Fatigue mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fatigue mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fatigue mechanisms US Medical PG Question 1: A 52-year-old woman presents to her primary care physician for her annual checkup. She lost her job 6 months ago and since then she has been feeling worthless because nobody wants to hire her. She also says that she is finding it difficult to concentrate, which is exacerbated by the fact that she has lost interest in activities that she used to love such as doing puzzles and working in the garden. She says that she is sleeping over 10 hours every day because she says it is difficult to find the energy to get up in the morning. She denies having any thoughts about suicide. Which of the following neurotransmitter profiles would most likely be seen in this patient?
- A. Increased dopamine
- B. Decreased serotonin and norepinephrine (Correct Answer)
- C. Increased norepinephrine
- D. Decreased acetylcholine
- E. Decreased gamma-aminobutyric acid
Fatigue mechanisms Explanation: ***Decreased serotonin and norepinephrine***
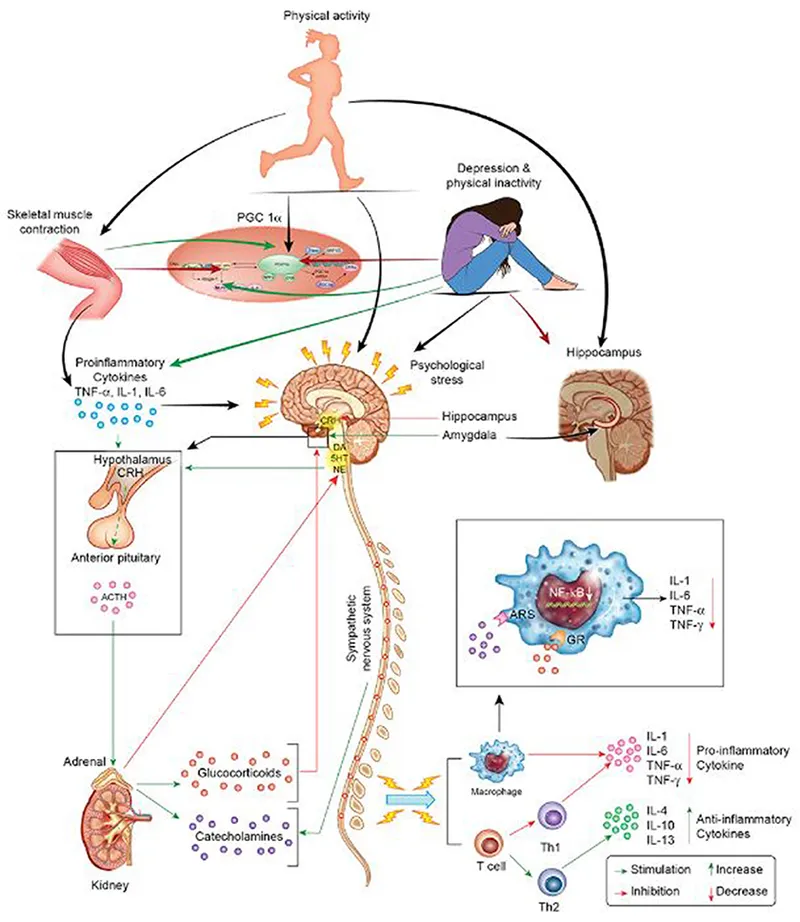
- The patient's symptoms, including **worthlessness**, difficulty **concentrating**, loss of **interest (anhedonia)**, and **hypersomnia**, are classic for **major depressive disorder**.
- **Depression** is most commonly associated with a deficiency in **monoamine neurotransmitters**, particularly **serotonin** and **norepinephrine**, which play key roles in mood, sleep, appetite, and cognition.
*Increased dopamine*
- **Increased dopamine** activity is more often associated with conditions like **psychosis (e.g., schizophrenia)** or the manic phases of **bipolar disorder**, which are not indicated by the patient's symptoms.
- While dopamine is involved in reward and motivation, a primary increase is not the typical finding in major depression.
*Increased norepinephrine*
- An **increase in norepinephrine** is often seen in conditions like **anxiety disorders**, **panic attacks**, or **mania**, characterized by states of heightened arousal and vigilance.
- The patient's symptoms of **lethargy**, **hypersomnia**, and **lack of energy** point away from an overall increase in norepinephrine.
