.
*Fused tetanic contraction at the end of all three experiments*
- **Fused tetanic contraction** occurs in **skeletal muscle** when stimulation frequency is high enough that individual twitches summate completely, leading to sustained contraction.
- This phenomenon is **not possible in cardiac muscle** due to its long **refractory period**, which prevents sustained contraction and allows for adequate filling time.
*Recruitment of small motor units at the start of experiments 1 and 2*
- **Motor unit recruitment** applies to **skeletal muscle** (phase 1) and involves recruiting small motor units first for fine or gentle movements.
- **Cardiac muscle** (phase 2) does not have motor units; instead, it relies on the **Frank-Starling mechanism** and hormonal/nervous regulation to adjust its contractile force as a syncytium.
Muscle fiber types and recruitment US Medical PG Question 4: An investigator is examining tissue samples from various muscle tissue throughout the body. She notices that biopsies collected from a specific site have a high concentration of sarcoplasmic reticulum, mitochondria, and myoglobin; they also stain poorly for ATPase. Additionally, the cell surface membranes of the myocytes in the specimen lack voltage-gated calcium channels. These myocytes are found in the greatest concentration at which of the following sites?
- A. Ventricular myocardium
- B. Tunica media
- C. Lateral rectus muscle
- D. Glandular myoepithelium
- E. Semispinalis muscle (Correct Answer)
Muscle fiber types and recruitment Explanation: ***Semispinalis muscle***
- The described characteristics—**high concentration of sarcoplasmic reticulum, mitochondria, and myoglobin** with **poor ATPase staining**—are hallmarks of **Type I (slow-twitch oxidative) skeletal muscle fibers**.
- Postural muscles like the **semispinalis** (part of the erector spinae group) are predominantly composed of Type I fibers adapted for sustained, aerobic contraction to maintain posture.
- These fibers appear **red** due to high myoglobin content, have abundant mitochondria for aerobic metabolism, and stain **poorly for ATPase** (distinguishing them from Type II fast-twitch fibers).
- While all skeletal muscle does possess voltage-gated calcium channels for excitation-contraction coupling, the overall profile best matches slow-twitch postural muscles.
*Ventricular myocardium*
- While cardiac muscle has high mitochondria, myoglobin, and sarcoplasmic reticulum, it **does possess L-type voltage-gated calcium channels** on the sarcolemma, which are essential for cardiac excitation-contraction coupling.
- Cardiac muscle relies on **both** extracellular Ca²⁺ influx through these channels and calcium-induced calcium release from the SR.
- Cardiac muscle typically stains **strongly for ATPase**, not poorly.
*Tunica media*
- Composed of **vascular smooth muscle** with poorly developed sarcoplasmic reticulum and relatively few mitochondria compared to skeletal or cardiac muscle.
- Smooth muscle relies heavily on **extracellular calcium influx** and the calmodulin pathway for contraction.
- Not characterized by high myoglobin content.
*Lateral rectus muscle*
- This extraocular muscle contains predominantly **Type IIb fast-twitch glycolytic fibers** adapted for rapid, precise eye movements.
- These fibers have **low myoglobin** (white muscle), fewer mitochondria, and stain **strongly for ATPase**.
- Opposite profile from the described tissue.
*Glandular myoepithelium*
- Myoepithelial cells are specialized contractile cells in secretory glands with minimal sarcoplasmic reticulum and mitochondria.
- Function is brief contraction for secretion expulsion, not sustained aerobic work.
- Do not exhibit the high oxidative capacity described.
Muscle fiber types and recruitment US Medical PG Question 5: In skeletal muscle, which step of excitation-contraction coupling requires ATP?
- A. Cross-bridge cycling (Correct Answer)
- B. Action potential propagation
- C. Troponin binding to calcium
- D. Calcium release from SR
Muscle fiber types and recruitment Explanation: ***Cross-bridge cycling***
- ATP is essential for two key actions in **cross-bridge cycling**: the **detachment of myosin heads from actin** and the **re-cocking of the myosin heads** for the next power stroke.
- Without ATP, myosin heads remain attached to actin, leading to **rigor mortis**.
*Action potential propagation*
- This process involves the flow of **ions (Na+ and K+)** across the sarcolemma through voltage-gated channels, which is a passive event down their electrochemical gradients.
- While ion pumps (like the Na+/K+ pump) maintain these gradients over time, the **propagation itself is not a direct ATP-dependent step** in the immediate sense of the action potential.
*Troponin binding to calcium*
- The binding of **calcium to troponin C** is a passive chemical interaction driven by the *concentration gradient* of calcium ions.
- This binding triggers a **conformational change** in the troponin-tropomyosin complex, exposing actin binding sites, and does not directly consume ATP.
*Calcium release from SR*
- The release of calcium from the **sarcoplasmic reticulum (SR)** into the sarcoplasm occurs through **ryanodine receptors**, which are mechanically or voltage-gated channels.
- This is a passive efflux down the **calcium concentration gradient**, and does not directly consume ATP.
