Exercise in special populations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exercise in special populations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Exercise in special populations US Medical PG Question 1: A 22-year-old woman with type 1 diabetes mellitus and mild asthma comes to the physician for a follow-up examination. She has had several episodes of sweating, dizziness, and nausea in the past 2 months that occur during the day and always resolve after she drinks orange juice. She is compliant with her diet and insulin regimen. The physician recommends lowering her insulin dose in certain situations. This recommendation is most important in which of the following situations?
- A. After a stressful exam
- B. During a viral infection
- C. Before exercise (Correct Answer)
- D. After large meals
- E. During pregnancy
Exercise in special populations Explanation: ***Before exercise***
- Exercise increases **glucose utilization** by muscles, which can lead to **hypoglycemia** in individuals taking insulin if the dose isn't adjusted.
- The patient's symptoms (sweating, dizziness, nausea) are classic for **hypoglycemia**, which resolves with sugar intake (orange juice).
*After a stressful exam*
- **Stress** typically elevates **counter-regulatory hormones** (e.g., cortisol, epinephrine), which can increase blood glucose levels rather than cause hypoglycemia.
- An insulin dose reduction is usually not necessary and could lead to **hyperglycemia** in this situation.
*During a viral infection*
- Infections, even viral ones, often trigger the release of **stress hormones**, increasing glucose production and leading to **hyperglycemia** and increased insulin requirements.
- Insulin doses usually need to be *increased*, not decreased, during illness to manage elevated blood sugar.
*After large meals*
- Large meals, especially those rich in carbohydrates, would necessitate an **increased or consistent insulin dose** to cover the glucose intake and prevent **postprandial hyperglycemia**.
- Reducing insulin after a large meal would likely lead to uncontrolled high blood sugar rather than prevent hypoglycemia.
*During pregnancy*
- While insulin requirements can fluctuate throughout pregnancy, they generally **increase** in the second and third trimesters due to increased **insulin resistance**.
- Reducing insulin during pregnancy without careful monitoring could lead to uncontrolled **hyperglycemia**, posing risks to both mother and fetus.
Exercise in special populations US Medical PG Question 2: A 42-year-old G1P0 woman presents to an obstetrician for her first prenatal visit. She has been pregnant for about 10 weeks and is concerned about how pregnancy will affect her health. Specifically, she is afraid that her complicated medical history will be adversely affected by her pregnancy. Her past medical history is significant for mild polycythemia, obesity hypoventilation syndrome, easy bleeding, multiple sclerosis, and aortic regurgitation. Which of these disorders is most likely to increase in severity during the course of the pregnancy?
- A. Easy bleeding
- B. Hypoventilation (Correct Answer)
- C. Multiple sclerosis
- D. Polycythemia
- E. Heart murmur
Exercise in special populations Explanation: ***Hypoventilation***
- Pregnancy leads to increased **oxygen consumption** and **carbon dioxide production**, requiring increased ventilation.
- In a patient with **obesity hypoventilation syndrome**, the already compromised respiratory drive and mechanics can worsen, leading to increased **hypercapnia** and **hypoxia**.
*Easy bleeding*
- Pregnancy is a **hypercoagulable state**, which typically reduces the risk of bleeding.
- While certain pregnancy complications (e.g., placental abruption) can cause bleeding, the overall physiological changes tend to **decrease primary bleeding tendencies**.
*Multiple sclerosis*
- Pregnancy typically has an **immunomodulatory effect** that can lead to a decrease in the frequency of MS relapses, especially in the third trimester.
- Relapses may increase postpartum, but during pregnancy itself, the condition often **stabilizes or improves**.
*Polycythemia*
- Pregnancy increases **plasma volume** significantly, which can lead to a relative **hemodilution**.
- This physiological change would likely **ameliorate mild polycythemia** rather than worsen it.
*Heart murmur*
- The murmur is due to **aortic regurgitation**, and while pregnancy increases **cardiac output** and **blood volume**, severe aortic regurgitation can worsen.
- However, the overall physiological changes of pregnancy result in **increased minute ventilation**, making hypoventilation a more direct and universally worsened problem with existing **obesity hypoventilation syndrome**.
Exercise in special populations US Medical PG Question 3: During exercise, what is the primary mechanism for increased oxygen delivery to active muscles?
