Metabolic changes with exercise US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metabolic changes with exercise. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metabolic changes with exercise US Medical PG Question 1: A 40-year-old female volunteers for an invasive study to measure her cardiac function. She has no previous cardiovascular history and takes no medications. With the test subject at rest, the following data is collected using blood tests, intravascular probes, and a closed rebreathing circuit:
Blood hemoglobin concentration 14 g/dL
Arterial oxygen content 0.22 mL O2/mL
Arterial oxygen saturation 98%
Venous oxygen content 0.17 mL O2/mL
Venous oxygen saturation 78%
Oxygen consumption 250 mL/min
The patient's pulse is 75/min, respiratory rate is 14/ min, and blood pressure is 125/70 mm Hg. What is the cardiac output of this volunteer?
- A. Body surface area is required to calculate cardiac output.
- B. Stroke volume is required to calculate cardiac output.
- C. 250 mL/min
- D. 5.0 L/min (Correct Answer)
- E. 50 L/min
Metabolic changes with exercise Explanation: ***5.0 L/min***
- Cardiac output can be calculated using the **Fick principle**: Cardiac Output $(\text{CO}) = \frac{{\text{Oxygen Consumption}}}{{\text{Arterial } \text{O}_2 \text{ Content} - \text{Venous O}_2 \text{ Content}}}$.
- Given Oxygen Consumption = 250 mL/min, Arterial O$_2$ Content = 0.22 mL/mL, and Venous O$_2$ Content = 0.17 mL/mL. Thus, CO = $\frac{{250 \text{ mL/min}}}{{(0.22 - 0.17) \text{ mL } \text{O}_2/\text{mL blood}}} = \frac{{250 \text{ mL/min}}}{{0.05 \text{ mL } \text{O}_2/\text{mL blood}}} = 5000 \text{ mL/min } = 5.0 \text{ L/min}$.
*Body surface area is required to calculate cardiac output.*
- **Body surface area (BSA)** is used to calculate **cardiac index**, which is cardiac output normalized to body size, but not cardiac output directly.
- While a normal cardiac output might be compared to a patient's BSA for context, it is not a necessary component for calculating the absolute cardiac output.
*Stroke volume is required to calculate cardiac output.*
- Cardiac output can be calculated as **Stroke Volume (SV) x Heart Rate (HR)**. However, stroke volume is not provided directly in this question.
- The Fick principle allows for the calculation of cardiac output **without explicit knowledge of stroke volume** or heart rate, using oxygen consumption and arteriovenous oxygen difference.
*250 mL/min*
- 250 mL/min represents the **oxygen consumption**, not the cardiac output.
- Cardiac output is the volume of blood pumped by the heart per minute, which is influenced by both oxygen consumption and the difference in oxygen content between arterial and venous blood.
*50 L/min*
- A cardiac output of 50 L/min is an **extremely high and physiologically impossible** value for a resting individual.
- This value is 10 times higher than the calculated cardiac output and typically represents a calculation error.
Metabolic changes with exercise US Medical PG Question 2: A scientist is trying to design a drug to modulate cellular metabolism in the treatment of obesity. Specifically, he is interested in understanding how fats are processed in adipocytes in response to different energy states. His target is a protein within these cells that catalyzes catabolism of an energy source. The products of this reaction are subsequently used in gluconeogenesis or β-oxidation. Which of the following is true of the most likely protein that is being studied by this scientist?
- A. It is stimulated by epinephrine (Correct Answer)
- B. It is inhibited by glucagon
- C. It is inhibited by acetylcholine
- D. It is inhibited by cortisol
- E. It is stimulated by insulin
Metabolic changes with exercise Explanation: ***It is stimulated by epinephrine***
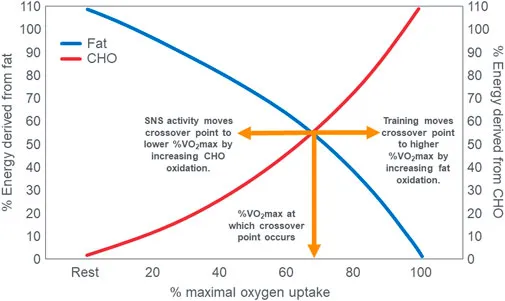
- The protein described is likely **hormone-sensitive lipase (HSL)**, which catabolizes **triglycerides** in adipocytes to **glycerol** and **fatty acids**.
