Exercise physiology

On this page
🏃 The Exercise Physiology Command Center: Mastering Human Performance
Exercise transforms every system in your body, from the ATP molecules powering each muscle contraction to the cardiovascular adjustments delivering oxygen under stress. You'll discover how energy systems activate in sequence, how your heart and lungs coordinate to meet metabolic demands, and why heat balance and neuromuscular fatigue ultimately limit performance. By integrating these physiological responses, you'll gain the clinical insight to optimize training, prescribe exercise therapeutically, and understand human performance at its most fundamental level.
🏃 The Exercise Physiology Command Center: Mastering Human Performance
💪 The Metabolic Powerhouse: Energy System Mastery
📌 Remember: PCr-GPS - Phosphocreatine for Creatine regeneration, Glycolysis for Power, Sustained oxidation for endurance
-
Phosphocreatine System (0-15 seconds)
- Peak power: 9+ mmol ATP/kg/sec
- Fuel source: Stored creatine phosphate (15-25 mmol/kg)
- Oxygen requirement: Zero (alactic)
- Recovery time: 2-3 minutes for 95% restoration
- Clinical relevance: Explosive movements, weightlifting
-
Glycolytic System (15 seconds - 2 minutes)
- Peak power: 4-5 mmol ATP/kg/sec
- Fuel source: Muscle glycogen (300-600g total body stores)
- Lactate production: 15-25 mmol/L at exhaustion
- pH decrease: 7.4 → 6.8 in active muscle
- Recovery time: 15-60 minutes for lactate clearance
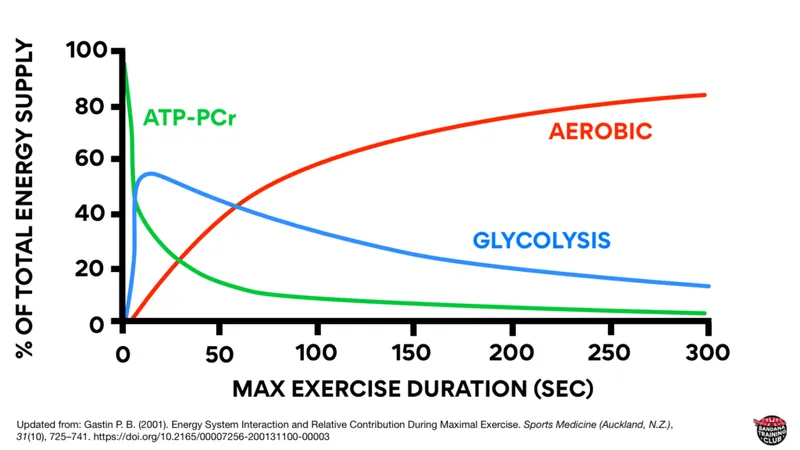
| System | Duration | Power Output | Fuel Source | Oxygen Need | Recovery Time |
|---|---|---|---|---|---|
| Phosphocreatine | 0-15 sec | 9+ mmol/kg/sec | PCr stores | None | 2-3 min |
| Glycolytic | 15 sec-2 min | 4-5 mmol/kg/sec | Muscle glycogen | None | 15-60 min |
| Oxidative | 2+ min | 1-2 mmol/kg/sec | CHO/Fat/Protein | High | Hours-days |
💡 Master This: Energy system contribution follows the power-duration relationship: as exercise duration increases, maximum sustainable power decreases exponentially, with 50% power reduction occurring every 2-3 minutes of sustained effort.
The oxidative system provides unlimited duration capacity but lower power output of 1-2 mmol ATP/kg/sec. This system utilizes carbohydrates (4 kcal/g), fats (9 kcal/g), and proteins (4 kcal/g) with complete oxygen dependence. Fat oxidation requires 15% more oxygen per ATP molecule compared to carbohydrate, explaining the metabolic efficiency advantage of glucose during high-intensity exercise.
Understanding energy system transitions predicts training adaptations and performance limitations across all exercise modalities.
