Regulation of thyroid function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Regulation of thyroid function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Regulation of thyroid function US Medical PG Question 1: A 27-year-old woman comes to the physician because of a 2-month history of palpitations, diaphoresis, and a 5-kg (11-lb) weight loss. Her pulse is 101/min and blood pressure is 141/84 mm Hg. Physical examination shows a fine tremor when the fingers are outstretched. After confirmation of the diagnosis, treatment is begun with an antithyroid medication. The physician emphasizes the need for adequate contraception because of the increased risk of severe fetal malformations associated with the use of this medication, which is why its use is discouraged in the first trimester of pregnancy. Which of the following best describes the mechanism of action of this drug?
- A. Inhibition of thyroid hormone release
- B. Inhibition of peripheral conversion of T4 to T3
- C. Decreased iodide uptake by follicular cells
- D. Suppression of thyroid-stimulating hormone release
- E. Inhibition of iodide ion oxidation (Correct Answer)
Regulation of thyroid function Explanation: ***Inhibition of iodide ion oxidation***
- The patient's symptoms (palpitations, diaphoresis, weight loss, tremor, tachycardia, hypertension) are classic for **hyperthyroidism**, likely **Graves' disease**.
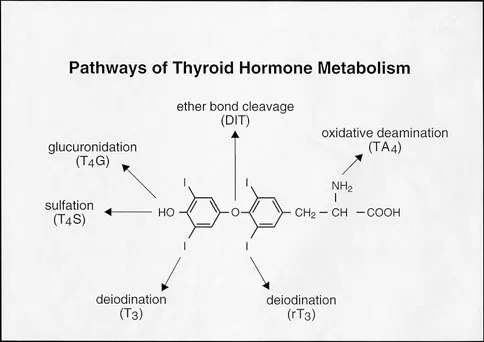
- The antithyroid drug described, which is contraindicated in the first trimester due to teratogenicity, is **methimazole**. Methimazole (and propylthiouracil) primarily inhibits **thyroid peroxidase**, thereby preventing the **oxidation of iodide** and its subsequent organification into tyrosine residues on thyroglobulin, blocking thyroid hormone synthesis.
*Inhibition of thyroid hormone release*
- This mechanism is characteristic of **iodides** (e.g., Lugol's solution, potassium iodide), which acutely inhibit the release of pre-formed thyroid hormones from the thyroid gland.
- While iodides can be used for rapid control of hyperthyroidism (e.g., before surgery or in thyroid storm), they are not the primary long-term antithyroid medications and do not carry the specific first-trimester teratogenicity risk described for PTU/methimazole.
*Inhibition of peripheral conversion of T4 to T3*
- This mechanism is primarily associated with **propylthiouracil (PTU)** (in addition to inhibiting thyroid hormone synthesis) and **beta-blockers** (like propranolol), as well as **glucocorticoids** and **amiodarone**.
- While PTU also inhibits iodide oxidation, its unique ability to inhibit peripheral T4 to T3 conversion makes it the preferred antithyroid drug in the **first trimester of pregnancy** due to a lower teratogenic risk compared to methimazole, directly contrasting the drug described in the question.
*Decreased iodide uptake by follicular cells*
- This is the mechanism of action of **perchlorate** and **thiocyanate**, which are competitive inhibitors of the **sodium-iodide symporter (NIS)**, blocking iodide transport into follicular cells.
- These agents are rarely used clinically due to toxicity concerns and are not the first-line antithyroid drugs with the described teratogenic profile.
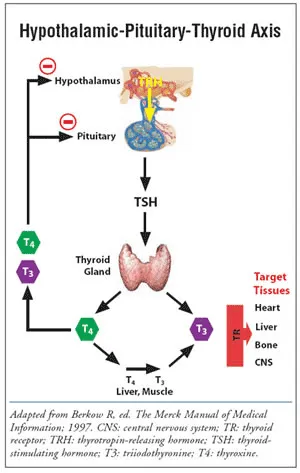
*Suppression of thyroid-stimulating hormone release*
- **TSH release** from the pituitary is primarily suppressed by **negative feedback** from high levels of circulating thyroid hormones (T3 and T4), or by direct intervention with agents like **somatostatin analogs** (e.g., octreotide) in rare cases of TSH-producing pituitary adenomas.