- A. Decreased blood viscosity
- B. Increased cardiac output (Correct Answer)
- C. Increased hemoglobin affinity
- D. Enhanced oxygen diffusion
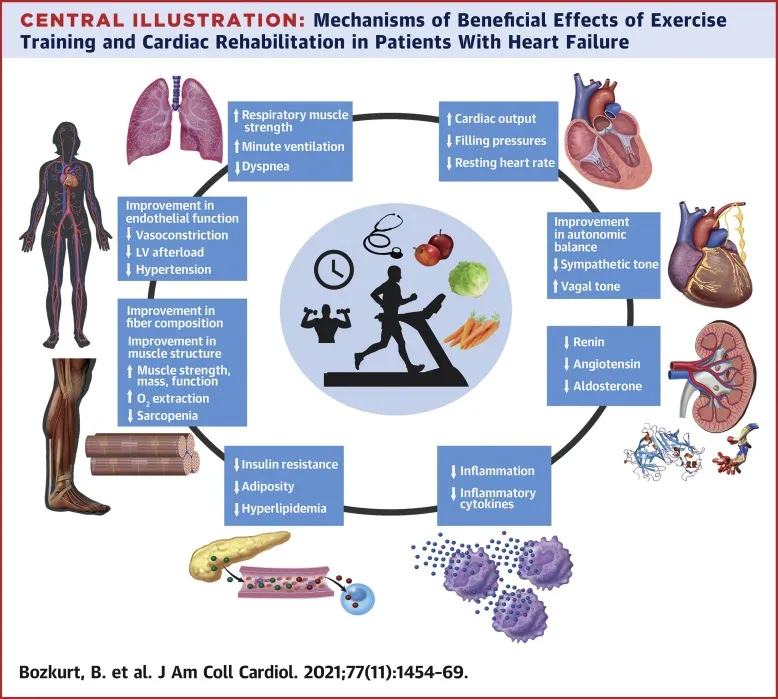
Exercise in special populations Explanation: ***Increased cardiac output***
- During exercise, **cardiac output** increases significantly due to both an elevated **heart rate** and increased **stroke volume**, directly pushing more oxygenated blood to the active muscles.
- This augmentation in blood flow is the primary factor ensuring a sufficient supply of oxygen and nutrients to meet the heightened metabolic demands of exercising muscles.
*Decreased blood viscosity*
- While factors like **hemodilution** can decrease blood viscosity during prolonged exercise, this effect is relatively minor and not the primary mechanism for acute increases in oxygen delivery compared to the dramatic increase in cardiac output.
- A decrease in blood viscosity can slightly improve flow efficiency, but it doesn't fundamentally change the amount of blood pumped per minute to the muscles.
*Increased hemoglobin affinity*
- An *increased* hemoglobin affinity for oxygen would actually make it *harder* for oxygen to unload from hemoglobin to the tissues, which is counterproductive for oxygen delivery during exercise.
- In fact, during exercise, local conditions like increased temperature, decreased pH (**Bohr effect**), and increased 2,3-BPG tend to *decrease* hemoglobin's affinity for oxygen, facilitating oxygen release to active muscles.
*Enhanced oxygen diffusion*
- While exercise does improve the efficiency of oxygen extraction at the tissue level due to a steeper partial pressure gradient and increased capillary recruitment, the *rate* of oxygen diffusion across the capillary membrane isn't the primary modulator of overall oxygen delivery.
- The main determinant is the *amount* of oxygenated blood reaching the muscle, which is governed by cardiac output and local blood flow regulation.
Exercise in special populations US Medical PG Question 4: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Exercise in special populations Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Exercise in special populations US Medical PG Question 5: A 56-year-old woman comes to the physician for follow-up after a measurement of elevated blood pressure at her last visit three months ago. She works as a high school teacher at a local school. She says that she mostly eats cafeteria food and take-out. She denies any regular physical activity. She does not smoke or use any recreational drugs. She drinks 2 to 3 glasses of wine per day. She has hypercholesterolemia for which she takes atorvastatin. Her height is 165 cm (5 ft 5 in), weight is 82 kg (181 lb), and BMI is 30.1 kg/m2. Her pulse is 67/min, respirations are 18/min, and blood pressure is 152/87 mm Hg on the right arm and 155/92 mm Hg on the left arm. She would like to try lifestyle modifications to improve her blood pressure before considering pharmacologic therapy. Which of the following lifestyle modifications is most likely to result in the greatest reduction of this patient's systolic blood pressure?