💪 The Metabolic Powerhouse: Energy System Mastery
🫀 The Cardiovascular Engine: Hemodynamic Orchestration
📌 Remember: HEART - Heart rate up, Ejection fraction up, Afterload down, Return enhanced, Tissue perfusion optimized
-
Central Cardiovascular Adaptations
- Cardiac output: 5L/min → 20-35L/min (maximal exercise)
- Heart rate: 60-80 bpm → 180-220 bpm (age-dependent maximum)
- Stroke volume: 70mL → 110-160mL (trained athletes)
- Ejection fraction: 55-60% → 70-80% during exercise
- End-diastolic volume: 120mL → 140-180mL (enhanced venous return)
-
Peripheral Vascular Adaptations
- Systemic vascular resistance: ↓60-80% in active muscles
- Blood flow redistribution: Skeletal muscle 15% → 85% of cardiac output
- Arteriovenous oxygen difference: 5mL/dL → 15-17mL/dL
- Capillary recruitment: 25% → 90% of available capillaries
- Oxygen extraction: 25% → 85% in working muscle
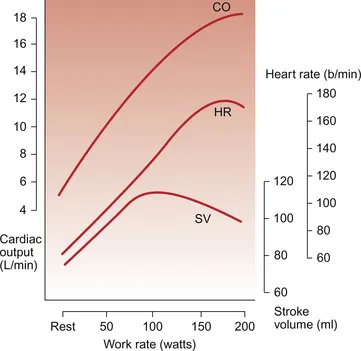
| Parameter | Rest | Moderate Exercise | Maximal Exercise | Adaptation |
|---|---|---|---|---|
| Heart Rate | 70 bpm | 120-140 bpm | 180-200 bpm | ↑200-300% |
| Stroke Volume | 70 mL | 100-120 mL | 110-160 mL | ↑50-130% |
| Cardiac Output | 5 L/min | 12-17 L/min | 20-35 L/min | ↑400-600% |
| A-V O₂ Diff | 5 mL/dL | 10-12 mL/dL | 15-17 mL/dL | ↑200-240% |
| Blood Pressure | 120/80 | 140-160/80 | 180-220/80 | ↑SBP only |
Blood flow redistribution represents a masterpiece of physiological control. Splanchnic blood flow decreases from 25% to 3-5% of cardiac output, while renal flow drops from 20% to 2-4%. Simultaneously, skeletal muscle blood flow increases from 15-20% to 80-85% through coordinated vasodilation and sympathetic vasoconstriction in non-exercising tissues.
💡 Master This: The Fick equation (VO₂ = Cardiac Output × A-V O₂ difference) reveals that exercise capacity depends equally on oxygen delivery (cardiovascular) and oxygen extraction (muscular), with elite athletes optimizing both components.
Understanding cardiovascular exercise responses enables precise exercise prescription and reveals the physiological basis for training-induced performance improvements.
🫀 The Cardiovascular Engine: Hemodynamic Orchestration
🫁 The Respiratory Powerhouse: Ventilatory Command and Control
📌 Remember: VENT-3 - Ventilation Escalates in Neural, Thermal, and 3 metabolic phases (CO₂, pH, O₂)
-
Ventilatory Control Mechanisms
- Central command: Immediate (0-15 sec) neural drive from motor cortex
- Mechanoreceptors: Muscle/joint feedback during movement
- Chemoreceptors: CO₂/pH (primary), O₂ (secondary) detection
- Central chemoreceptors: 80% of CO₂ response (medulla)
- Peripheral chemoreceptors: 20% of CO₂ response + hypoxia detection
- Ventilatory threshold: 50-60% VO₂max (untrained), 70-80% VO₂max (trained)
-
Gas Exchange Optimization
- Alveolar ventilation: 4-5 L/min → 80-120 L/min (maximal exercise)
- Respiratory rate: 12-16 breaths/min → 40-60 breaths/min
- Tidal volume: 500mL → 2000-3000mL (approaching vital capacity)
- Dead space ventilation: 150mL remains constant (↓relative contribution)
- Ventilation-perfusion matching: 0.8 → 1.0-1.2 (V/Q ratio)
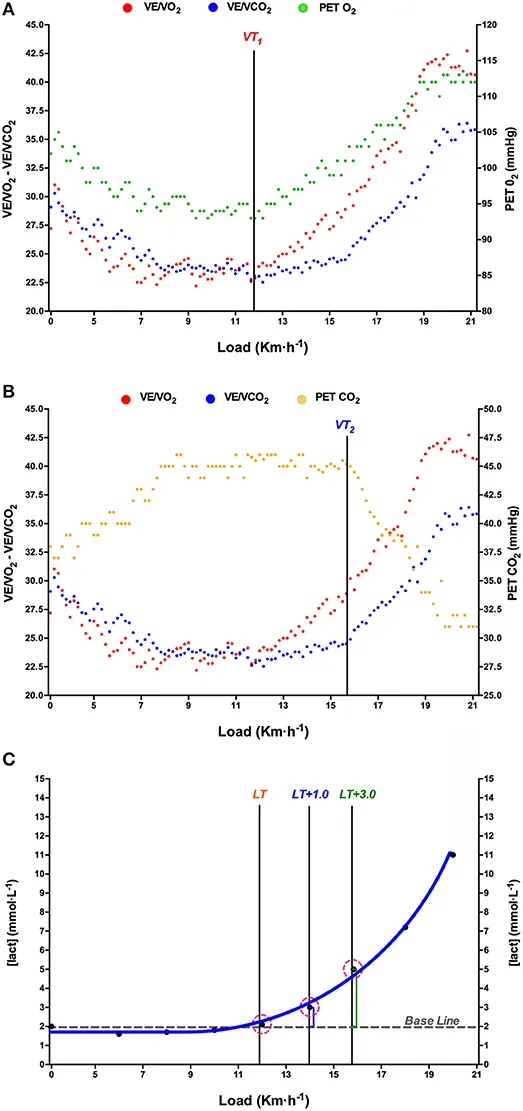
| Intensity | Ventilation | RR | TV | VE/VO₂ | VE/VCO₂ | Pattern |
