Exercise testing principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exercise testing principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Exercise testing principles US Medical PG Question 1: A 25-year-old male athlete undergoes a cardiopulmonary exercise test. As exercise intensity increases from rest to moderate levels, which of the following best describes the relationship between oxygen consumption and cardiac output?
- A. Linear increase until anaerobic threshold (Correct Answer)
- B. Exponential increase throughout exercise
- C. Plateau at low exercise intensities
- D. No change until anaerobic threshold
Exercise testing principles Explanation: ***Linear increase until anaerobic threshold***
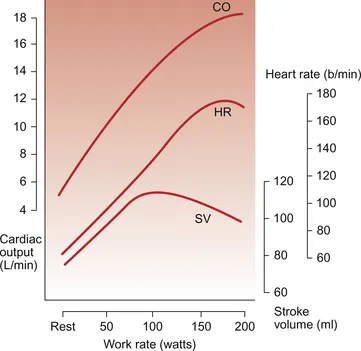
- During incremental exercise, both **oxygen consumption (VO2)** and **cardiac output (CO)** increase proportionally with work rate.
- This **linear relationship** continues until the body reaches the **anaerobic threshold**, beyond which other physiological responses begin to dominate.
*Exponential increase throughout exercise*
- An **exponential increase** would imply a disproportionately rapid rise in oxygen consumption and cardiac output even at low-to-moderate exercise intensities, which is not physiologically accurate.
- While both parameters do increase, the initial increase is typically linear, reflecting the immediate physiological demands.
*Plateau at low exercise intensities*
- A **plateau** would suggest that the body's demand for oxygen and the heart's pumping capacity stabilize despite an increase in exercise intensity, which contradicts the need for increased energy supply during exercise.
- The cardiovascular system actively responds to even low-intensity exercise to meet metabolic demands.
*No change until anaerobic threshold*
- **No change** would mean that the cardiovascular system is not responding to the increased metabolic demands of exercise, which is incorrect.
- Both VO2 and CO begin to rise almost immediately upon starting exercise to meet the muscles' increasing oxygen requirements.
Exercise testing principles US Medical PG Question 2: A 40-year-old female volunteers for an invasive study to measure her cardiac function. She has no previous cardiovascular history and takes no medications. With the test subject at rest, the following data is collected using blood tests, intravascular probes, and a closed rebreathing circuit:
Blood hemoglobin concentration 14 g/dL
Arterial oxygen content 0.22 mL O2/mL
Arterial oxygen saturation 98%
Venous oxygen content 0.17 mL O2/mL
Venous oxygen saturation 78%
Oxygen consumption 250 mL/min
The patient's pulse is 75/min, respiratory rate is 14/ min, and blood pressure is 125/70 mm Hg. What is the cardiac output of this volunteer?
- A. Body surface area is required to calculate cardiac output.
- B. Stroke volume is required to calculate cardiac output.
- C. 250 mL/min
- D. 5.0 L/min (Correct Answer)
- E. 50 L/min
Exercise testing principles Explanation: ***5.0 L/min***
- Cardiac output can be calculated using the **Fick principle**: Cardiac Output $(\text{CO}) = \frac{{\text{Oxygen Consumption}}}{{\text{Arterial } \text{O}_2 \text{ Content} - \text{Venous O}_2 \text{ Content}}}$.
- Given Oxygen Consumption = 250 mL/min, Arterial O$_2$ Content = 0.22 mL/mL, and Venous O$_2$ Content = 0.17 mL/mL. Thus, CO = $\frac{{250 \text{ mL/min}}}{{(0.22 - 0.17) \text{ mL } \text{O}_2/\text{mL blood}}} = \frac{{250 \text{ mL/min}}}{{0.05 \text{ mL } \text{O}_2/\text{mL blood}}} = 5000 \text{ mL/min } = 5.0 \text{ L/min}$.
*Body surface area is required to calculate cardiac output.*
- **Body surface area (BSA)** is used to calculate **cardiac index**, which is cardiac output normalized to body size, but not cardiac output directly.