- **Epinephrine** (and norepinephrine) stimulates HSL activity via a **cAMP-dependent protein kinase A (PKA)** pathway, leading to increased fatty acid release for energy.
*It is inhibited by glucagon*
- **Glucagon primarily acts on the liver** to promote gluconeogenesis and glycogenolysis, but it does **not directly inhibit HSL** in adipocytes.
- While glucagon has a lipolytic effect, it doesn't inhibit the enzyme that releases fatty acids.
*It is inhibited by acetylcholine*
- **Acetylcholine** is a neurotransmitter involved in the **parasympathetic nervous system**, which generally promotes energy storage.
- It does **not directly inhibit HSL**; its effects on lipid metabolism are indirect and typically involve other pathways.
*It is inhibited by cortisol*
- **Cortisol**, a glucocorticoid, generally **promotes lipolysis** (breakdown of fats) in certain contexts, particularly during stress to provide energy substrates.
- Therefore, it would **not inhibit HSL**; rather, it often enhances its activity or provides a permissive effect for other lipolytic hormones.
*It is stimulated by insulin*
- **Insulin** is an **anabolic hormone** that promotes energy storage, including **lipogenesis** (fat synthesis) and inhibits lipolysis.
- Insulin **inhibits HSL activity** by activating phosphodiesterase, which reduces cAMP levels, thus deactivating PKA and preventing HSL phosphorylation.
Metabolic changes with exercise US Medical PG Question 3: During exercise, what is the primary mechanism for increased oxygen delivery to active muscles?
- A. Decreased blood viscosity
- B. Increased cardiac output (Correct Answer)
- C. Increased hemoglobin affinity
- D. Enhanced oxygen diffusion
Metabolic changes with exercise Explanation: ***Increased cardiac output***
- During exercise, **cardiac output** increases significantly due to both an elevated **heart rate** and increased **stroke volume**, directly pushing more oxygenated blood to the active muscles.
- This augmentation in blood flow is the primary factor ensuring a sufficient supply of oxygen and nutrients to meet the heightened metabolic demands of exercising muscles.
*Decreased blood viscosity*
- While factors like **hemodilution** can decrease blood viscosity during prolonged exercise, this effect is relatively minor and not the primary mechanism for acute increases in oxygen delivery compared to the dramatic increase in cardiac output.
- A decrease in blood viscosity can slightly improve flow efficiency, but it doesn't fundamentally change the amount of blood pumped per minute to the muscles.
*Increased hemoglobin affinity*
- An *increased* hemoglobin affinity for oxygen would actually make it *harder* for oxygen to unload from hemoglobin to the tissues, which is counterproductive for oxygen delivery during exercise.
- In fact, during exercise, local conditions like increased temperature, decreased pH (**Bohr effect**), and increased 2,3-BPG tend to *decrease* hemoglobin's affinity for oxygen, facilitating oxygen release to active muscles.
*Enhanced oxygen diffusion*
- While exercise does improve the efficiency of oxygen extraction at the tissue level due to a steeper partial pressure gradient and increased capillary recruitment, the *rate* of oxygen diffusion across the capillary membrane isn't the primary modulator of overall oxygen delivery.
- The main determinant is the *amount* of oxygenated blood reaching the muscle, which is governed by cardiac output and local blood flow regulation.
Metabolic changes with exercise US Medical PG Question 4: During a clinical study evaluating the effects of exercise on muscle perfusion, 15 healthy individuals perform a 20-minute treadmill run at submaximal effort. Before and after the treadmill session, perfusion of the quadriceps muscle is evaluated with contrast-enhanced magnetic resonance imaging. The study shows a significant increase in muscle blood flow per unit of tissue mass. Which of the following local changes is most likely involved in the observed change in perfusion?
- A. Increase in adenosine (Correct Answer)
- B. Decrease in potassium
- C. Increase in thromboxane A2
- D. Increase in endothelin
- E. Decrease in prostacyclin
Metabolic changes with exercise Explanation: ***Increase in adenosine***
- **Adenosine** is a potent **vasodilator** released by metabolically active tissues, particularly in response to increased oxygen demand and ATP hydrolysis during exercise.