- A. Walking for 30 minutes, 5 days per week
- B. Reducing sodium intake to less than 2.4 g per day
- C. Losing 15 kg (33 lb) of body weight (Correct Answer)
- D. Adopting a DASH diet
- E. Decreasing alcohol consumption to maximum of one drink per day
Exercise in special populations Explanation: ***Losing 15 kg (33 lb) of body weight***
- **Weight reduction** is the most effective lifestyle modification for lowering blood pressure, correlating directly with the amount of weight lost.
- A loss of 15 kg (33 lb) in this patient, who is **obese (BMI 30.1)**, could significantly reduce her systolic blood pressure, potentially by 5-20 mmHg per 10 kg weight loss.
*Walking for 30 minutes, 5 days per week*
- Regular **aerobic physical activity** is beneficial for blood pressure reduction, typically resulting in a 4-9 mmHg decrease in systolic pressure.
- While helpful, the magnitude of reduction from exercise alone is generally less than that achieved with significant weight loss in an obese individual.
*Reducing sodium intake to less than 2.4 g per day*
- **Sodium restriction** is an effective strategy, often leading to a 2-8 mmHg reduction in systolic blood pressure.
- Given the patient's diet of cafeteria and take-out food, high sodium intake is likely, making this a relevant intervention, but typically less impactful than substantial weight loss.
*Adopting a DASH diet*
- The **Dietary Approaches to Stop Hypertension (DASH) diet** emphasizes fruits, vegetables, and low-fat dairy, and can significantly lower blood pressure, by 8-14 mmHg.
- This diet is highly effective, but for an obese individual, the blood pressure reduction from achieving a healthy weight is often greater.
*Decreasing alcohol consumption to maximum of one drink per day*
- Reducing **excessive alcohol intake** can decrease systolic blood pressure by 2-4 mmHg, as the patient reports 2-3 glasses of wine daily.
- While beneficial, this reduction is likely to be less substantial compared to major weight loss or other dietary changes.
Exercise in special populations US Medical PG Question 6: A 65-year-old man presents to the emergency department with shortness of breath. He was at home cleaning his yard when his symptoms began. The patient is a farmer and does not have regular medical care. He has smoked two packs of cigarettes every day for the past 40 years. The patient lives alone and admits to feeling lonely at times. His temperature is 99.5°F (37.5°C), blood pressure is 159/95 mmHg, pulse is 90/min, respirations are 19/min, and oxygen saturation is 86% on room air. On physical exam, you note a man in distress. Pulmonary exam reveals poor air movement, wheezing, and bibasilar crackles. Cardiac exam is notable for an S4 heart sound. The patient is started on appropriate therapy and his symptoms improve. Prior to discharge he is no longer distressed when breathing and his oxygen saturation is 90% on room air. Which of the following interventions could improve mortality the most in this patient?
- A. Varenicline (Correct Answer)
- B. Albuterol
- C. Ipratropium
- D. Home oxygen
- E. Magnesium
Exercise in special populations Explanation: ***Varenicline***
- This patient presents with symptoms highly suggestive of an **acute exacerbation of COPD** (shortness of breath, poor air movement, wheezing, significant smoking history). **Smoking cessation** is the single most effective intervention to improve mortality in patients with COPD, and varenicline is a highly effective medication for this purpose.
- While other interventions manage acute symptoms, quitting smoking addresses the underlying progressive lung damage and **reduces the risk of future exacerbations and overall mortality**.
*Albuterol*
- **Albuterol** is a **short-acting beta-agonist (SABA)** used as a rescue inhaler to provide rapid bronchodilation during an acute exacerbation of COPD.
- While essential for **symptomatic relief** and managing acute episodes, it does not impact the long-term progression of COPD or overall mortality.
*Ipratropium*
- **Ipratropium** is a **short-acting muscarinic antagonist (SAMA)** that also causes bronchodilation and is used in the acute management of COPD exacerbations, often in combination with SABAs.