- While a normal cardiac output might be compared to a patient's BSA for context, it is not a necessary component for calculating the absolute cardiac output.
*Stroke volume is required to calculate cardiac output.*
- Cardiac output can be calculated as **Stroke Volume (SV) x Heart Rate (HR)**. However, stroke volume is not provided directly in this question.
- The Fick principle allows for the calculation of cardiac output **without explicit knowledge of stroke volume** or heart rate, using oxygen consumption and arteriovenous oxygen difference.
*250 mL/min*
- 250 mL/min represents the **oxygen consumption**, not the cardiac output.
- Cardiac output is the volume of blood pumped by the heart per minute, which is influenced by both oxygen consumption and the difference in oxygen content between arterial and venous blood.
*50 L/min*
- A cardiac output of 50 L/min is an **extremely high and physiologically impossible** value for a resting individual.
- This value is 10 times higher than the calculated cardiac output and typically represents a calculation error.
Exercise testing principles US Medical PG Question 3: A woman with coronary artery disease is starting to go for a walk. As she begins, her heart rate accelerates from a resting pulse of 60 bpm until it reaches a rate of 120 bpm, at which point she begins to feel a tightening in her chest. She stops walking to rest and the tightening resolves. This has been happening to her consistently for the last 6 months. Which of the following is a true statement?
- A. This patient's chest pain is indicative of transmural ischemia
- B. Perfusion of the myocardium takes place equally throughout the cardiac cycle
- C. Increasing the heart rate increases the amount of time spent during each cardiac cycle
- D. Increasing the heart rate decreases the relative amount of time spent during diastole (Correct Answer)
- E. Perfusion of the myocardium takes place primarily during systole
Exercise testing principles Explanation: ***Increasing the heart rate decreases the relative amount of time spent during diastole***
- With increasing heart rate, the **duration of the cardiac cycle decreases**, but this reduction is disproportionately greater in **diastole (filling phase)** compared to systole (ejection phase), which becomes critical in patients with coronary artery disease as myocardial perfusion occurs during diastole.
- Reduced diastolic time means less time for **coronary artery filling** and **myocardial perfusion**, exacerbating ischemia in the presence of fixed coronary stenosis.
*This patient's chest pain is indicative of transmural ischemia*
- The patient's symptoms are consistent with **stable angina**, characterized by chest pain with exertion that resolves with rest, suggesting **subendocardial ischemia** rather than transmural.
- **Transmural ischemia** typically indicates a more severe, often prolonged, and extensive reduction in blood flow, such as in a **ST-elevation myocardial infarction (STEMI)**.
*Perfusion of the myocardium takes place equally throughout the cardiac cycle*
- Myocardial perfusion is **not equal throughout the cardiac cycle**; it primarily occurs during **diastole** when the heart muscle is relaxed and coronary arteries are less compressed.
- During **systole**, the contracting myocardium compresses the coronary arteries, restricting blood flow, especially to the **subendocardial layers**.
*Increasing the heart rate increases the amount of time spent during each cardiac cycle*
- **Increasing heart rate** by definition **decreases the total duration of each cardiac cycle** (e.g., if heart rate is 60 bpm, cycle duration is 1 second; if 120 bpm, cycle duration is 0.5 seconds).
- While both systole and diastole shorten, the **diastolic phase shortens more significantly**, which is problematic for myocardial perfusion.
*Perfusion of the myocardium takes place primarily during systole*
- **Myocardial perfusion primarily occurs during diastole**, not systole, because the **intramyocardial pressure is lower** and the coronary arteries are less compressed, allowing for better blood flow.
- During **systole**, the high intramyocardial pressure, especially in the left ventricular wall, compresses the coronary vessels, significantly reducing blood flow to the myocardium.
Exercise testing principles US Medical PG Question 4: A 50-year-old woman comes to the physician for a routine health maintenance examination. She has no personal or family history of serious illness. She smoked one pack of cigarettes daily for 5 years during her 20s. Her pulse is 70/min, and blood pressure is 120/78 mm Hg. Serum lipid studies and glucose concentration are within the reference ranges. Which of the following health maintenance recommendations is most appropriate at this time?
