Cardiovascular responses to exercise US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiovascular responses to exercise. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiovascular responses to exercise US Medical PG Question 1: A woman with coronary artery disease is starting to go for a walk. As she begins, her heart rate accelerates from a resting pulse of 60 bpm until it reaches a rate of 120 bpm, at which point she begins to feel a tightening in her chest. She stops walking to rest and the tightening resolves. This has been happening to her consistently for the last 6 months. Which of the following is a true statement?
- A. This patient's chest pain is indicative of transmural ischemia
- B. Perfusion of the myocardium takes place equally throughout the cardiac cycle
- C. Increasing the heart rate increases the amount of time spent during each cardiac cycle
- D. Increasing the heart rate decreases the relative amount of time spent during diastole (Correct Answer)
- E. Perfusion of the myocardium takes place primarily during systole
Cardiovascular responses to exercise Explanation: ***Increasing the heart rate decreases the relative amount of time spent during diastole***
- With increasing heart rate, the **duration of the cardiac cycle decreases**, but this reduction is disproportionately greater in **diastole (filling phase)** compared to systole (ejection phase), which becomes critical in patients with coronary artery disease as myocardial perfusion occurs during diastole.
- Reduced diastolic time means less time for **coronary artery filling** and **myocardial perfusion**, exacerbating ischemia in the presence of fixed coronary stenosis.
*This patient's chest pain is indicative of transmural ischemia*
- The patient's symptoms are consistent with **stable angina**, characterized by chest pain with exertion that resolves with rest, suggesting **subendocardial ischemia** rather than transmural.
- **Transmural ischemia** typically indicates a more severe, often prolonged, and extensive reduction in blood flow, such as in a **ST-elevation myocardial infarction (STEMI)**.
*Perfusion of the myocardium takes place equally throughout the cardiac cycle*
- Myocardial perfusion is **not equal throughout the cardiac cycle**; it primarily occurs during **diastole** when the heart muscle is relaxed and coronary arteries are less compressed.
- During **systole**, the contracting myocardium compresses the coronary arteries, restricting blood flow, especially to the **subendocardial layers**.
*Increasing the heart rate increases the amount of time spent during each cardiac cycle*
- **Increasing heart rate** by definition **decreases the total duration of each cardiac cycle** (e.g., if heart rate is 60 bpm, cycle duration is 1 second; if 120 bpm, cycle duration is 0.5 seconds).
- While both systole and diastole shorten, the **diastolic phase shortens more significantly**, which is problematic for myocardial perfusion.
*Perfusion of the myocardium takes place primarily during systole*
- **Myocardial perfusion primarily occurs during diastole**, not systole, because the **intramyocardial pressure is lower** and the coronary arteries are less compressed, allowing for better blood flow.
- During **systole**, the high intramyocardial pressure, especially in the left ventricular wall, compresses the coronary vessels, significantly reducing blood flow to the myocardium.
Cardiovascular responses to exercise US Medical PG Question 2: A 17-year-old previously healthy, athletic male suddenly falls unconscious while playing soccer. His athletic trainer comes to his aid and notes that he is pulseless. He begins performing CPR on the patient until the ambulance arrives but the teenager is pronounced dead when the paramedics arrived. Upon investigation of his primary care physician's office notes, it was found that the child had a recognized murmur that was ruled to be "benign." Which of the following conditions would have increased the intensity of the murmur?
- A. Inspiration
- B. Placing the patient in a squatting position
- C. Valsalva (Correct Answer)
- D. Passive leg raise
- E. Handgrip
Cardiovascular responses to exercise Explanation: ***Valsalva***
- The patient's sudden death after collapsing during soccer, coupled with a previously noted "benign" murmur, strongly suggests **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a common cause of sudden cardiac death in young athletes. The **Valsalva maneuver** decreases preload and left ventricular volume, thereby **increasing the left ventricular outflow tract (LVOT) obstruction** and hence the intensity of the HOCM murmur.
- This maneuver reduces venous return to the heart, leading to reduced ventricular filling and decreased stroke volume. This exacerbates the obstruction in HOCM, making the murmur louder.
*Inspiration*
- **Inspiration** typically **increases venous return to the right side of the heart**, which would generally intensify right-sided murmurs (e.g., tricuspid regurgitation).
