Thyroid hormone transport and action US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid hormone transport and action. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid hormone transport and action US Medical PG Question 1: A 27-year-old woman comes to the physician because of a 2-month history of palpitations, diaphoresis, and a 5-kg (11-lb) weight loss. Her pulse is 101/min and blood pressure is 141/84 mm Hg. Physical examination shows a fine tremor when the fingers are outstretched. After confirmation of the diagnosis, treatment is begun with an antithyroid medication. The physician emphasizes the need for adequate contraception because of the increased risk of severe fetal malformations associated with the use of this medication, which is why its use is discouraged in the first trimester of pregnancy. Which of the following best describes the mechanism of action of this drug?
- A. Inhibition of thyroid hormone release
- B. Inhibition of peripheral conversion of T4 to T3
- C. Decreased iodide uptake by follicular cells
- D. Suppression of thyroid-stimulating hormone release
- E. Inhibition of iodide ion oxidation (Correct Answer)
Thyroid hormone transport and action Explanation: ***Inhibition of iodide ion oxidation***
- The patient's symptoms (palpitations, diaphoresis, weight loss, tremor, tachycardia, hypertension) are classic for **hyperthyroidism**, likely **Graves' disease**.
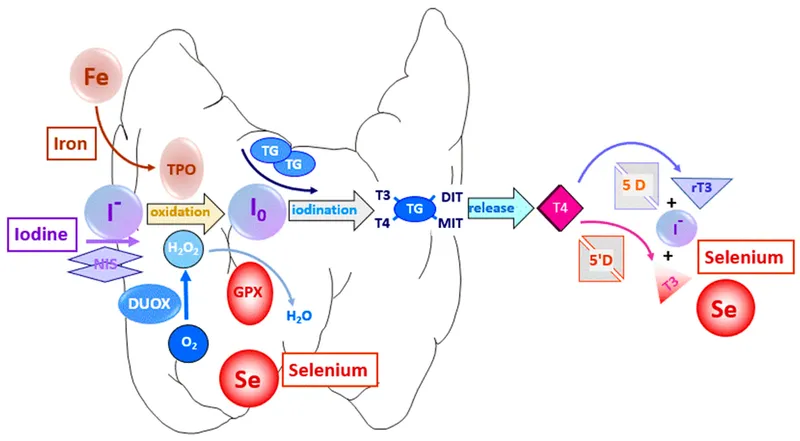
- The antithyroid drug described, which is contraindicated in the first trimester due to teratogenicity, is **methimazole**. Methimazole (and propylthiouracil) primarily inhibits **thyroid peroxidase**, thereby preventing the **oxidation of iodide** and its subsequent organification into tyrosine residues on thyroglobulin, blocking thyroid hormone synthesis.
*Inhibition of thyroid hormone release*
- This mechanism is characteristic of **iodides** (e.g., Lugol's solution, potassium iodide), which acutely inhibit the release of pre-formed thyroid hormones from the thyroid gland.
- While iodides can be used for rapid control of hyperthyroidism (e.g., before surgery or in thyroid storm), they are not the primary long-term antithyroid medications and do not carry the specific first-trimester teratogenicity risk described for PTU/methimazole.
*Inhibition of peripheral conversion of T4 to T3*
- This mechanism is primarily associated with **propylthiouracil (PTU)** (in addition to inhibiting thyroid hormone synthesis) and **beta-blockers** (like propranolol), as well as **glucocorticoids** and **amiodarone**.
- While PTU also inhibits iodide oxidation, its unique ability to inhibit peripheral T4 to T3 conversion makes it the preferred antithyroid drug in the **first trimester of pregnancy** due to a lower teratogenic risk compared to methimazole, directly contrasting the drug described in the question.
*Decreased iodide uptake by follicular cells*
- This is the mechanism of action of **perchlorate** and **thiocyanate**, which are competitive inhibitors of the **sodium-iodide symporter (NIS)**, blocking iodide transport into follicular cells.
- These agents are rarely used clinically due to toxicity concerns and are not the first-line antithyroid drugs with the described teratogenic profile.