|---|---|---|---|---|---|---|
| Rest | 6-8 L/min | 12-16 | 500mL | 25-30 | 25-30 | Linear |
| Moderate | 30-50 L/min | 20-30 | 1500-2000mL | 25-30 | 25-30 | Linear |
| VT1 | 60-80 L/min | 30-40 | 2000-2500mL | 30-35 | 25-30 | Breakpoint |
| VT2 | 100-150 L/min | 40-50 | 2500-3000mL | 35-45 | 30-40 | Exponential |
| Maximal | 150-200 L/min | 50-60 | 3000mL+ | 40-50 | 35-45 | Plateau |
The respiratory exchange ratio (RER = VCO₂/VO₂) provides real-time insight into metabolic fuel utilization. Values of 0.70 indicate pure fat oxidation, 0.85 represents mixed fuel utilization, and 1.00+ reflects carbohydrate dominance with anaerobic contribution. During maximal exercise, RER can exceed 1.15 due to bicarbonate buffering of metabolic acidosis.
💡 Master This: Ventilatory thresholds occur at 50-60% VO₂max (VT1, aerobic threshold) and 80-90% VO₂max (VT2, anaerobic threshold), representing critical metabolic transition points that determine sustainable exercise intensity.
Respiratory muscle fatigue becomes limiting during prolonged high-intensity exercise, with diaphragmatic blood flow competing with locomotor muscles for cardiac output allocation. This phenomenon explains the metaboreflex response, where respiratory muscle fatigue triggers sympathetic vasoconstriction in exercising limbs.
Understanding ventilatory control mechanisms enables precise interpretation of exercise testing data and optimization of training intensity zones.
🫁 The Respiratory Powerhouse: Ventilatory Command and Control
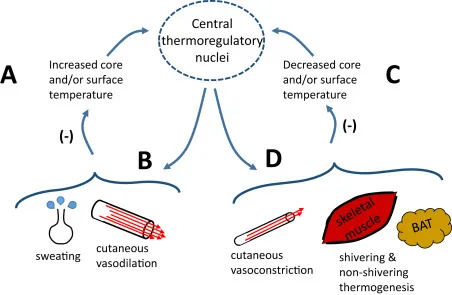
🔥 The Thermoregulatory Network: Heat Balance Mastery
📌 Remember: HEAT-LOSS - Heat production ↑, Evaporation primary, Acclimatization essential, Temperature regulated, Losses via 4 routes, Overload causes illness, Sweating saves, Salt matters
-
Heat Production Mechanisms
- Resting heat production: 80-100 watts (1-1.2 kcal/min)
- Moderate exercise: 400-600 watts (6-9 kcal/min)
- Maximal exercise: 1200-1500 watts (18-22 kcal/min)
- Mechanical efficiency: 20-25% (trained athletes up to 28%)
- Heat storage rate: 8-12°C/hour without cooling mechanisms
- Critical core temperature: 40-42°C (performance decrement begins)
-
Heat Loss Pathways
- Radiation: 60% at rest, ↓15-20% during exercise
- Convection: 15% at rest, ↓5-10% during exercise
- Conduction: 3% at rest, minimal during exercise
- Evaporation: 22% at rest, ↑70-80% during exercise
- Sweat rate: 0.5-1.0 L/hour (untrained), 2.0-3.5 L/hour (trained)
- Evaporative cooling: 580 kcal per liter of sweat evaporated
| Environmental Condition | Sweat Rate | Core Temp Rise | Performance Impact | Heat Illness Risk |
|---|---|---|---|---|
| Cool (10-15°C) | 0.5-1.0 L/hr | 1-2°C | Minimal | Low |
| Moderate (20-25°C) | 1.0-2.0 L/hr | 2-3°C | 5-10% ↓ | Low-Moderate |
| Hot (30-35°C) | 2.0-3.0 L/hr | 3-4°C | 15-25% ↓ | Moderate-High |
| Extreme (>35°C) | 3.0+ L/hr | 4+°C | >25% ↓ | High-Critical |
The hypothalamic thermoregulatory center integrates thermal input from core and skin thermoreceptors, initiating responses when core temperature rises >0.5°C above baseline. Sympathetic activation triggers cutaneous vasodilation (increasing skin blood flow from 5% to 15-20% of cardiac output) and eccrine sweat gland activation.