Muscle fiber types and recruitment US Medical PG Question 6: A 52-year-old man undergoes an exercise stress test for a 1-week history of squeezing substernal chest pain that is aggravated by exercise and relieved by rest. During the test, there is a substantial increase in the breakdown of glycogen in the muscle cells. Which of the following changes best explains this intracellular finding?
- A. Activation of phosphorylase kinase (Correct Answer)
- B. Decrease in protein kinase A
- C. Inactivation of glycogen synthase kinase
- D. Activation of protein phosphatase
- E. Increase in glucose-6-phosphate
Muscle fiber types and recruitment Explanation: ***Activation of phosphorylase kinase***
- Exercise, particularly in the context of **ischemic heart disease** suggested by the patient's symptoms, triggers a rapid need for energy, leading to **glycogenolysis**.
- **Phosphorylase kinase** is the key enzyme that activates **glycogen phosphorylase**, the rate-limiting step in glycogen breakdown, to release glucose-1-phosphate from glycogen stores.
*Decrease in protein kinase A*
- **Protein kinase A (PKA)** is typically activated during exercise via **epinephrine** signaling, which in turn *activates* phosphorylase kinase and *inhibits* glycogen synthase.
- A decrease in PKA activity would lead to *reduced* glycogen breakdown, which contradicts the described increase in glycogen breakdown.
*Inactivation of glycogen synthase kinase*
- **Glycogen synthase kinase (GSK3)** phosphorylates and inactivates **glycogen synthase**, thereby *inhibiting* glycogen synthesis.
- If GSK3 were inactivated, glycogen synthesis would be *promoted*, rather than glycogen breakdown, further contradicting the clinical scenario.
*Activation of protein phosphatase*
- **Protein phosphatases** generally remove phosphate groups, which would *deactivate* glycogen phosphorylase and *activate* glycogen synthase.
- This action would promote glycogen synthesis and inhibit glycogen breakdown, which is the opposite of the observed physiological response during exercise.
*Increase in glucose-6-phosphate*
- While **glucose-6-phosphate** is an intermediate in glycogen metabolism, an increase in its concentration would primarily signal abundant glucose and tend to *inhibit* glycogen phosphorylase and *activate* glycogen synthase.
- This effect would favor glycogen synthesis and inhibit its breakdown, making it an unlikely explanation for increased glycogen breakdown during exercise.
Muscle fiber types and recruitment US Medical PG Question 7: An investigator is studying muscle tissue in high-performance athletes. He obtains blood samples from athletes before and after a workout session consisting of short, fast sprints. Which of the following findings is most likely upon evaluation of blood obtained after the workout session?
- A. Decreased concentration of NADH
- B. Increased concentration of H+ (Correct Answer)
- C. Decreased concentration of lactate
- D. Increased concentration of insulin
- E. Increased concentration of ATP
Muscle fiber types and recruitment Explanation: ***Increased concentration of H+***
- During **anaerobic metabolism** in high-intensity exercise like sprints, pyruvate is converted to **lactate** by **lactate dehydrogenase** to regenerate NAD+. This process produces H+, leading to a decrease in pH and an increase in H+ concentration in the blood.
- The accumulation of **hydrogen ions (H+)** contributes to metabolic acidosis, muscle fatigue, and the burning sensation experienced during intense exertion.
- Blood gas analysis would show **decreased pH** and **increased H+ concentration**.
*Decreased concentration of NADH*
- NADH is primarily an **intracellular metabolite** and is not typically measured in blood samples as it does not circulate freely in significant concentrations.
- Within muscle cells during anaerobic glycolysis, NADH is consumed by lactate dehydrogenase to convert pyruvate to lactate, regenerating NAD+ for continued glycolysis.
- This option is not a realistic blood finding from a clinical laboratory perspective.
*Decreased concentration of lactate*
- **High-intensity sprints** primarily rely on **anaerobic metabolism**, which rapidly produces **lactate** from pyruvate.
- Therefore, the concentration of lactate in the blood would significantly **increase** after such a workout, not decrease.
- Elevated blood lactate is a hallmark finding after intense anaerobic exercise.
*Increased concentration of insulin*
- **Insulin** levels typically **decrease** during exercise, especially high-intensity exercise, due to **sympathetic nervous system activation** and the body's need to mobilize glucose from liver glycogen and fatty acids.
- Exercise promotes glucose uptake through **insulin-independent mechanisms** (GLUT4 translocation via AMP-activated protein kinase).
- Increased insulin would be counterproductive during intense exercise when glucose mobilization is needed.
*Increased concentration of ATP*
- ATP does not circulate in blood in measurable concentrations as a typical laboratory finding.
- Within muscle cells, ATP is rapidly **consumed** during intense exercise to fuel muscle contraction.
- While cells work to maintain ATP levels through anaerobic glycolysis and the creatine phosphate system, net ATP does not accumulate in the blood.
Muscle fiber types and recruitment US Medical PG Question 8: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Muscle fiber types and recruitment Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Muscle fiber types and recruitment US Medical PG Question 9: A 25-year-old woman presents to her primary care physician for her yearly physical exam. She has no past medical history and says that she does not currently have any health concerns. On physical exam, she is found to have hyperactive patellar reflexes but says that she has had this finding since she was a child. She asks her physician why this might be the case. Her physician explains that there are certain cells that are responsible for detecting muscle stretch and responding to restore the length of the muscle. Which of the following is most likely a characteristic of these structures?