*Decreased acetylcholine*
- **Decreased acetylcholine** is primarily linked to cognitive deficits seen in conditions like **Alzheimer's disease**, affecting memory and learning.
- While depression can involve cognitive impairment, a primary deficit in acetylcholine is not the hallmark neurotransmitter change in major depressive disorder.
*Decreased gamma-aminobutyric acid*
- **Decreased GABA** (gamma-aminobutyric acid) is primarily associated with conditions of heightened excitability and anxiety, such as **anxiety disorders**, **insomnia**, and **seizure disorders**.
- The patient's presentation of **hypersomnia** and **low energy** is inconsistent with a primary GABA deficiency.
Fatigue mechanisms US Medical PG Question 2: During exercise, what is the primary mechanism for increased oxygen delivery to active muscles?
- A. Decreased blood viscosity
- B. Increased cardiac output (Correct Answer)
- C. Increased hemoglobin affinity
- D. Enhanced oxygen diffusion
Fatigue mechanisms Explanation: ***Increased cardiac output***
- During exercise, **cardiac output** increases significantly due to both an elevated **heart rate** and increased **stroke volume**, directly pushing more oxygenated blood to the active muscles.
- This augmentation in blood flow is the primary factor ensuring a sufficient supply of oxygen and nutrients to meet the heightened metabolic demands of exercising muscles.
*Decreased blood viscosity*
- While factors like **hemodilution** can decrease blood viscosity during prolonged exercise, this effect is relatively minor and not the primary mechanism for acute increases in oxygen delivery compared to the dramatic increase in cardiac output.
- A decrease in blood viscosity can slightly improve flow efficiency, but it doesn't fundamentally change the amount of blood pumped per minute to the muscles.
*Increased hemoglobin affinity*
- An *increased* hemoglobin affinity for oxygen would actually make it *harder* for oxygen to unload from hemoglobin to the tissues, which is counterproductive for oxygen delivery during exercise.
- In fact, during exercise, local conditions like increased temperature, decreased pH (**Bohr effect**), and increased 2,3-BPG tend to *decrease* hemoglobin's affinity for oxygen, facilitating oxygen release to active muscles.
*Enhanced oxygen diffusion*
- While exercise does improve the efficiency of oxygen extraction at the tissue level due to a steeper partial pressure gradient and increased capillary recruitment, the *rate* of oxygen diffusion across the capillary membrane isn't the primary modulator of overall oxygen delivery.
- The main determinant is the *amount* of oxygenated blood reaching the muscle, which is governed by cardiac output and local blood flow regulation.
Fatigue mechanisms US Medical PG Question 3: An investigator is examining tissue samples from various muscle tissue throughout the body. She notices that biopsies collected from a specific site have a high concentration of sarcoplasmic reticulum, mitochondria, and myoglobin; they also stain poorly for ATPase. Additionally, the cell surface membranes of the myocytes in the specimen lack voltage-gated calcium channels. These myocytes are found in the greatest concentration at which of the following sites?
- A. Ventricular myocardium
- B. Tunica media
- C. Lateral rectus muscle
- D. Glandular myoepithelium
- E. Semispinalis muscle (Correct Answer)
Fatigue mechanisms Explanation: ***Semispinalis muscle***
- The described characteristics—**high concentration of sarcoplasmic reticulum, mitochondria, and myoglobin** with **poor ATPase staining**—are hallmarks of **Type I (slow-twitch oxidative) skeletal muscle fibers**.
- Postural muscles like the **semispinalis** (part of the erector spinae group) are predominantly composed of Type I fibers adapted for sustained, aerobic contraction to maintain posture.
- These fibers appear **red** due to high myoglobin content, have abundant mitochondria for aerobic metabolism, and stain **poorly for ATPase** (distinguishing them from Type II fast-twitch fibers).
- While all skeletal muscle does possess voltage-gated calcium channels for excitation-contraction coupling, the overall profile best matches slow-twitch postural muscles.
*Ventricular myocardium*
- While cardiac muscle has high mitochondria, myoglobin, and sarcoplasmic reticulum, it **does possess L-type voltage-gated calcium channels** on the sarcolemma, which are essential for cardiac excitation-contraction coupling.
- Cardiac muscle relies on **both** extracellular Ca²⁺ influx through these channels and calcium-induced calcium release from the SR.