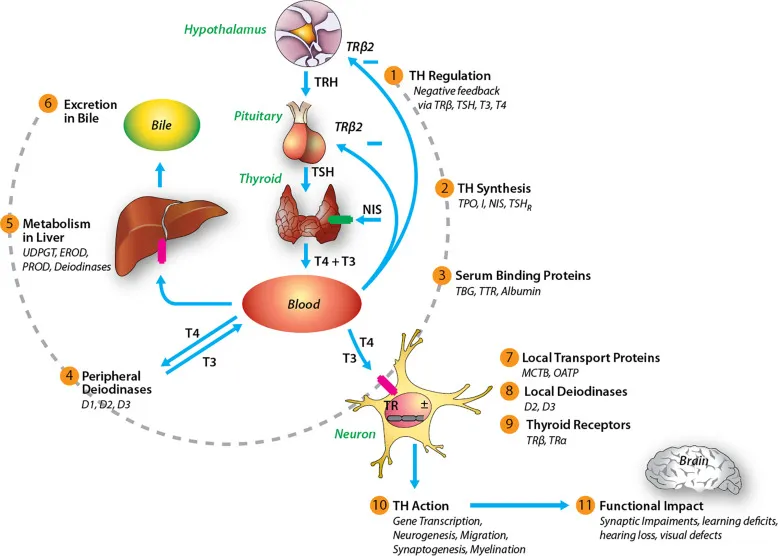
*Suppression of thyroid-stimulating hormone release*
- **TSH release** from the pituitary is primarily suppressed by **negative feedback** from high levels of circulating thyroid hormones (T3 and T4), or by direct intervention with agents like **somatostatin analogs** (e.g., octreotide) in rare cases of TSH-producing pituitary adenomas.
- Antithyroid drugs do not directly suppress TSH release; rather, by reducing thyroid hormone levels, they would eventually lead to an *increase* in TSH secretion if hyperthyroidism were adequately treated and feedback restored.
Thyroid hormone transport and action US Medical PG Question 2: A 49-year-old woman presents to the office because of tremors for 2 months. She says that her hands have been shaking a lot, especially when she feels stressed. In addition, she has been sweating more than usual and has lost 8 kg (17.6 lb) in the last 2 months. She has a past medical history of vitiligo. Her vital signs are a heart rate of 98/min, a respiratory rate of 14/min, a temperature of 37.6°C (99.7°F), and a blood pressure of 115/75 mm Hg. Physical examination shows a fine, bilateral hand tremor and a diffuse goiter. Which of the following hormonal imbalances is most likely present?
- A. Low TSH, high free T4, and high free T3 (Correct Answer)
- B. High TSH, high free T4, and high free T3
- C. High TSH, normal free T4, and normal free T3
- D. Low TSH, normal free T4, and normal free T3
- E. High TSH, low free T4, and low free T3
Thyroid hormone transport and action Explanation: ***Low TSH, high free T4, and high free T3***
- The patient's symptoms (tremors, sweating, weight loss, tachycardia, goiter) are classic for **hyperthyroidism**, which is typically characterized by **low TSH** due to negative feedback and **elevated free T4 and T3** levels.
- Her history of **vitiligo**, an autoimmune condition, further supports an autoimmune thyroid disorder like **Graves' disease**, a common cause of hyperthyroidism.
*High TSH, high free T4, and high free T3*
- This pattern would indicate **secondary hyperthyroidism**, caused by a TSH-secreting pituitary adenoma.
- While TSH would be high, it is a much rarer cause of hyperthyroidism compared to primary causes.
*High TSH, normal free T4, and normal free T3*
- This hormonal profile is characteristic of **subclinical hypothyroidism** or a **compensated primary hypothyroidism** early in its course.
- The patient's symptoms are inconsistent with hypothyroidism.
*Low TSH, normal free T4, and normal free T3*
- This suggests **subclinical hyperthyroidism**, where TSH is suppressed but thyroid hormone levels are still within the normal range.
- The patient's prominent and severe symptoms (tremors, significant weight loss, goiter) indicate overt hyperthyroidism, not subclinical disease.
*High TSH, low free T4, and low free T3*
- This is the classic hormonal profile for **primary hypothyroidism**, where the thyroid gland is failing to produce sufficient hormones, leading to elevated TSH.
- The patient's symptoms of nervousness, weight loss, and tremors are directly opposite to those seen in hypothyroidism.
Thyroid hormone transport and action US Medical PG Question 3: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
Thyroid hormone transport and action Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
Thyroid hormone transport and action US Medical PG Question 4: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Thyroid hormone transport and action Explanation: ***Peripheral 5'-deiodinase***
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Thyroid hormone transport and action US Medical PG Question 5: A 43-year-old woman comes to the physician because of a 3-month history of tremor, diarrhea, and a 5-kg (11-lb) weight loss. Her pulse is 110/min. Examination shows protrusion of the eyeball when looking forward. A bruit is heard over the anterior neck on auscultation. Serum studies show autoantibodies to the thyroid-stimulating hormone receptor. The patient decides to undergo definitive treatment for her condition with a radioactive tracer. The success of this treatment directly depends on the activity of which of the following?