- A. They inhibit the activity of alpha-motoneurons
- B. They activate inhibitory interneurons
- C. They are in parallel with extrafusal skeletal muscle fibers (Correct Answer)
- D. They are in series with extrafusal skeletal muscle fibers
- E. They are innervated by group Ib afferent neurons
Muscle fiber types and recruitment Explanation: ***They are in parallel with extrafusal skeletal muscle fibers***
- The structures described are **muscle spindles**, which are **stretch receptors** located within the muscle belly and arranged in parallel with **extrafusal muscle fibers**.
- This parallel arrangement allows them to detect changes in **muscle length** and the rate of change of length, initiating the **stretch reflex**.
*They inhibit the activity of alpha-motoneurons*
- Muscle spindles, primarily through their **Ia afferent fibers**, **excite** alpha-motoneurons, leading to muscle contraction and opposing the stretch.
- **Inhibition** of alpha-motoneurons is typically associated with structures like **Golgi tendon organs**, which respond to muscle tension.
*They activate inhibitory interneurons*
- While muscle spindles do excite **excitatory interneurons** that activate synergistic muscles, their primary action in the monosynaptic stretch reflex is direct excitation of **alpha-motoneurons**.
- **Inhibitory interneurons** are typically involved in mediating **reciprocal inhibition** of antagonistic muscles in response to muscle spindle activation.
*They are in series with extrafusal skeletal muscle fibers*
- Structures arranged in **series** with extrafusal muscle fibers are **Golgi tendon organs**, which are tension receptors.
- Muscle spindles are oriented **in parallel** to detect changes in muscle length.
*They are innervated by group Ib afferent neurons*
- Muscle spindles are primarily innervated by **group Ia (primary) afferent neurons** and **group II (secondary) afferent neurons**, which detect muscle length and rate of change of length.
- **Group Ib afferent neurons** innervate **Golgi tendon organs**, which are sensitive to muscle tension.
Muscle fiber types and recruitment US Medical PG Question 10: A 38-year-old woman presents to the physician’s clinic with a 6-month history of generalized weakness that usually worsens as the day progresses. She also complains of the drooping of her eyelids and double vision that is worse in the evening. Physical examination reveals bilateral ptosis after a sustained upward gaze and loss of eye convergence which improves upon placing ice packs over the eyes and after the administration of edrophonium. Which of the following is an intrinsic property of the muscle group affected in this patient?
- A. A small mass per motor unit
- B. High ATPase activity (Correct Answer)
- C. High myoglobin content
- D. High density of mitochondria
- E. Increased amount of ATP generated per molecule of glucose
Muscle fiber types and recruitment Explanation: ***High ATPase activity***
- This patient presents with **myasthenia gravis (MG)**, an autoimmune disorder affecting the neuromuscular junction through antibodies against acetylcholine receptors.
- **Extraocular muscles** and other muscles affected early in MG contain a high proportion of **fast-twitch (Type II) muscle fibers**, which are characterized by **high ATPase activity**.
- **Type II fibers** with high ATPase activity generate rapid, powerful contractions but are **more susceptible to neuromuscular junction dysfunction** due to their higher firing rates and greater dependence on efficient neuromuscular transmission.
- This intrinsic property (high ATPase activity) is why these muscles are preferentially affected in myasthenia gravis.
*A small mass per motor unit*
- While extraocular muscles do have **small motor units** (allowing for precise eye movements), this describes the **innervation pattern** rather than an intrinsic biochemical property of the muscle fibers themselves.
- The question specifically asks about an intrinsic property of the muscle group, referring to the metabolic and contractile characteristics of the muscle fibers.
*High myoglobin content*
- **High myoglobin content** is characteristic of **Type I (slow-twitch) oxidative fibers**, which rely on sustained oxygen delivery for prolonged, fatigue-resistant contractions.
- Muscles preferentially affected in MG have a higher proportion of **Type II fibers**, which have lower myoglobin content compared to Type I fibers.
*High density of mitochondria*
- **High mitochondrial density** is characteristic of **Type I (slow-twitch) oxidative fibers** that depend on aerobic metabolism for sustained energy production.
- While extraocular muscles do have oxidative capacity, the **Type II fibers** preferentially affected in MG have relatively lower mitochondrial density compared to Type I fibers and rely more on glycolytic metabolism for rapid energy needs.
*Increased amount of ATP generated per molecule of glucose*
- **Aerobic respiration** in Type I fibers generates approximately 32 ATP molecules per glucose through oxidative phosphorylation.
- **Type II fibers** rely more heavily on **anaerobic glycolysis**, which produces only 2 ATP per glucose molecule, making them less efficient in ATP generation per glucose.
- The muscles affected in MG have higher proportions of Type II fibers with lower ATP efficiency per glucose molecule.
More Muscle fiber types and recruitment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.