- Its accumulation leads to relaxation of vascular smooth muscle, increasing blood flow to meet the muscles' elevated metabolic needs.
*Decrease in potassium*
- An increase in **extracellular potassium** (not a decrease) generally causes vasodilation in skeletal muscle by hyperpolarizing smooth muscle cells.
- A decrease in potassium outside the cell would not be expected to cause vasodilation and increased perfusion during exercise.
*Increase in thromboxane A2*
- **Thromboxane A2** is primarily a **vasoconstrictor** and platelet aggregator, mainly involved in hemostasis and inflammation.
- Increased levels would lead to reduced blood flow, not the observed increase in perfusion during exercise.
*Increase in endothelin*
- **Endothelin** is one of the most potent **vasoconstrictors** known, primarily released from endothelial cells.
- An increase in endothelin would severely constrict blood vessels and decrease muscle perfusion, counteracting the effects of exercise.
*Decrease in prostacyclin*
- **Prostacyclin (PGI2)** is a potent **vasodilator** and inhibitor of platelet aggregation.
- A decrease in prostacyclin would lead to vasoconstriction and reduced blood flow, which is contrary to the increased perfusion seen during exercise.
Metabolic changes with exercise US Medical PG Question 5: A 52-year-old man undergoes an exercise stress test for a 1-week history of squeezing substernal chest pain that is aggravated by exercise and relieved by rest. During the test, there is a substantial increase in the breakdown of glycogen in the muscle cells. Which of the following changes best explains this intracellular finding?
- A. Activation of phosphorylase kinase (Correct Answer)
- B. Decrease in protein kinase A
- C. Inactivation of glycogen synthase kinase
- D. Activation of protein phosphatase
- E. Increase in glucose-6-phosphate
Metabolic changes with exercise Explanation: ***Activation of phosphorylase kinase***
- Exercise, particularly in the context of **ischemic heart disease** suggested by the patient's symptoms, triggers a rapid need for energy, leading to **glycogenolysis**.
- **Phosphorylase kinase** is the key enzyme that activates **glycogen phosphorylase**, the rate-limiting step in glycogen breakdown, to release glucose-1-phosphate from glycogen stores.
*Decrease in protein kinase A*
- **Protein kinase A (PKA)** is typically activated during exercise via **epinephrine** signaling, which in turn *activates* phosphorylase kinase and *inhibits* glycogen synthase.
- A decrease in PKA activity would lead to *reduced* glycogen breakdown, which contradicts the described increase in glycogen breakdown.
*Inactivation of glycogen synthase kinase*
- **Glycogen synthase kinase (GSK3)** phosphorylates and inactivates **glycogen synthase**, thereby *inhibiting* glycogen synthesis.
- If GSK3 were inactivated, glycogen synthesis would be *promoted*, rather than glycogen breakdown, further contradicting the clinical scenario.
*Activation of protein phosphatase*
- **Protein phosphatases** generally remove phosphate groups, which would *deactivate* glycogen phosphorylase and *activate* glycogen synthase.
- This action would promote glycogen synthesis and inhibit glycogen breakdown, which is the opposite of the observed physiological response during exercise.
*Increase in glucose-6-phosphate*
- While **glucose-6-phosphate** is an intermediate in glycogen metabolism, an increase in its concentration would primarily signal abundant glucose and tend to *inhibit* glycogen phosphorylase and *activate* glycogen synthase.
- This effect would favor glycogen synthesis and inhibit its breakdown, making it an unlikely explanation for increased glycogen breakdown during exercise.
Metabolic changes with exercise US Medical PG Question 6: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Metabolic changes with exercise Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Metabolic changes with exercise US Medical PG Question 7: During heavy exercise, what is the primary mechanism for maintaining arterial pH despite increased lactic acid production?
- A. Increased bicarbonate reabsorption
- B. Phosphate buffering
- C. Increased hydrogen secretion
- D. Hyperventilation (Correct Answer)
Metabolic changes with exercise Explanation: ***Hyperventilation***
- **Hyperventilation** during heavy exercise increases the expulsion of **carbon dioxide (CO2)**, shifting the **bicarbonate buffer system** equilibrium to the left.