- It would have **minimal effect or slightly decrease** the intensity of a left-sided obstructive murmur like that in HOCM, as it does not directly increase the LVOT obstruction.
*Placing the patient in a squatting position*
- Squatting increases both **preload** and **afterload** by increasing systemic vascular resistance and venous return.
- This increase in ventricular volume would **reduce the outflow tract obstruction** in HOCM, thereby **decreasing the intensity of the murmur**.
*Passive leg raise*
- A **passive leg raise** increases **venous return** and thus **preload**, leading to increased ventricular filling.
- Similar to squatting, this increased left ventricular volume would **reduce the left ventricular outflow tract obstruction** associated with HOCM, thereby **decreasing the murmur's intensity**.
*Handgrip*
- The **handgrip maneuver** primarily **increases afterload** and, to some extent, preload by increasing systemic vascular resistance.
- While it can increase the intensity of murmurs like mitral regurgitation and ventricular septal defect, it would generally **decrease or have no significant effect** on the murmur of HOCM due to the increased ventricular volume reducing the outflow obstruction.
Cardiovascular responses to exercise US Medical PG Question 3: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
Cardiovascular responses to exercise Explanation: ***40 mL/beat***
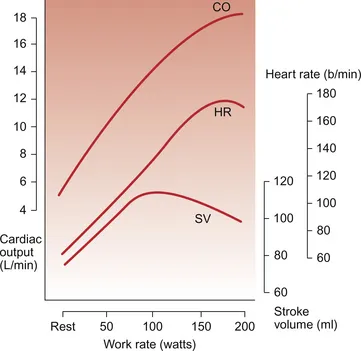
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
Cardiovascular responses to exercise US Medical PG Question 4: During a clinical study evaluating the effects of exercise on muscle perfusion, 15 healthy individuals perform a 20-minute treadmill run at submaximal effort. Before and after the treadmill session, perfusion of the quadriceps muscle is evaluated with contrast-enhanced magnetic resonance imaging. The study shows a significant increase in muscle blood flow per unit of tissue mass. Which of the following local changes is most likely involved in the observed change in perfusion?
- A. Increase in adenosine (Correct Answer)
- B. Decrease in potassium
- C. Increase in thromboxane A2
- D. Increase in endothelin
- E. Decrease in prostacyclin
Cardiovascular responses to exercise Explanation: ***Increase in adenosine***
- **Adenosine** is a potent **vasodilator** released by metabolically active tissues, particularly in response to increased oxygen demand and ATP hydrolysis during exercise.
- Its accumulation leads to relaxation of vascular smooth muscle, increasing blood flow to meet the muscles' elevated metabolic needs.
*Decrease in potassium*
- An increase in **extracellular potassium** (not a decrease) generally causes vasodilation in skeletal muscle by hyperpolarizing smooth muscle cells.
- A decrease in potassium outside the cell would not be expected to cause vasodilation and increased perfusion during exercise.
*Increase in thromboxane A2*
- **Thromboxane A2** is primarily a **vasoconstrictor** and platelet aggregator, mainly involved in hemostasis and inflammation.
- Increased levels would lead to reduced blood flow, not the observed increase in perfusion during exercise.
*Increase in endothelin*
- **Endothelin** is one of the most potent **vasoconstrictors** known, primarily released from endothelial cells.
- An increase in endothelin would severely constrict blood vessels and decrease muscle perfusion, counteracting the effects of exercise.
*Decrease in prostacyclin*
- **Prostacyclin (PGI2)** is a potent **vasodilator** and inhibitor of platelet aggregation.
- A decrease in prostacyclin would lead to vasoconstriction and reduced blood flow, which is contrary to the increased perfusion seen during exercise.
Cardiovascular responses to exercise US Medical PG Question 5: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Cardiovascular responses to exercise Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Cardiovascular responses to exercise US Medical PG Question 6: In the coronary steal phenomenon, vessel dilation is paradoxically harmful because blood is diverted from ischemic areas of the myocardium. Which of the following is responsible for the coronary steal phenomenon?