- Like albuterol, it provides **symptomatic relief** but does not alter the disease course or improve long-term mortality.
*Home oxygen*
- **Home oxygen therapy** is indicated for patients with severe, chronic hypoxemia (PaO2 < 55 mmHg or SaO2 < 88%) on room air to improve quality of life and decrease mortality.
- While beneficial for select patients with **chronic hypoxemia**, it is not a primary intervention for acute exacerbations or a more impactful mortality-reducing strategy than smoking cessation for a patient who continues to smoke.
*Magnesium*
- **Intravenous magnesium sulfate** can be considered in severe, life-threatening asthma exacerbations or acute COPD exacerbations that are unresponsive to standard bronchodilator therapy.
- It works by inducing **bronchial smooth muscle relaxation** but is a therapy for acute rather than chronic management or mortality improvement.
Exercise in special populations US Medical PG Question 7: A 56-year-old woman visits her family physician accompanied by her son. She has recently immigrated to Canada and does not speak English. Her son tells the physician that he is worried that his mother gets a lot of sugar in her diet and does not often monitor her glucose levels. Her previous lab work shows a HbA1c value of 8.7%. On examination, her blood pressure is 130/87 mm Hg and weight is 102 kg (224.9 lb). Which of the following is the correct location of where the glucose transport is most likely affected in this patient?
- A. Skeletal muscle (Correct Answer)
- B. Red blood cells
- C. Pancreas
- D. Brain
- E. Liver
Exercise in special populations Explanation: ***Skeletal muscle***
- This patient presents with an HbA1c of 8.7% and obesity, indicative of **Type 2 Diabetes Mellitus**, where **insulin resistance** is a key feature.
- **Skeletal muscle** is a primary site of **glucose uptake** stimulated by insulin and is therefore most significantly affected by insulin resistance.
*Red blood cells*
- **Red blood cells** take up glucose via **insulin-independent** GLUT1 transporters.
- Their glucose transport is generally **not affected** in Type 2 Diabetes, although high glucose levels can lead to glycation of hemoglobin (HbA1c).
*Pancreas*
- The **pancreas** (specifically beta cells) produces insulin, and in Type 2 Diabetes, there can be a **progressive decline in beta cell function** over time.
- However, the initial and primary defect in glucose utilization is **insulin resistance** in peripheral tissues, not impaired glucose transport into pancreatic cells for metabolic regulation.
*Brain*
- The **brain** primarily utilizes glucose for energy via **insulin-independent** GLUT1 and GLUT3 transporters at the blood-brain barrier and neurons, respectively.
- Glucose uptake into the brain is generally **preserved** in Type 2 Diabetes, even in severe insulin resistance.
*Liver*
- The **liver** is involved in both glucose production (gluconeogenesis, glycogenolysis) and uptake (glycogenesis). In Type 2 Diabetes, the liver exhibits **increased glucose output** due to insulin resistance and impaired suppression of endogenous glucose production.
- While **hepatic insulin resistance** is present, the question asks about the primary site where **glucose transport is most likely affected**, and skeletal muscle's role in glucose disposal makes it a more direct answer for impaired glucose transport.
Exercise in special populations US Medical PG Question 8: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Exercise in special populations Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Exercise in special populations US Medical PG Question 9: A person is exercising strenuously on a treadmill for 1 hour. An arterial blood gas measurement is then taken. Which of the following are the most likely values?
- A. pH 7.56, PaO2 100, PCO2 44, HCO3 38
- B. pH 7.32, PaO2 42, PCO2 50, HCO3 27
- C. pH 7.57 PaO2 100, PCO2 23, HCO3 21 (Correct Answer)
- D. pH 7.38, PaO2 100, PCO2 69 HCO3 42
- E. pH 7.36, PaO2 100, PCO2 40, HCO3 23
Exercise in special populations Explanation: ***pH 7.57, PaO2 100, PCO2 23, HCO3 21***
- After 1 hour of strenuous exercise, this represents **respiratory alkalosis with mild metabolic compensation**, which is the expected finding in a healthy individual during sustained vigorous exercise.
- The **low PCO2 (23 mmHg)** reflects appropriate **hyperventilation** in response to increased metabolic demands and lactic acid production. During intense exercise, minute ventilation increases dramatically, often exceeding the rate of CO2 production.