- A. Anion-oxidizing enzyme
- B. Transmembrane carrier (Correct Answer)
- C. Lysosomal protease
- D. Binding globulin
- E. Hormone-activating enzyme
Thyroid hormone transport and action Explanation: ***Transmembrane carrier***
- Radioactive iodine treatment relies on the uptake of iodine by thyroid follicular cells via the **sodium-iodide symporter (NIS)**, a **transmembrane carrier protein**.
- NIS actively transports iodide into thyroid cells, allowing the radioactive iodine to concentrate in the thyroid and destroy overactive tissue.
*Anion-oxidizing enzyme*
- This refers to **thyroid peroxidase (TPO)**, an enzyme that oxidizes iodide to iodine, incorporates iodine into thyroglobulin, and couples iodinated tyrosines.
- While essential for thyroid hormone synthesis, TPO's activity does not directly determine the success of **radioactive iodine uptake** for treatment.
*Lysosomal protease*
- **Lysosomal proteases** are involved in the breakdown of thyroglobulin to release thyroid hormones (T3 and T4) into circulation.
- They are important for the *release* of hormones but not for the *uptake* of iodine for radioactive treatment.
*Binding globulin*
- **Thyroxine-binding globulin (TBG)** is a plasma protein that transports thyroid hormones in the blood, maintaining a reservoir of T3 and T4.
- TBG's activity affects the availability of free thyroid hormones but has no direct role in the cellular uptake of radioactive iodine by the thyroid gland.
*Hormone-activating enzyme*
- This typically refers to deiodinases, enzymes that convert T4 (prohormone) into the more active T3 in peripheral tissues.
- These enzymes act *outside* the thyroid gland to activate hormones, and their activity does not directly influence the uptake of radioactive iodine.
Thyroid hormone transport and action US Medical PG Question 6: A 55-year-old woman has a total thyroidectomy for papillary thyroid carcinoma. She complains of tingling around the mouth 11 hours after the operation. Her condition rapidly deteriorates with difficulty breathing and chest tightness. Which of the following best represent the signaling pathway of the deficient hormone responsible for this patient’s symptoms?
- A. Cyclic guanosine monophosphate (cGMP)
- B. Cyclic adenosine monophosphate (cAMP) (Correct Answer)
- C. Intracellular receptors
- D. Receptor tyrosine kinase
- E. Inositol trisphosphate (IP3)
Thyroid hormone transport and action Explanation: ***Cyclic adenosine monophosphate (cAMP)***
- The patient's symptoms of perioral tingling, difficulty breathing, and chest tightness after total thyroidectomy suggest **hypocalcemia**, likely due to accidental removal or damage to the **parathyroid glands** during surgery.
- The deficient **parathyroid hormone (PTH)** acts primarily through the **cAMP second messenger system** to increase serum calcium levels.
*Cyclic guanosine monophosphate (cGMP)*
- **cGMP** is a second messenger system primarily involved in mediating the effects of hormones like **atrial natriuretic peptide (ANP)** and **nitric oxide**, which are unrelated to calcium homeostasis and parathyroid function.
- This pathway is not the primary mechanism of action for **PTH**.
*Intracellular receptors*
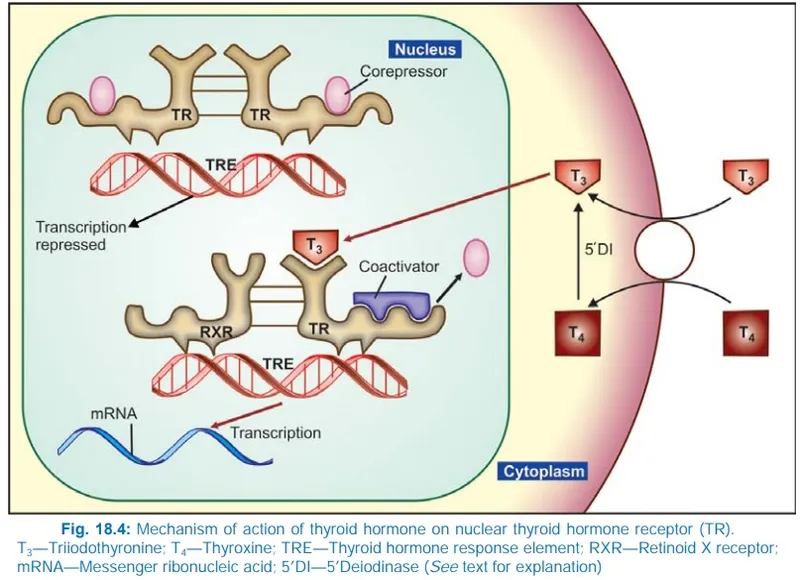
- **Intracellular receptors** are typically used by **steroid hormones** (e.g., cortisol, estrogen) and **thyroid hormones**, which are lipid-soluble and can cross the cell membrane.