- Cardiac muscle typically stains **strongly for ATPase**, not poorly.
*Tunica media*
- Composed of **vascular smooth muscle** with poorly developed sarcoplasmic reticulum and relatively few mitochondria compared to skeletal or cardiac muscle.
- Smooth muscle relies heavily on **extracellular calcium influx** and the calmodulin pathway for contraction.
- Not characterized by high myoglobin content.
*Lateral rectus muscle*
- This extraocular muscle contains predominantly **Type IIb fast-twitch glycolytic fibers** adapted for rapid, precise eye movements.
- These fibers have **low myoglobin** (white muscle), fewer mitochondria, and stain **strongly for ATPase**.
- Opposite profile from the described tissue.
*Glandular myoepithelium*
- Myoepithelial cells are specialized contractile cells in secretory glands with minimal sarcoplasmic reticulum and mitochondria.
- Function is brief contraction for secretion expulsion, not sustained aerobic work.
- Do not exhibit the high oxidative capacity described.
Fatigue mechanisms US Medical PG Question 4: In skeletal muscle, which step of excitation-contraction coupling requires ATP?
- A. Cross-bridge cycling (Correct Answer)
- B. Action potential propagation
- C. Troponin binding to calcium
- D. Calcium release from SR
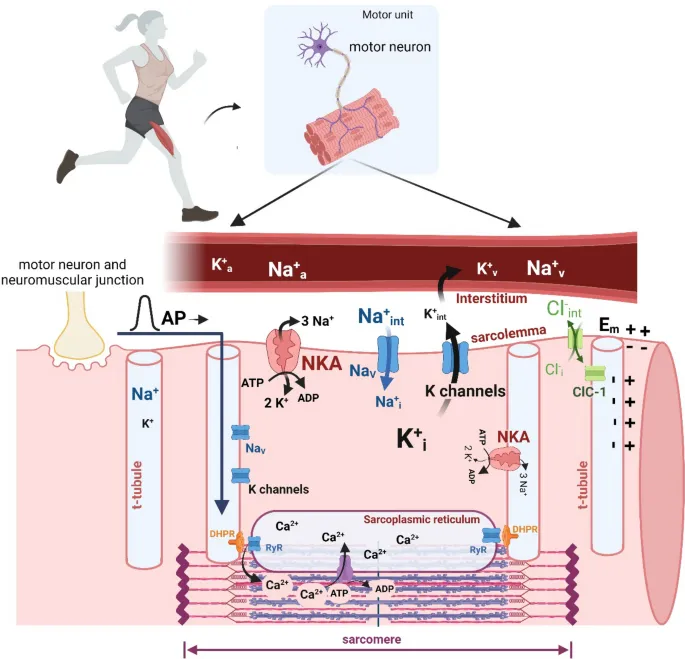
Fatigue mechanisms Explanation: ***Cross-bridge cycling***
- ATP is essential for two key actions in **cross-bridge cycling**: the **detachment of myosin heads from actin** and the **re-cocking of the myosin heads** for the next power stroke.
- Without ATP, myosin heads remain attached to actin, leading to **rigor mortis**.
*Action potential propagation*
- This process involves the flow of **ions (Na+ and K+)** across the sarcolemma through voltage-gated channels, which is a passive event down their electrochemical gradients.
- While ion pumps (like the Na+/K+ pump) maintain these gradients over time, the **propagation itself is not a direct ATP-dependent step** in the immediate sense of the action potential.
*Troponin binding to calcium*
- The binding of **calcium to troponin C** is a passive chemical interaction driven by the *concentration gradient* of calcium ions.
- This binding triggers a **conformational change** in the troponin-tropomyosin complex, exposing actin binding sites, and does not directly consume ATP.
*Calcium release from SR*
- The release of calcium from the **sarcoplasmic reticulum (SR)** into the sarcoplasm occurs through **ryanodine receptors**, which are mechanically or voltage-gated channels.
- This is a passive efflux down the **calcium concentration gradient**, and does not directly consume ATP.