- A. Venodilation
- B. Microvessel dilation (Correct Answer)
- C. Dilation of the large coronary arteries
- D. Systemic arterial dilation
- E. Volume loss of fluid in the periphery
Cardiovascular responses to exercise Explanation: ***Microvessel dilation***
- The coronary steal phenomenon occurs when **vasodilators** are administered, causing dilation of **healthy coronary microvessels** and a decrease in resistance.
- This preferentially diverts blood flow away from already **ischemic areas** with maximally dilated intrinsic microvessels, worsening myocardial ischemia.
*Venodilation*
- **Venodilation** primarily reduces **preload** by increasing venous capacitance, not by directly altering coronary microcirculatory blood flow distribution in a way that causes "steal."
- While some vasodilators have venodilatory effects, this specific effect is not the mechanism behind coronary steal.
*Dilation of the large coronary arteries*
- Dilation of large coronary arteries alone doesn't cause the "steal" but rather improves overall blood flow. The critical issue is the differential response of **collateral** and **non-collateral microvessels**.
- **Stenoses** in large coronary arteries are the underlying pathology, but the steal phenomenon itself results from changes in **downstream microvascular resistance**.
*Systemic arterial dilation*
- **Systemic arterial dilation** primarily reduces afterload and can lower blood pressure, but it does not specifically explain the redistribution of coronary blood flow to the detriment of ischemic zones within the myocardium.
- The key to coronary steal is the **heterogeneity of response** at the microvascular level within the coronary circulation.
*Volume loss of fluid in the periphery*
- **Volume loss** in the periphery would influence overall circulatory dynamics and cardiac output but is not directly responsible for the **localized myocardial blood flow redistribution** characteristic of the coronary steal phenomenon.
- Coronary steal is a physiological process related to **vasoreactivity** and not hypovolemia.
Cardiovascular responses to exercise US Medical PG Question 7: A 42-year-old firefighter candidate undergoes VO2 max testing showing 32 mL/kg/min (below required 42 mL/kg/min). His body composition shows 28% body fat. He has normal cardiac function (ejection fraction 60%), hemoglobin 15.2 g/dL, and no respiratory disease. Lactate threshold occurs at 65% of VO2 max. Evaluate the most effective evidence-based training strategy to meet occupational requirements within 12 weeks.
- A. Resistance training focusing on muscular strength to improve work efficiency
- B. High-intensity interval training (HIIT) at 90-95% VO2 max with active recovery
- C. Threshold training at lactate threshold intensity for extended durations
- D. Continuous moderate-intensity training at 60-70% VO2 max for 60 minutes daily
- E. Combined approach: HIIT twice weekly plus threshold training three times weekly (Correct Answer)
Cardiovascular responses to exercise Explanation: ***Combined approach: HIIT twice weekly plus threshold training three times weekly***
- A combined protocol is superior for maximizing **VO2 max** and improving the **lactate threshold** simultaneously within a short 12-week window.
- **High-Intensity Interval Training (HIIT)** effectively increases **stroke volume** and maximal cardiac output, while **threshold training** enhances peripheral adaptations like **mitochondrial density**.
*Resistance training focusing on muscular strength to improve work efficiency*
- While strength is important for firefighting, it does not significantly elevate **VO2 max** or the **aerobic capacity** needed to meet the 42 mL/kg/min requirement.
- This strategy primarily improves **neuromuscular recruitment** and absolute power rather than the **oxygen transport system**.
*High-intensity interval training (HIIT) at 90-95% VO2 max with active recovery*
- Although HIIT is a potent stimulus for cardiovascular gains, relying solely on HIIT may lead to **overtraining** or injury if performed at the frequency needed to meet the target.
- It lacks the high-volume metabolic stress provided by **threshold training** that is necessary to shift the **anaerobic threshold** optimally.
*Threshold training at lactate threshold intensity for extended durations*
- Threshold training alone improves **metabolic efficiency** but is less effective than HIIT at increasing the **central cardiovascular limits** like maximal stroke volume.
- This approach might improve endurance at current levels but often results in a plateau in **maximal aerobic power (VO2 max)**.
*Continuous moderate-intensity training at 60-70% VO2 max for 60 minutes daily*
- Moderate-intensity training is insufficient to stimulate the significant **10 mL/kg/min increase** required for this candidate within 12 weeks.
- This intensity primarily improves **lipid oxidation** and base endurance rather than the maximal **oxygen consumption** required for occupational clearance.