- **PTH** is a peptide hormone and acts on cell surface receptors.
*Receptor tyrosine kinase*
- **Receptor tyrosine kinases (RTKs)** are transmembrane receptors involved in signaling pathways for hormones like **insulin** and **growth factors**, promoting cell growth, differentiation, and metabolism.
- This is not the primary signaling pathway for **PTH**.
*Inositol trisphosphate (IP3)*
- The **IP3/DAG (diacylglycerol)** pathway is another common second messenger system used by various hormones (e.g., **vasopressin, oxytocin, TRH**), leading to the release of intracellular calcium.
- While it involves calcium signaling, it is not the primary or most characteristic pathway for **PTH** action, which predominantly utilizes **cAMP**.
Thyroid hormone transport and action US Medical PG Question 7: A previously healthy 27-year-old man comes to the physician because of a 3-week history of anxiety, diarrhea, and a 4.1-kg (9-lb) weight loss. On questioning, he also reports that he noticed a painless mass on his left testicle 2 weeks ago. His pulse is 110/min and irregular and blood pressure is 150/70 mm Hg. Examination shows diaphoresis and a fine tremor of the outstretched fingers. Testicular examination shows a 3-cm, firm, nontender mass on the left scrotum that does not transilluminate. This patient's underlying condition is most likely to be associated with which of the following findings?
- A. Elevated serum AFP
- B. Elevated serum hCG (Correct Answer)
- C. Elevated serum TSH
- D. Proptosis on exophthalmometry
- E. Positive urine metanephrines
Thyroid hormone transport and action Explanation: ***Elevated serum hCG***
- The patient presents with symptoms of **hyperthyroidism** (anxiety, weight loss, tachycardia, tremor, diaphoresis) and a **testicular mass**.
- Some **testicular germ cell tumors**, particularly **choriocarcinoma** and some **mixed germ cell tumors**, can produce **hCG**, which has structural similarity to TSH and can stimulate the thyroid gland, leading to **paraneoplastic hyperthyroidism**.
- **Serum hCG** is an important tumor marker for germ cell tumors and would be elevated in this clinical scenario.
*Elevated serum AFP*
- **Alpha-fetoprotein (AFP)** is a tumor marker often elevated in **non-seminomatous germ cell tumors** like **yolk sac tumors** and **embryonal carcinomas**.
- While AFP may be elevated in some testicular tumors, it does not explain the hyperthyroid symptoms, as hCG (not AFP) has TSH-like activity.
*Elevated serum TSH*
- In **hyperthyroidism**, the **thyroid stimulating hormone (TSH)** level is typically **suppressed** due to negative feedback from high thyroid hormone levels.
- An elevated TSH would indicate **primary hypothyroidism**, which contradicts the patient's clinical presentation.
*Proptosis on exophthalmometry*
- **Proptosis** (exophthalmos) is a common finding in **Graves' disease**, an autoimmune cause of hyperthyroidism.
- However, the presence of a **testicular mass** strongly suggests a paraneoplastic etiology for the hyperthyroidism, making Graves' disease less likely as the primary underlying condition.
*Positive urine metanephrines*
- **Urine metanephrines** are markers elevated in **pheochromocytoma**, a tumor of the adrenal medulla that secretes catecholamines.
- While pheochromocytoma can cause hypertension, tachycardia, and anxiety, it does not typically present with a testicular mass or directly cause weight loss through a thyroid-like mechanism.
Thyroid hormone transport and action US Medical PG Question 8: An 18-year-old girl comes to the clinic because she is concerned about her weight. She states that she is on her school’s cheerleading team and is upset because she feels she is the “fattest” girl on the team despite her healthy diet. She says that in the last 2 weeks since practice began, she has lost 2 lbs. The patient has bipolar disorder I. Her medications include lithium and a combined oral contraceptive that was recently started by her gynecologist, because “everyone is on it." Her mother has hypothyroidism and is treated with levothyroxine. The patient’s BMI is 23.2 kg/m2. Thyroid function labs are drawn and shown below:
Thyroid-stimulating hormone (TSH): 4.0 mIU/L
Serum thyroxine (T4): 18 ug/dL
Free thyroxine (Free T4): 1.4 ng/dl (normal range: 0.7-1.9 ng/dL)
Serum triiodothyronine (T3): 210 ng/dL
Free triiodothyronine (T3): 6.0 pg/mL (normal range: 3.0-7.0 pg/mL)
Which of the following is the most likely cause of the patient’s abnormal lab values?