Fatigue mechanisms US Medical PG Question 5: A 55-year-old man presents to his physician with weakness and fatigue for 1 week. There is no significant past medical history. He mentions that he is very health conscious and has heard about the health benefits of juices. He is following a juice-only diet for the last 2 weeks. His physical examination is completely normal, except for depressed deep tendon reflexes. The only abnormality in a complete laboratory evaluation is a serum potassium level of 6.0 mEq/L (6.0 mmol/L). There are significantly peaked T-waves on ECG. Which of the following pathophysiologic mechanisms best explains the patient’s symptoms?
- A. Decreased resting membrane potential of skeletal muscle cells (Correct Answer)
- B. Prolonged release of Ca2+ ions after stimulation of Ryanodine receptors
- C. Hyperpolarization of skeletal muscle cells
- D. Dysfunction of Na+ channels
- E. Dysfunction of dystrophin-glycoprotein complex
Fatigue mechanisms Explanation: ***Decreased resting membrane potential of skeletal muscle cells***
- The patient's **hyperkalemia** (serum potassium 6.0 mEq/L), evidenced by peaked T-waves, reduces the electrochemical gradient for potassium, making the **resting membrane potential less negative (more depolarized)**.
- While seemingly contradictory, a persistent partial depolarization due to high extracellular potassium can lead to inactivation of voltage-gated sodium channels, preventing the generation of new action potentials and causing **muscle weakness and depressed reflexes**.
*Prolonged release of Ca2+ ions after stimulation of Ryanodine receptors*
- This mechanism is associated with conditions like **malignant hyperthermia** or certain myopathies, characterized by muscle rigidity, cramps, or excessive heat production, which are not seen here.
- Hyperkalemia primarily affects **membrane excitability** rather than intracellular calcium release pathways directly.
*Hyperpolarization of skeletal muscle cells*
- **Hyperpolarization** would make the resting membrane potential more negative, making it harder to reach the threshold for an action potential, leading to weakness.
- This typically occurs in conditions causing **hypokalemia**, as a lower extracellular potassium concentration increases the electrochemical gradient and causes a net efflux of potassium ions.
*Dysfunction of Na+ channels*
- Dysfunction of **sodium channels** can cause various neuromuscular disorders, including periodic paralysis or myotonic conditions.
- While hyperkalemia indirectly affects sodium channel function by altering the resting membrane potential, the primary pathophysiologic insult here is the altered potassium gradient, not an intrinsic channel defect.
*Dysfunction of dystrophin-glycoprotein complex*
- This complex is crucial for maintaining muscle fiber integrity and is defective in **muscular dystrophies** (e.g., Duchenne muscular dystrophy).
- Such conditions cause progressive muscle degeneration and weakness, which develop over a much longer period than the acute symptoms described here and are not related to electrolyte imbalances.
Fatigue mechanisms US Medical PG Question 6: A 22-year-old medical student decides to fast for 24 hours after reading about the possible health benefits of fasting. She read that blood glucose levels are maintained by metabolic processes such as hepatic glycogenolysis and hepatic gluconeogenesis during the initial 3 days of fasting. During the day, she did not suffer from the symptoms of hypoglycemia. Which of the following signaling molecules most likely stimulated the reaction which maintained her blood glucose after all her stored glucose was broken down and used up?
- A. Adenosine diphosphate
- B. Acetyl CoA (Correct Answer)
- C. Acetate
- D. Citrate
- E. Adenosine monophosphate
Fatigue mechanisms Explanation: ***Acetyl CoA***
- **Acetyl CoA** is the key **allosteric activator of pyruvate carboxylase**, the first committed enzyme of gluconeogenesis that converts pyruvate to oxaloacetate.
- During prolonged fasting after glycogen stores are depleted, the body shifts to **fatty acid oxidation** (β-oxidation), which produces large amounts of **Acetyl CoA**.
- High **Acetyl CoA** levels signal that fat is being oxidized for energy, and simultaneously **activate gluconeogenesis** to maintain blood glucose for glucose-dependent tissues (brain, RBCs).
- This is the primary signaling mechanism that directly stimulates the gluconeogenic pathway after glycogen is exhausted.
*Adenosine monophosphate (AMP)*
- **AMP** levels rise during energy depletion and activate **AMP-activated protein kinase (AMPK)**.
- However, AMPK **inhibits gluconeogenesis** (not stimulates it) because gluconeogenesis is an **ATP-consuming** anabolic process (requires 6 ATP per glucose).
- AMPK promotes ATP-generating catabolic processes like fatty acid oxidation, but suppresses ATP-consuming processes like gluconeogenesis and fatty acid synthesis.