- Antithyroid drugs do not directly suppress TSH release; rather, by reducing thyroid hormone levels, they would eventually lead to an *increase* in TSH secretion if hyperthyroidism were adequately treated and feedback restored.
Regulation of thyroid function US Medical PG Question 2: A 27-year-old G1P0 at 12 weeks estimated gestational age presents for prenatal care. The patient says she has occasional nausea and vomiting and a few episodes of palpitations and diarrhea this last week. Physical examination is unremarkable, except for a heart rate of 145/min. Basic thyroid function tests are shown in the table below. Which of the following additional laboratory tests would be most useful in assessing this patient's condition?
Thyroid-stimulating hormone (TSH)
0.28 mIU/L (0.3–4.5 mIU/L)
Total T4
12 µg/dL (5.4–11.5 µg/dL)
- A. Thyrotropin receptor antibodies (TRAb)
- B. Total triiodothyronine (T3) levels
- C. Thyroid peroxidase (TPO) antibodies
- D. Free thyroxine (T4) levels (Correct Answer)
- E. Thyroxine-binding globulin (TBG) levels
Regulation of thyroid function Explanation: ***Free thyroxine (T4) levels***
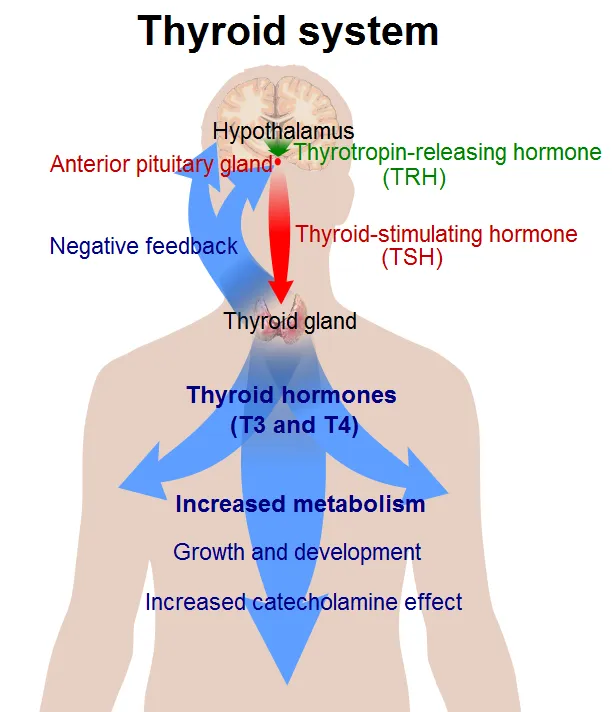
- In pregnancy, **estrogen increases thyroxine-binding globulin (TBG)**, leading to higher **total T4** levels even if free T4 is normal.
- Measuring **free T4 provides a more accurate assessment** of the biologically active thyroid hormone, which is crucial for distinguishing between physiological changes of pregnancy and true hyperthyroidism.
*Thyrotropin receptor antibodies (TRAb)*
- **TRAb are specific for Graves' disease**, which is a cause of hyperthyroidism, but their presence is a confirmatory test after hyperthyroidism has been established.
- The initial step is to confirm the diagnosis of **hyperthyroidism** by evaluating free hormone levels, particularly in pregnancy where total hormone levels are less reliable.
*Total triiodothyronine (T3) levels*
- Similar to total T4, **total T3 levels are also affected by increased TBG in pregnancy**, making them less reliable for initial diagnosis of thyroid dysfunction.
- While T3 is an important thyroid hormone, **free T4 is generally the primary screening test** for hyperthyroidism.
*Thyroid peroxidase (TPO) antibodies*
- **TPO antibodies are indicative of autoimmune thyroiditis**, such as Hashimoto's thyroiditis, which typically causes hypothyroidism, not hyperthyroidism, as suggested by the patient's symptoms and elevated T4.
- Although TPO antibodies can sometimes be positive in Graves' disease, they are **not the primary diagnostic test for active hyperthyroidism**, especially regarding the magnitude of the elevation.
*Thyroxine-binding globulin (TBG) levels*
- While **TBG levels are elevated in pregnancy**, measuring TBG itself doesn't directly assess thyroid function.
- Understanding the physiology of **TBG elevation explains why total T4 is high**, but it doesn't help in determining whether the patient is truly hyperthyroid; for that, free T4 is needed.