💡 Master This: Critical water loss occurs at 2-3% body weight, causing 10-15% performance decrement, while >5% dehydration leads to heat exhaustion and >7% approaches heat stroke territory with core temperatures >40°C.
Electrolyte balance becomes critical during prolonged exercise, with sodium losses of 20-80 mmol/L of sweat depending on acclimatization status. Hyponatremia risk increases when fluid replacement exceeds 1.5 L/hour without adequate sodium replacement (300-700 mg/hour recommended).
Understanding thermoregulatory physiology enables safe exercise prescription in challenging environmental conditions and prevents heat-related illness.

🔥 The Thermoregulatory Network: Heat Balance Mastery
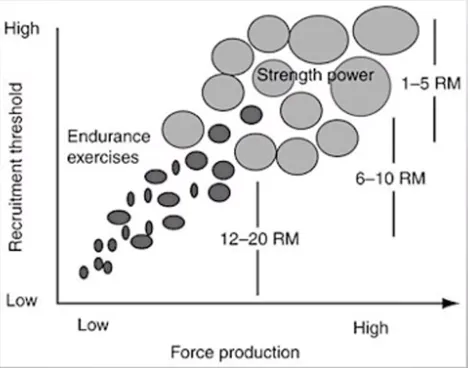
⚡ The Neuromuscular Command: Fiber Recruitment and Fatigue
📌 Remember: FIBER-TYPES - Fast vs slow, Innervation size principle, Blood supply differs, Energy systems vary, Recruitment ordered, Training adapts, Yield force differently, Power vs endurance, Enzymes specialized, Speed varies
-
Type I Fibers (Slow-Twitch Oxidative)
- Composition: 40-50% in untrained, 60-80% in endurance athletes
- Contraction time: 100-120 msec to peak tension
- Force production: Low (10-15 N/cm²)
- Fatigue resistance: High (>60 minutes sustained activity)
- Mitochondrial density: 15-20% of fiber volume
- Capillary density: 4-6 capillaries per fiber
- Oxidative enzymes: High (citrate synthase 40-60 μmol/g/min)
-
Type IIa Fibers (Fast-Twitch Oxidative-Glycolytic)
- Composition: 30-40% in untrained, 20-35% in power athletes
- Contraction time: 50-70 msec to peak tension
- Force production: Moderate-High (20-30 N/cm²)
- Fatigue resistance: Moderate (5-15 minutes high-intensity)
- Mitochondrial density: 8-12% of fiber volume
- Glycolytic capacity: Moderate-High
- Hybrid characteristics: Trainable toward Type I or IIx
| Fiber Type | % Composition | Contraction Speed | Force Output | Fatigue Resistance | Primary Energy |
|---|---|---|---|---|---|
| Type I | 40-50% | 100-120 msec | 10-15 N/cm² | >60 min | Oxidative |
| Type IIa | 30-40% | 50-70 msec | 20-30 N/cm² | 5-15 min | Mixed |
| Type IIx | 10-20% | 30-50 msec | 35-45 N/cm² | <2 min | Glycolytic |
Neuromuscular fatigue manifests through both central and peripheral mechanisms. Central fatigue involves ↓motor unit recruitment and ↓firing frequency from supraspinal centers, while peripheral fatigue results from metabolic accumulation (H⁺, Pi, K⁺), excitation-contraction coupling failure, and substrate depletion.