- A. Perform BRCA gene test
- B. Perform abdominal ultrasound
- C. Perform 24-hour ECG
- D. Perform DEXA scan
- E. Perform colonoscopy (Correct Answer)
Exercise testing principles Explanation: ***Perform colonoscopy***
- **Colorectal cancer screening** with colonoscopy is generally recommended for individuals at average risk starting at age **45-50 years**.
- This patient is **50 years old** and has no increased risk factors, making routine colonoscopy the most appropriate screening.
*Perform BRCA gene test*
- **BRCA gene testing** is indicated for individuals with a strong **family history** of breast or ovarian cancer, or those with personal history suggesting a genetic predisposition.
- This patient has **no personal or family history** of serious illness, so BRCA testing is not warranted.
*Perform abdominal ultrasound*
- **Abdominal ultrasound** is typically used to investigate specific symptoms or screen for conditions like **abdominal aortic aneurysm** in high-risk individuals (e.g., male smokers over 65).
- This patient has **no relevant symptoms** or risk factors for which routine abdominal ultrasound screening is recommended.
*Perform 24-hour ECG*
- A **24-hour ECG (Holter monitor)** is used to detect paroxysmal **arrhythmias** or evaluate symptoms like palpitations, syncope, or dizziness.
- This patient is asymptomatic with a normal pulse and blood pressure; therefore, **routine 24-hour ECG** is not indicated.
*Perform DEXA scan*
- A **DEXA scan** is recommended for **osteoporosis screening** in women typically starting at age **65**, or earlier if they have significant risk factors like a history of fragility fractures or certain medical conditions.
- At **50 years old** and with no apparent risk factors for osteoporosis, a DEXA scan is not yet routinely indicated according to general guidelines.
Exercise testing principles US Medical PG Question 5: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
Exercise testing principles Explanation: ***40 mL/beat***
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
Exercise testing principles US Medical PG Question 6: A 43-year-old man comes to the emergency room complaining of chest discomfort. He describes the feeling as "tightness," and also reports weakness and palpitations for the past hour. He denies shortness of breath, diaphoresis, or lightheadedness. He has no significant past medical history, and does not smoke, drink, or use illicit drugs. His father had a myocardial infarction at age 72. He is afebrile, heart rate is 125 bpm, and his blood pressure is 120/76. He is alert and oriented to person, place, and time. His electrocardiogram is shown below. Which of the following tests should be ordered in the initial work-up of this patient's condition?
- A. Chest x-ray
- B. Blood alcohol level
- C. Urine free cortisol level
- D. Urine metanephrines
- E. Thyroid stimulating hormone level (TSH) (Correct Answer)
Exercise testing principles Explanation: ***Thyroid stimulating hormone level (TSH)***
- The patient presents with **palpitations**, **tachycardia (HR 125 bpm)**, and chest tightness, with an ECG showing a **regular narrow-complex tachycardia** consistent with **supraventricular tachycardia (SVT)**.
- **Hyperthyroidism** is a critical secondary cause of SVT and atrial arrhythmias that must be ruled out in the initial workup.
- **TSH testing** is essential to identify **thyroid dysfunction** as a reversible and treatable cause of the tachyarrhythmia.
- Treating the underlying hyperthyroidism can resolve the arrhythmia and prevent recurrence.
*Incorrect: Urine metanephrines*
- While **pheochromocytoma** can cause palpitations and tachycardia, it typically presents with **paroxysmal hypertension**, **headaches**, and **diaphoresis** (the classic triad).
- This patient has **normal blood pressure** and denies diaphoresis, making pheochromocytoma less likely.
- TSH is a more appropriate first-line test given the clinical presentation.
*Incorrect: Chest x-ray*
- A chest X-ray may help evaluate for **structural cardiac or pulmonary abnormalities**, but it does not identify the **underlying cause** of SVT.
- It is not specific for diagnosing **metabolic or endocrine triggers** of tachyarrhythmias.