- A. Familial hyperthyroidism
- B. Hypocholesterolemia
- C. Lithium
- D. Oral contraception-induced (Correct Answer)
- E. Surreptitious use of levothyroxine
Thyroid hormone transport and action Explanation: ***Oral contraception-induced***
- The patient's **total T4 and T3 are elevated**, while **free T4 and T3** are within normal limits, indicating an increase in thyroid-binding globulin (TBG).
- Oral contraceptives, specifically **estrogen**, increase the synthesis of TBG in the liver, leading to higher total thyroid hormone levels as more hormone is bound.
*Familial hyperthyroidism*
- Familial hyperthyroidism would present with genuinely **elevated free T4 and T3** levels, alongside suppressed TSH, indicating true hyperthyroidism.
- The patient's **normal free T4 and T3** and slightly elevated TSH rule out true hyperthyroidism.
*Hypocholesterolemia*
- While thyroid hormones can affect lipid metabolism, **hypocholesterolemia is not a direct cause** of altered thyroid lab values.
- It is also not a common side effect of oral contraceptives, nor is it related to the specific pattern of elevated total T4/T3 with normal free hormones.
*Lithium*
- Lithium is known to **cause hypothyroidism** (elevated TSH, low T4/T3) or, less commonly, hyperthyroidism, but not isolated elevated total T4/T3 with normal free hormones due to increased TBG.
- The patient's normal free thyroid hormones and only slightly elevated TSH are not consistent with significant lithium-induced thyroid dysfunction.
*Surreptitious use of levothyroxine*
- Surreptitious use of exogenous **levothyroxine** would typically result in suppressed TSH and elevated free T4, as the gland would be overstimulated or shut down.
- The patient's normal free T4 and elevated total T4/T3 are not indicative of levothyroxine abuse.
Thyroid hormone transport and action US Medical PG Question 9: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Thyroid hormone transport and action Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Thyroid hormone transport and action US Medical PG Question 10: A neurophysiologist describes the mechanism of a specific type of synaptic transmission to his students. While illustrating this, he points out that when the action potential reaches the presynaptic terminal of a chemical synapse, the voltage-gated Ca2+ channels open. Ca2+ ions trigger the release of neurotransmitters from vesicles in the presynaptic terminal. In this type of synaptic transmission, increased cytosolic Ca2+ levels cause the release of a neurotransmitter from small vesicles with dense cores. Which of the following neurotransmitters is most likely to be the one that is released into the synaptic cleft in this type of synapse?
- A. Epinephrine
- B. Glutamate
- C. Glycine
- D. GABA (γ-amino butyric acid)
- E. Norepinephrine (Correct Answer)
Thyroid hormone transport and action Explanation: ***Norepinephrine***
- **Norepinephrine** is the primary catecholamine neurotransmitter stored in **small vesicles with dense cores** (dense-core vesicles).
- It is released from **sympathetic postganglionic neurons** and central nervous system neurons, particularly from the **locus coeruleus**.
- Dense-core vesicles are the hallmark of catecholaminergic neurons, and norepinephrine is the most abundant neuronal catecholamine.
- The description perfectly matches noradrenergic synaptic transmission.
*Epinephrine*
- While epinephrine is also a catecholamine stored in dense-core vesicles, it functions primarily as a **hormone** released from the **adrenal medulla** (not a neurotransmitter).
- Only a **very small number** of CNS neurons use epinephrine as a neurotransmitter (mainly in medullary regions).
- In the context of synaptic transmission, norepinephrine is far more common.
*Glutamate*
- **Glutamate** is the primary excitatory neurotransmitter in the CNS but is stored in **small, clear synaptic vesicles**, not dense-core vesicles.
- It does not fit the description of dense-core vesicle storage.
*Glycine*
- **Glycine** is an inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Found predominantly in the **spinal cord** and brainstem, not in dense-core vesicles.
*GABA (γ-amino butyric acid)*
- **GABA** is the main inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Not associated with dense-core vesicle storage.
More Thyroid hormone transport and action US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.