- This reduction in **CO2** effectively removes **hydrogen ions (H+)**, thereby helping to maintain **arterial pH** despite rising **lactic acid** levels.
*Increased bicarbonate reabsorption*
- While the kidneys adapt by increasing **bicarbonate reabsorption** to compensate for acidosis, this is a **slower renal mechanism** for pH regulation, taking hours to days, rather than an immediate response during acute exercise.
- The rapid pH regulation during exercise primarily relies on respiratory and chemical buffer systems, not renal function.
*Phosphate buffering*
- The **phosphate buffer system** is indeed important for intracellular and renal tubular fluid buffering.
- However, its buffering capacity in the extracellular fluid and plasma is relatively limited compared to the **bicarbonate system** due to its lower concentration.
*Increased hydrogen secretion*
- **Increased hydrogen secretion** by the renal tubules is a long-term mechanism for compensating for acidosis, which helps excrete excess **acid** and regenerate **bicarbonate**.
- This is a slow, renal regulatory process and not the primary rapid mechanism for maintaining pH during the immediate demands of heavy exercise.
Metabolic changes with exercise US Medical PG Question 8: A 24-year-old man is running a marathon. Upon reaching the finish line, his serum lactate levels were measured and were significantly increased as compared to his baseline. Which of the following pathways converts the lactate produced by muscles into glucose and transports it back to the muscles?
- A. Citric acid cycle
- B. Glycolysis
- C. Glycogenesis
- D. Pentose phosphate pathway
- E. Cori cycle (Correct Answer)
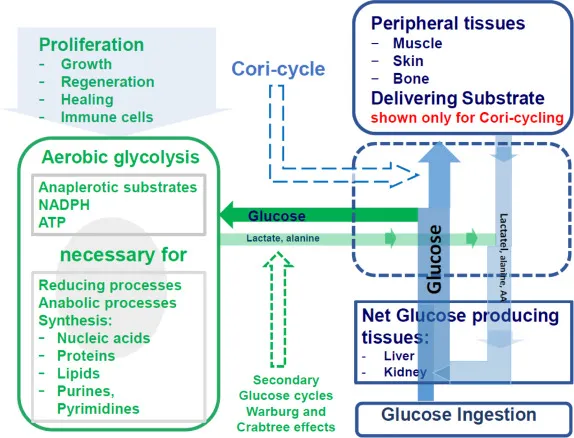
Metabolic changes with exercise Explanation: ***Cori cycle***
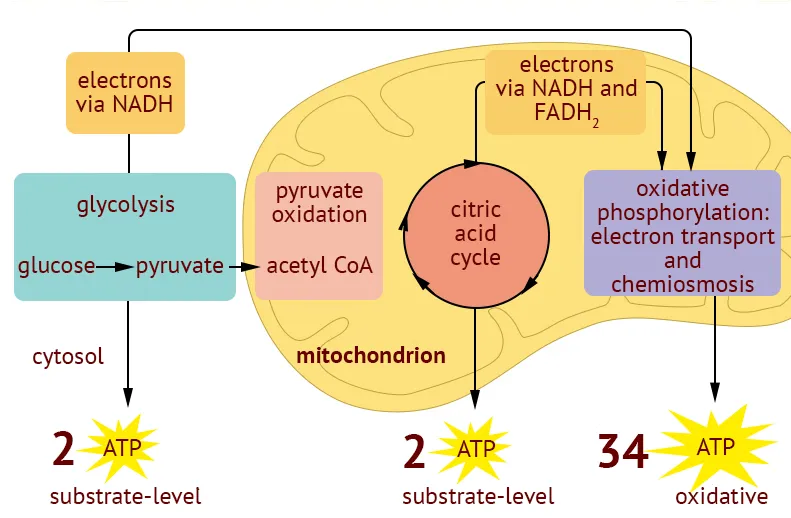
- The **Cori cycle** is the metabolic pathway that converts **lactate** produced by anaerobic glycolysis in muscles (especially during intense exercise) back to **glucose in the liver** via gluconeogenesis.
- During strenuous exercise, muscles rely on anaerobic glycolysis when oxygen supply is insufficient, producing lactate and 2 ATP per glucose.