Cardiovascular responses to exercise US Medical PG Question 8: A 38-year-old woman with mitochondrial myopathy due to a complex I deficiency presents with severe exercise intolerance. Her baseline lactate is 3.2 mmol/L (normal <2.0) and rises to 12.8 mmol/L after minimal exercise. Her VO2 max is 18 mL/kg/min. Cardiopulmonary and hematologic evaluations are normal. Evaluate the pathophysiologic mechanism and optimal exercise approach.
- A. Defective electron transport chain necessitates low-intensity aerobic exercise below anaerobic threshold (Correct Answer)
- B. Excessive lactate production mandates complete exercise avoidance to prevent rhabdomyolysis
- C. Mitochondrial dysfunction requires carbohydrate restriction to force fatty acid oxidation adaptation
- D. Impaired oxidative phosphorylation requires high-intensity interval training to stimulate mitochondrial biogenesis
- E. Complex I deficiency indicates need for supplemental oxygen during exercise to bypass metabolic block
Cardiovascular responses to exercise Explanation: ***Defective electron transport chain necessitates low-intensity aerobic exercise below anaerobic threshold***
- Complex I deficiency impairs **oxidative phosphorylation**, causing a shift to **anaerobic metabolism** and early **lactic acidosis** even with minimal exertion.
- Training at a low intensity below the **anaerobic threshold** allows for the utilization of what limited oxidative capacity remains while avoiding dangerous surges in **lactate levels**.
*Excessive lactate production mandates complete exercise avoidance to prevent rhabdomyolysis*
- Complete **exercise avoidance** leads to progressive **deconditioning** and a further decline in functional capacity and muscle strength.
- While high exertion is risky, **monitored, submaximal exercise** is generally safe and helps maintain metabolic fitness in mitochondrial patients.
*Mitochondrial dysfunction requires carbohydrate restriction to force fatty acid oxidation adaptation*
- **Fatty acid oxidation** still requires a functional **electron transport chain** (ETC) to produce ATP; restricted carbohydrates would deprive the body of an essential fuel source.
- Complex I deficiency blocks the re-oxidation of **NADH**, a process required for both carbohydrate and fat metabolism, making restriction counterproductive.
*Impaired oxidative phosphorylation requires high-intensity interval training to stimulate mitochondrial biogenesis*
- **High-intensity interval training (HIIT)** pushes the body significantly above the **anaerobic threshold**, which could trigger severe metabolic crises in this patient.
- Excessive **lactic acid accumulation** (12.8 mmol/L) at minimal exercise indicates that high-intensity loads exceed the patient's immediate buffering and metabolic capabilities.
*Complex I deficiency indicates need for supplemental oxygen during exercise to bypass metabolic block*
- Supplemental oxygen increases the **partial pressure of oxygen** in the blood but does not fix the **intracellular metabolic block** within the mitochondria.
- The pathology in this patient is not an **oxygen delivery** issue (normal cardiopulmonary eval) but an **oxygen utilization** defect at the ETC level.
Cardiovascular responses to exercise US Medical PG Question 9: A 55-year-old man with hypertension controlled on metoprolol 100 mg daily wants to start an exercise program. His resting heart rate is 58 bpm, blood pressure 128/78 mmHg. During exercise testing, his heart rate reaches only 118 bpm at perceived maximal exertion (predicted maximum 165 bpm), but he achieves adequate workload with RPE of 18/20. Evaluate the most appropriate exercise prescription approach.
- A. Switch to a calcium channel blocker to preserve chronotropic response
- B. Use rating of perceived exertion (RPE) rather than target heart rate (Correct Answer)
- C. Perform exercise at lower intensity due to blunted heart rate response
- D. Discontinue metoprolol to achieve target heart rate during exercise
- E. Add dobutamine during exercise to increase heart rate and contractility
Cardiovascular responses to exercise Explanation: ***Use rating of perceived exertion (RPE) rather than target heart rate***
- **Beta-blockers** like **metoprolol** attenuate the **chronotropic response**, leading to a blunted heart rate that does not accurately reflect exercise intensity.
- The **Borg scale** or **RPE** is the most reliable method for monitoring intensity in these patients because it correlates with metabolic demand regardless of medication-induced heart rate suppression.