*Incorrect: Blood alcohol level*
- The patient **denies alcohol use**, making this test unnecessary in the initial evaluation.
- Alcohol withdrawal can cause tachycardia, but there is no clinical history suggesting this.
*Incorrect: Urine free cortisol level*
- **Cushing's syndrome** does not typically present with acute palpitations or SVT as the primary manifestation.
- This test is not relevant to the immediate evaluation of **tachyarrhythmia**.
Exercise testing principles US Medical PG Question 7: A study is conducted to find an association between serum cholesterol and ischemic heart disease. Data is collected, and patients are classified into either the "high cholesterol" or "normal cholesterol" group and also into groups whether or not the patient experiences stable angina. Which type of data analysis is most appropriate for this study?
- A. Attributable risk
- B. Analysis of variance
- C. Chi-squared (Correct Answer)
- D. T-test
- E. Pearson correlation
Exercise testing principles Explanation: ***Chi-squared***
- The **chi-squared test** is ideal for analyzing two **categorical variables**, such as cholesterol levels (high/normal) and the presence of stable angina (yes/no), to see if there's an association between them.
- It assesses whether the observed frequencies in each category differ significantly from the expected frequencies, under the assumption of no association.
*Attributable risk*
- **Attributable risk** quantifies the proportion of disease in an exposed group that is directly due to the exposure.
- While it might be calculated *after* establishing an association (e.g., using a chi-squared test), it's a measure of actual impact rather than a method for *finding the association* between two categorical variables.
*Analysis of variance*
- **Analysis of variance (ANOVA)** is used to compare the means of **three or more groups** for a continuous outcome variable.
- It works when you have a categorical independent variable with multiple levels and a continuous dependent variable, which is not the case here as both variables are categorical.
*T-test*
- A **t-test** is used to compare the means of **two groups** for a continuous outcome variable.
- It is not appropriate for analyzing the association between two categorical variables like cholesterol categories and angina presence.
*Pearson correlation*
- **Pearson correlation** measures the linear relationship between **two continuous variables**.
- It is unsuitable for this study as both cholesterol status and angina presence are categorical variables, not continuous.
Exercise testing principles US Medical PG Question 8: A 58-year-old woman comes to the physician because of a 3-month history of recurring chest discomfort. The symptoms occur when walking up the stairs to her apartment or when walking quickly for 5 minutes on level terrain. She has not had shortness of breath, palpitations, or dizziness. She has hypertension and hyperlipidemia. Current medications include estrogen replacement therapy, metoprolol, amlodipine, lisinopril, hydrochlorothiazide, and rosuvastatin. She drinks 3–4 cups of coffee per day. She does not drink alcohol. Her pulse is 65/min, respirations are 21/min, and blood pressure is 145/90 mm Hg. Physical examination shows no abnormalities. A resting ECG shows normal sinus rhythm. She is scheduled for a cardiac exercise stress test in 2 days. Discontinuation of which of the following is the most appropriate next step in management at this time?
- A. Metoprolol and amlodipine (Correct Answer)
- B. Lisinopril and hydrochlorothiazide
- C. Estrogen and hydrochlorothiazide
- D. Estrogen and amlodipine
- E. Metoprolol and rosuvastatin
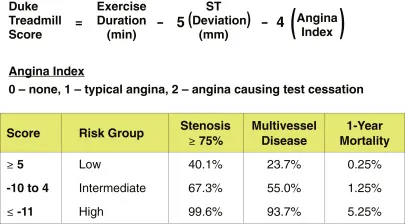
Exercise testing principles Explanation: ***Metoprolol and amlodipine***
- **Beta-blockers** (metoprolol) and **calcium channel blockers** (amlodipine) used to treat angina can mask ischemia during a stress test, leading to a falsely negative result.
- Temporarily discontinuing these medications allows for a more accurate assessment of the heart's response to stress and diagnosis of **ischemic heart disease**.
*Lisinopril and hydrochlorothiazide*
- **ACE inhibitors** (lisinopril) and **diuretics** (hydrochlorothiazide) primarily manage blood pressure and do not significantly interfere with the diagnostic capabilities of a cardiac exercise stress test for detecting ischemia.