*Adenosine diphosphate (ADP)*
- **ADP** accumulates when ATP is hydrolyzed and signals moderate energy deficit.
- ADP is primarily a substrate for ATP regeneration via oxidative phosphorylation and does not directly regulate gluconeogenesis.
- Its role in metabolic regulation is less specific than allosteric activators like Acetyl CoA.
*Acetate*
- **Acetate** can be converted to Acetyl CoA but is not a direct signaling molecule for gluconeogenesis.
- It is a minor metabolite that may be produced in specific conditions (e.g., alcohol metabolism, ketoacidosis) but does not play a primary role in fasting-induced glucose homeostasis.
*Citrate*
- **Citrate** is a Krebs cycle intermediate that inhibits **phosphofructokinase-1 (PFK-1)** in glycolysis, thus reducing glucose breakdown.
- While citrate inhibition of glycolysis indirectly favors gluconeogenesis by preventing futile cycling, citrate does not **directly activate** gluconeogenic enzymes.
- Citrate primarily signals energy sufficiency and promotes fatty acid synthesis in the fed state, not fasting gluconeogenesis.
Fatigue mechanisms US Medical PG Question 7: A 71-year-old woman comes to the physician because of an 8-month history of fatigue. Laboratory studies show a hemoglobin concentration of 13.3 g/dL, a serum creatinine concentration of 0.9 mg/dL, and a serum alkaline phosphatase concentration of 100 U/L. Laboratory evaluation of which of the following parameters would be most helpful in determining the cause of this patient's symptoms?
- A. Cancer antigen 27-29
- B. Calcitriol
- C. Lactate dehydrogenase
- D. Ferritin (Correct Answer)
- E. Gamma-glutamyl transpeptidase
Fatigue mechanisms Explanation: ***Correct: Ferritin***
- The patient's fatigue associated with a normal hemoglobin and creatinine suggests a subtle cause for fatigue, and **iron deficiency without anemia** (iron deficiency anemia can cause decrease in hemoglobin levels) is a common cause, which would be identified by low ferritin levels.
- Ferritin is a **storage protein for iron**, and its levels accurately reflect the body's iron stores and are the most sensitive indicator for iron deficiency.
*Incorrect: Cancer antigen 27-29*
- This marker is primarily used to monitor **breast cancer recurrence** or progression, not for initial diagnosis or as a general screen for fatigue.
- There is no clinical indication in the patient's presentation that suggests breast cancer, making this an unlikely and unhelpful test.
*Incorrect: Calcitriol*
- Calcitriol is the active form of vitamin D, primarily involved in **calcium and phosphorus metabolism** and bone health.
- While vitamin D deficiency can cause fatigue, the patient's normal alkaline phosphatase (ALP is elevated in vitamin D deficiency due to secondary hyperparathyroidism) and absence of other related symptoms make calcitriol assessment less likely to be the most helpful first step.
*Incorrect: Lactate dehydrogenase*
- **LDH is a general marker of tissue damage and cell turnover**, elevated in conditions like hemolysis, malignancy, or liver disease.
- It is a non-specific marker that would not pinpoint the cause of fatigue in this patient with otherwise normal baseline labs.
*Incorrect: Gamma-glutamyl transpeptidase*
- GGT is an enzyme primarily used to assess **liver function and bile duct obstruction**, often in conjunction with alkaline phosphatase.
- Given the patient's normal alkaline phosphatase and no other signs of liver disease, GGT would not be a helpful test for fatigue in this context.
Fatigue mechanisms US Medical PG Question 8: An investigator is studying muscle contraction in tissue obtained from the thigh muscle of an experimental animal. After injection of radiolabeled ATP, the tissue is stimulated with electrical impulses. Radioassay of these muscle cells is most likely to show greatest activity in which of the following structures?
- A. H zone
- B. M line
- C. A band (Correct Answer)
- D. Z line
- E. I band
Fatigue mechanisms Explanation: ***A band***
- The **A band** contains the entire length of the **thick myosin filaments** along with the **overlap zone** where myosin and actin interact. Myosin has **ATPase activity**, meaning it binds and hydrolyzes **ATP** to power muscle contraction through cross-bridge cycling.