- The lactate is transported via bloodstream to the liver, where it is converted back to glucose (requiring 6 ATP), which then returns to muscles for energy or glycogen storage.
- This cycle allows muscles to continue generating ATP anaerobically while the liver handles lactate clearance.
*Citric acid cycle*
- The **citric acid cycle** (Krebs cycle) oxidizes **acetyl-CoA** to generate ATP, NADH, and FADH₂ in the mitochondrial matrix under aerobic conditions.
- It does not convert lactate to glucose; rather, pyruvate can be converted to acetyl-CoA to enter this cycle for complete oxidation.
- This is an aerobic process and does not involve the liver-muscle lactate-glucose exchange.
*Glycolysis*
- **Glycolysis** is the metabolic pathway that breaks down **glucose into pyruvate**, generating 2 ATP and 2 NADH per glucose molecule.
- Under anaerobic conditions, pyruvate is converted to lactate to regenerate NAD⁺ for continued glycolysis.
- This is the opposite of what the question asks—glycolysis produces lactate from glucose, not glucose from lactate.
*Glycogenesis*
- **Glycogenesis** is the process of synthesizing **glycogen from glucose** for storage, primarily in liver and muscle tissue.
- While it involves glucose storage, it does not convert lactate back to glucose or involve the metabolic exchange between muscles and liver described in the question.
*Pentose phosphate pathway*
- The **pentose phosphate pathway** (hexose monophosphate shunt) produces **NADPH** for reductive biosynthesis and **ribose-5-phosphate** for nucleotide synthesis.
- It branches from glycolysis but is not involved in lactate metabolism or the muscle-liver glucose-lactate exchange.
Metabolic changes with exercise US Medical PG Question 9: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Metabolic changes with exercise Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Metabolic changes with exercise US Medical PG Question 10: A 37-year-old man presents to his primary care physician because he has been experiencing episodes where he wakes up at night gasping for breath. His past medical history is significant for morbid obesity as well as hypertension for which he takes lisinopril. He is diagnosed with sleep apnea and prescribed a continuous positive airway pressure apparatus. In addition, the physician discusses making lifestyle and behavioral changes such as dietary modifications and exercise. The patient agrees to attempt these behavioral changes. Which of the following is most likely to result in improving patient adherence to this plan?
- A. Refer the patient to a peer support group addressing lifestyle changes
- B. Ask the patient to bring a family member to next appointment
- C. Provide follow-up appointments to assess progress in attaining goals (Correct Answer)
- D. Provide appropriate publications for the patient's educational level
- E. Inform the patient of the health consequences of not intervening
Metabolic changes with exercise Explanation: ***Provide follow-up appointments to assess progress in attaining goals***
- **Regular follow-up appointments** provide accountability and opportunities to discuss progress, troubleshoot challenges, and reinforce motivation for lifestyle changes
- This approach fosters a **patient-centered relationship** where the physician actively participates in the patient's journey, increasing adherence
- Evidence supports that scheduled follow-up is one of the most effective interventions for improving adherence to chronic disease management plans
*Refer the patient to a peer support group addressing lifestyle changes*
- While peer support can be beneficial for some patients, it is **not universally effective** and might not be suitable for all patients, especially as a primary strategy for adherence
- The effectiveness of such groups varies widely based on the patient's personality and group dynamics, potentially leading to **inconsistent adherence**
*Ask the patient to bring a family member to next appointment*
- Involving family can be supportive, but it may not always be appropriate or desired by the patient and doesn't directly address the patient's individual motivation or challenges
- While family support can enhance adherence, this approach is supplementary rather than primary in effectiveness
*Provide appropriate publications for the patient's educational level*
- Providing educational materials is a good initial step, but information alone is often **insufficient to sustain long-term behavioral changes**
- Without active follow-up and personalized guidance, written materials can be easily forgotten or not fully implemented into daily life
*Inform the patient of the health consequences of not intervening*
- While explaining risks is crucial for informed consent and awareness, relying solely on **fear-based motivation** often has limited long-term effectiveness in promoting sustained behavioral change
- Patients are often aware of potential negative consequences, but this knowledge alone does not provide the practical support or strategies needed for adherence
More Metabolic changes with exercise US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.