*Switch to a calcium channel blocker to preserve chronotropic response*
- There is no clinical indication to switch an effective **antihypertensive therapy** solely to modify the physiological response to exercise when alternative monitoring tools exist.
- Certain calcium channel blockers, such as **verapamil** or **diltiazem**, also possess **negative chronotropic effects** similar to beta-blockers.
*Perform exercise at lower intensity due to blunted heart rate response*
- The blunted heart rate is a pharmacological effect, not a sign of **cardiovascular dysfunction** or limited aerobic capacity.
- Restricting intensity based only on heart rate would lead to **under-training**, given the patient reached an **RPE of 18/20** and performed adequate workload.
*Discontinue metoprolol to achieve target heart rate during exercise*
- Discontinuing a necessary medication for **hypertension** control poses significant health risks like **rebound hypertension** or tachycardia.
- Achieving a specific **target heart rate** is a secondary goal compared to maintaining stable blood pressure and overall cardiovascular safety.
*Add dobutamine during exercise to increase heart rate and contractility*
- **Dobutamine** is a pharmacological stress agent used in diagnostic testing, not as an adjunct for routine physical exercise programs.
- Using a **beta-agonist** to counteract the effects of a **beta-antagonist** is counterproductive and clinically inappropriate for exercise prescription.
Cardiovascular responses to exercise US Medical PG Question 10: A 25-year-old elite swimmer training at sea level travels to compete at altitude (2400 meters). After 2 days of acclimatization, she experiences decreased performance. Her arterial blood gas shows pH 7.46, PaO2 65 mmHg, PaCO2 32 mmHg, HCO3- 22 mEq/L. Analyze the limiting factor for her current exercise performance at altitude.
- A. Incomplete respiratory compensation reducing oxygen delivery
- B. Decreased plasma volume reducing stroke volume and cardiac output
- C. Alkalosis shifting the oxygen-hemoglobin dissociation curve leftward
- D. Inadequate time for erythropoietin-stimulated red blood cell production (Correct Answer)
- E. Reduced oxidative enzyme activity in skeletal muscle mitochondria
Cardiovascular responses to exercise Explanation: ***Inadequate time for erythropoietin-stimulated red blood cell production***
- While **erythropoietin (EPO)** levels rise within hours of altitude exposure, a significant increase in **red blood cell mass** and **hemoglobin** concentration requires approximately 2 to 3 weeks.
- After only 2 days, the athlete has a reduced **arterial oxygen content (CaO2)** due to low **PaO2** without the compensatory increase in oxygen-carrying capacity needed for elite performance.
*Incomplete respiratory compensation reducing oxygen delivery*
- The ABG shows a **PaCO2 of 32 mmHg** and a **pH of 7.46**, indicating that **hyperventilation** (respiratory compensation) is actively occurring to mitigate hypoxia.
- Respiratory compensation occurs rapidly (minutes to hours) and is not the primary limiting factor after 2 days compared to the lack of **polycythemia**.
*Decreased plasma volume reducing stroke volume and cardiac output*
- **Plasma volume** does decrease shortly after reaching altitude due to **bicarbonate diuresis** and suppression of aldosterone, which can lead to a hemoconcentration effect.
- However, this relative increase in hematocrit is insufficient to match the absolute increase in **red cell mass** required for sustained high-intensity exercise at altitude.
*Alkalosis shifting the oxygen-hemoglobin dissociation curve leftward*
- **Respiratory alkalosis** (pH 7.46) causes a **left shift** in the oxygen-hemoglobin dissociation curve, which increases oxygen affinity in the lungs but impairs **unloading at the tissues**.
- While this inhibits oxygen delivery, it is a physiologic consequence of hyperventilation and is partially offset by an eventual increase in **2,3-BPG**; it is not the main driver of performance loss compared to total oxygen content.
*Reduced oxidative enzyme activity in skeletal muscle mitochondria*
- **Mitochondrial density** and **oxidative enzyme activity** generally remain stable or may even decrease slightly during long-term altitude acclimatization.
- Changes in muscle biochemistry are **chronic adaptations** and do not explain acute performance decreases within a 48-hour window.
More Cardiovascular responses to exercise US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.