- The **slightly elevated pH (7.57)** and **mildly decreased HCO3 (21 mEq/L)** indicate that respiratory compensation has slightly overshot, creating mild alkalosis, while the bicarbonate is consumed both in buffering lactate and through renal compensation.
- **Normal PaO2 (100 mmHg)** confirms adequate oxygenation maintained by increased ventilation.
*pH 7.36, PaO2 100, PCO2 40, HCO3 23*
- These are **completely normal arterial blood gas values** with no evidence of any physiological stress or compensation.
- After 1 hour of strenuous exercise, we would expect **hyperventilation with decreased PCO2**, not a normal PCO2 of 40 mmHg. This profile would be consistent with rest, not vigorous exercise.
- The absence of any respiratory or metabolic changes makes this inconsistent with the clinical scenario.
*pH 7.56, PaO2 100, PCO2 44, HCO3 38*
- This profile suggests **metabolic alkalosis** (high pH, high HCO3) with inadequate respiratory compensation (normal to slightly elevated PCO2).
- This is **not consistent with strenuous exercise**, which produces metabolic acid (lactate), not metabolic base. The elevated HCO3 suggests vomiting, diuretic use, or other causes of metabolic alkalosis.
*pH 7.32, PaO2 42, PCO2 50, HCO3 27*
- This indicates **respiratory acidosis** (low pH, high PCO2) with **severe hypoxemia** (PaO2 42 mmHg).
- During strenuous exercise, healthy individuals **increase ventilation** to enhance O2 delivery and remove CO2, so both hypoxemia and hypercapnia are unexpected and would suggest severe cardiopulmonary disease or hypoventilation.
*pH 7.38, PaO2 100, PCO2 69, HCO3 42*
- This demonstrates **compensated respiratory acidosis** (normal pH, markedly elevated PCO2 and HCO3).
- The **very high PCO2 (69 mmHg)** indicates severe **hypoventilation**, which is the opposite of what occurs during exercise. This profile suggests chronic respiratory failure with metabolic compensation, such as in severe COPD.
Exercise in special populations US Medical PG Question 10: A 19-year-old male soccer player undergoes an exercise tolerance test to measure his maximal oxygen uptake during exercise. Which of the following changes are most likely to occur during exercise?
- A. Increased apical ventilation-perfusion ratio
- B. Decreased physiologic dead space (Correct Answer)
- C. Decreased alveolar-arterial oxygen gradient
- D. Increased arterial partial pressure of oxygen
- E. Increased pulmonary vascular resistance
Exercise in special populations Explanation: **Decreased physiologic dead space**
- During exercise, there is improved perfusion to previously underperfused areas of the lung, leading to a **more uniform ventilation-perfusion (V/Q) matching** and thus a decrease in physiologic dead space.
- The increased cardiac output helps to perfuse more capillaries, reducing the amount of ventilated air that does not participate in gas exchange.
*Increased apical ventilation-perfusion ratio*
- At rest, the **apical V/Q ratio is already high** due to gravity-dependent differences in blood flow; exercise partially normalizes these differences.
- While overall V/Q matching improves, the relative V/Q differences between apical and basal regions may become less pronounced, not necessarily a further increase in the apical ratio.
*Decreased alveolar-arterial oxygen gradient*
- During severe exercise, the **A-a gradient often increases slightly** due to increased oxygen diffusion limitations and V/Q mismatch.
- Although overall gas exchange efficiency improves, the sheer volume of oxygen demand can reveal small imbalances, rather than fully eliminating the gradient.
*Increased arterial partial pressure of oxygen*
- Exercise typically leads to **stable or slightly decreased arterial PO2** in healthy individuals due to the increased metabolic demand and potential small V/Q mismatches.
- The body maintains arterial PO2 remarkably well even at high exertion, but it does not usually significantly increase.
*Increased pulmonary vascular resistance*
- During exercise, **pulmonary vascular resistance (PVR) generally decreases** due to recruitment and distension of pulmonary capillaries.
- This decrease in PVR helps to accommodate the increased cardiac output without a significant rise in pulmonary arterial pressure.
More Exercise in special populations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.