- While they can lower blood pressure, their impact on the heart's ischemic response during stress is less direct and less problematic than that of beta-blockers or calcium channel blockers.
*Estrogen and hydrochlorothiazide*
- **Estrogen replacement therapy** generally does not interfere with the results or interpretation of an exercise stress test for ischemia.
- **Hydrochlorothiazide** is a diuretic primarily affecting blood pressure and fluid balance; it does not significantly alter cardiac physiology in a way that would obscure ischemic findings during stress.
*Estrogen and amlodipine*
- While **amlodipine** (a calcium channel blocker) needs to be held before a stress test, **estrogen replacement therapy** does not affect the diagnostic accuracy of the test.
- Combining these two would be partially correct regarding amlodipine but introduces an unnecessary and incorrect action regarding estrogen.
*Metoprolol and rosuvastatin*
- **Metoprolol** (a beta-blocker) should be discontinued as it can mask ischemia during a stress test.
- However, **rosuvastatin** (a statin) is crucial for managing hyperlipidemia and preventing cardiovascular events; there is no medical reason to discontinue it before a stress test, as it does not interfere with the test's diagnostic accuracy.
Exercise testing principles US Medical PG Question 9: An 18-year-old boy is brought to the emergency department by his parents because he suddenly collapsed while playing football. His parents mention that he had complained of dizziness while playing before, but never fainted in the middle of a game. On physical examination, the blood pressure is 130/90 mm Hg, the respirations are 15/min, and the pulse is 110/min. The chest is clear, but a systolic ejection murmur is present. The remainder of the examination revealed no significant findings. An electrocardiogram is ordered, along with an echocardiogram. He is diagnosed with hypertrophic cardiomyopathy and the physician lists all the precautions he must follow. Which of the following drugs will be on the list of contraindicated substances?
- A. Βeta-blockers
- B. Dobutamine
- C. Nitrates (Correct Answer)
- D. Calcium channel blockers
- E. Potassium channel blockers
Exercise testing principles Explanation: ***Nitrates***
- **Nitrates** cause **vasodilation**, which decreases **preload** and worsens **left ventricular outflow tract obstruction (LVOTO)** in **hypertrophic cardiomyopathy (HCM)**, potentially leading to syncope or sudden death.
- Reduced preload exacerbates the dynamic obstruction, causing a critical drop in cardiac output.
- **Commonly encountered substances** patients must avoid include nitroglycerin, isosorbide, and **phosphodiesterase-5 inhibitors** (sildenafil, tadalafil) which potentiate nitrate effects.
- This is a critical counseling point for HCM patients in everyday life.
*Beta-blockers*
- **Beta-blockers** are **first-line treatment** for **hypertrophic cardiomyopathy (HCM)** as they reduce heart rate, improve diastolic filling, and decrease contractility, thereby reducing **LVOTO**.
- They alleviate symptoms and reduce the risk of sudden cardiac death in HCM.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** that increases contractility and heart rate, which would worsen **LVOTO** in HCM.
- While also contraindicated in HCM, dobutamine is only used in **controlled hospital settings** for stress testing or hemodynamic support, not a substance patients encounter in daily life.
- The question focuses on outpatient counseling about substances to avoid in everyday situations.
*Calcium channel blockers*
- **Non-dihydropyridine calcium channel blockers** (verapamil, diltiazem) are used in **HCM management**, particularly in patients who cannot tolerate beta-blockers.
- They improve **diastolic function** and reduce **LVOTO** by decreasing contractility and heart rate.
- **Caution:** Dihydropyridines (nifedipine, amlodipine) can worsen obstruction and should be avoided.
*Potassium channel blockers*
- **Antiarrhythmics** like **amiodarone** (potassium channel blocker) are used in **HCM** patients for atrial or ventricular arrhythmias.
- Not contraindicated; therapeutically indicated for rhythm management.
Exercise testing principles US Medical PG Question 10: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Exercise testing principles Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
More Exercise testing principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.