💡 Master This: The force-velocity relationship demonstrates that maximum force production occurs at zero velocity (isometric), while maximum velocity occurs at zero load, with power output peaking at approximately 30-35% of maximum force.
Training adaptations modify fiber characteristics through enzyme upregulation, mitochondrial biogenesis, and capillarization. Endurance training increases oxidative enzyme activity by 50-100% and mitochondrial density by 40-80%, while resistance training enhances contractile protein synthesis and neural recruitment patterns.
Understanding neuromuscular physiology enables targeted training prescription and explains individual variations in exercise capacity and training responsiveness.
⚡ The Neuromuscular Command: Fiber Recruitment and Fatigue
🎯 The Performance Integration Matrix: Clinical Exercise Mastery
📌 Remember: EXERCISE-Rx - Evaluate first, Xamine limitations, Establish goals, Risk stratify, Calculate intensity, Implement FITT-VP, Supervise initially, Evaluate progress, Revise as needed, x-tra safety always
-
Intensity Prescription Methods
- Heart rate reserve: Target HR = (HRmax - HRrest) × %intensity + HRrest
- VO₂ reserve: Target VO₂ = (VO₂max - VO₂rest) × %intensity + VO₂rest
- Rating of perceived exertion: Borg 6-20 scale (12-16 = moderate intensity)
- Moderate intensity: 40-60% HRR, 3-6 METs, RPE 12-14
- Vigorous intensity: 60-85% HRR, 6+ METs, RPE 14-17
- Talk test: Comfortable conversation (moderate), broken sentences (vigorous)
-
Clinical Exercise Testing Applications
- Diagnostic: CAD detection (85% sensitivity, 77% specificity)
- Prognostic: Duke Treadmill Score (risk stratification)
- Functional capacity: Peak VO₂ assessment (mL/kg/min)
- Normal values: >25 mL/kg/min (women), >35 mL/kg/min (men)
- Cardiovascular risk: <15 mL/kg/min (high risk), 15-25 (moderate)
- Athletic performance: >50 mL/kg/min (endurance athletes)
| Population | Frequency | Intensity | Time | Type | Special Considerations |
|---|---|---|---|---|---|
| Healthy Adults | 3-5 days/week | 40-85% HRR | 20-60 min | Aerobic + Resistance | 150 min/week moderate |
| Cardiac Rehab | 3-4 days/week | 40-70% HRR | 20-40 min | Supervised aerobic | Telemetry monitoring |
| Diabetes | 5+ days/week | 50-70% HRR | 30-60 min | Mixed modalities | Glucose monitoring |
| Elderly | 3-4 days/week | 30-60% HRR | 20-45 min | Low impact + balance | Fall prevention focus |
Contraindications to exercise testing include unstable angina, uncontrolled arrhythmias, acute myocarditis, severe aortic stenosis (valve area <1.0 cm²), and uncontrolled hypertension (>180/110 mmHg). Relative contraindications require careful risk-benefit analysis and may include recent MI (<2 days), complex ventricular ectopy, and severe pulmonary hypertension.
💡 Master This: The metabolic equivalent (MET) system enables universal exercise prescription, with 1 MET = 3.5 mL O₂/kg/min, allowing precise intensity matching across different activities and populations regardless of body weight or fitness level.
Special population considerations require modified approaches. Cardiac patients benefit from telemetry monitoring during initial phases, with intensity limited to 40-70% HRR and RPE 11-14. Diabetic patients require glucose monitoring before, during, and after exercise, with carbohydrate supplementation for sessions >60 minutes or when glucose <100 mg/dL.
Understanding integrated exercise physiology enables evidence-based clinical practice, optimizing therapeutic outcomes while minimizing adverse events across diverse patient populations.
🎯 The Performance Integration Matrix: Clinical Exercise Mastery
Practice Questions: Exercise physiology
Test your understanding with these related questions
A 35-year-old woman presents to the clinic for a several-month history of heat intolerance. She lives in a small apartment with her husband and reports that she always feels hot and sweaty, even when their air conditioning is on high. On further questioning, she's also had a 4.5 kg (10 lb) unintentional weight loss. The vital signs include: heart rate 102/min and blood pressure 150/80 mm Hg. The physical exam is notable for warm and slightly moist skin. She also exhibits a fine tremor in her hands when her arms are outstretched. Which of the following laboratory values is most likely low in this patient?