- Therefore, the greatest accumulation of **radiolabeled ATP** and its breakdown products would be found where **myosin heads** are located throughout the A band.
- The A band represents the most complete answer as it encompasses all regions containing myosin ATPase activity.
*H zone*
- The **H zone** is the central part of the **A band** where only **thick myosin filaments** are present, with no overlap with thin actin filaments.
- While myosin heads with ATPase activity are present here and would show radiolabeled ATP, the **H zone** is only a **subset** of the A band. The **A band** is the more comprehensive answer as it includes both the H zone and the overlap regions where most cross-bridge cycling occurs.
*M line*
- The **M line** is the very center of the **H zone** and anchors the **thick filaments**.
- It consists of structural proteins like **myomesin** and **creatine kinase**. While creatine kinase can phosphorylate ADP to regenerate ATP, it does not directly hydrolyze ATP for muscle contraction the way myosin ATPase does.
*Z line*
- The **Z line** (or Z disc) marks the boundaries of a **sarcomere** and anchors the **thin actin filaments**.
- It contains proteins like **alpha-actinin** and **desmin** but does not directly consume ATP for muscle contraction.
*I band*
- The **I band** contains only **thin actin filaments** and extends from the edge of the A band to the Z line.
- While actin is crucial for contraction, it does not possess **ATPase activity**; ATP hydrolysis primarily occurs at the **myosin heads** located in the A band.
Fatigue mechanisms US Medical PG Question 9: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
Fatigue mechanisms Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Fatigue mechanisms US Medical PG Question 10: A 38-year-old woman presents to the physician’s clinic with a 6-month history of generalized weakness that usually worsens as the day progresses. She also complains of the drooping of her eyelids and double vision that is worse in the evening. Physical examination reveals bilateral ptosis after a sustained upward gaze and loss of eye convergence which improves upon placing ice packs over the eyes and after the administration of edrophonium. Which of the following is an intrinsic property of the muscle group affected in this patient?
- A. A small mass per motor unit
- B. High ATPase activity (Correct Answer)
- C. High myoglobin content
- D. High density of mitochondria
- E. Increased amount of ATP generated per molecule of glucose
Fatigue mechanisms Explanation: ***High ATPase activity***
- This patient presents with **myasthenia gravis (MG)**, an autoimmune disorder affecting the neuromuscular junction through antibodies against acetylcholine receptors.
- **Extraocular muscles** and other muscles affected early in MG contain a high proportion of **fast-twitch (Type II) muscle fibers**, which are characterized by **high ATPase activity**.
- **Type II fibers** with high ATPase activity generate rapid, powerful contractions but are **more susceptible to neuromuscular junction dysfunction** due to their higher firing rates and greater dependence on efficient neuromuscular transmission.
- This intrinsic property (high ATPase activity) is why these muscles are preferentially affected in myasthenia gravis.
*A small mass per motor unit*
- While extraocular muscles do have **small motor units** (allowing for precise eye movements), this describes the **innervation pattern** rather than an intrinsic biochemical property of the muscle fibers themselves.
- The question specifically asks about an intrinsic property of the muscle group, referring to the metabolic and contractile characteristics of the muscle fibers.
*High myoglobin content*
- **High myoglobin content** is characteristic of **Type I (slow-twitch) oxidative fibers**, which rely on sustained oxygen delivery for prolonged, fatigue-resistant contractions.
- Muscles preferentially affected in MG have a higher proportion of **Type II fibers**, which have lower myoglobin content compared to Type I fibers.
*High density of mitochondria*
- **High mitochondrial density** is characteristic of **Type I (slow-twitch) oxidative fibers** that depend on aerobic metabolism for sustained energy production.
- While extraocular muscles do have oxidative capacity, the **Type II fibers** preferentially affected in MG have relatively lower mitochondrial density compared to Type I fibers and rely more on glycolytic metabolism for rapid energy needs.
*Increased amount of ATP generated per molecule of glucose*
- **Aerobic respiration** in Type I fibers generates approximately 32 ATP molecules per glucose through oxidative phosphorylation.
- **Type II fibers** rely more heavily on **anaerobic glycolysis**, which produces only 2 ATP per glucose molecule, making them less efficient in ATP generation per glucose.
- The muscles affected in MG have higher proportions of Type II fibers with lower ATP efficiency per glucose molecule.
More Fatigue mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.