Regulation of thyroid function US Medical PG Question 3: A 49-year-old woman presents to the office because of tremors for 2 months. She says that her hands have been shaking a lot, especially when she feels stressed. In addition, she has been sweating more than usual and has lost 8 kg (17.6 lb) in the last 2 months. She has a past medical history of vitiligo. Her vital signs are a heart rate of 98/min, a respiratory rate of 14/min, a temperature of 37.6°C (99.7°F), and a blood pressure of 115/75 mm Hg. Physical examination shows a fine, bilateral hand tremor and a diffuse goiter. Which of the following hormonal imbalances is most likely present?
- A. Low TSH, high free T4, and high free T3 (Correct Answer)
- B. High TSH, high free T4, and high free T3
- C. High TSH, normal free T4, and normal free T3
- D. Low TSH, normal free T4, and normal free T3
- E. High TSH, low free T4, and low free T3
Regulation of thyroid function Explanation: ***Low TSH, high free T4, and high free T3***
- The patient's symptoms (tremors, sweating, weight loss, tachycardia, goiter) are classic for **hyperthyroidism**, which is typically characterized by **low TSH** due to negative feedback and **elevated free T4 and T3** levels.
- Her history of **vitiligo**, an autoimmune condition, further supports an autoimmune thyroid disorder like **Graves' disease**, a common cause of hyperthyroidism.
*High TSH, high free T4, and high free T3*
- This pattern would indicate **secondary hyperthyroidism**, caused by a TSH-secreting pituitary adenoma.
- While TSH would be high, it is a much rarer cause of hyperthyroidism compared to primary causes.
*High TSH, normal free T4, and normal free T3*
- This hormonal profile is characteristic of **subclinical hypothyroidism** or a **compensated primary hypothyroidism** early in its course.
- The patient's symptoms are inconsistent with hypothyroidism.
*Low TSH, normal free T4, and normal free T3*
- This suggests **subclinical hyperthyroidism**, where TSH is suppressed but thyroid hormone levels are still within the normal range.
- The patient's prominent and severe symptoms (tremors, significant weight loss, goiter) indicate overt hyperthyroidism, not subclinical disease.
*High TSH, low free T4, and low free T3*
- This is the classic hormonal profile for **primary hypothyroidism**, where the thyroid gland is failing to produce sufficient hormones, leading to elevated TSH.
- The patient's symptoms of nervousness, weight loss, and tremors are directly opposite to those seen in hypothyroidism.
Regulation of thyroid function US Medical PG Question 4: A 31-year-old woman presents to her primary care physician with a 2-week history of diarrhea. She says that she has also noticed that she is losing weight, which makes her feel anxious since she has relatives who have suffered from anorexia. Finally, she says that she is worried she has a fever because she feels warm and has been sweating profusely. On physical examination she is found to have proptosis, fine tremor of her hands, and symmetrical, non-tender thyroid enlargement. Which of the following types of enzymes is targeted by a treatment for this disease?
- A. Peroxidase (Correct Answer)
- B. Kinase
- C. Catalase
- D. Cyclooxygenase
- E. Phosphatase
Regulation of thyroid function Explanation: ***Peroxidase***
- The patient's symptoms (diarrhea, weight loss, anxiety, sweating, proptosis, fine tremor, and symmetrical thyroid enlargement) are classic for **Graves' disease**, a form of **hyperthyroidism**.
- **Thionamides** (e.g., propylthiouracil, methimazole) are a primary treatment for Graves' disease, and they work by inhibiting **thyroid peroxidase (TPO)**, an enzyme crucial for thyroid hormone synthesis.
*Kinase*
- **Kinases** are enzymes that catalyze the transfer of phosphate groups, often involved in signaling pathways. While kinases are important drug targets, they are not directly involved in the primary treatment mechanism for Graves' disease.
- Examples of kinase inhibitors include those used in cancer therapy, but not for hyperthyroidism's specific pathophysiology.
*Catalase*
- **Catalase** is an enzyme that catalyzes the decomposition of hydrogen peroxide into water and oxygen, protecting cells from oxidative damage.
- It has no direct role in the synthesis of thyroid hormones or as a target for hyperthyroidism treatment.
*Cyclooxygenase*
- **Cyclooxygenase (COX)** enzymes are involved in the synthesis of prostaglandins and thromboxanes, key mediators of inflammation and pain.
- COX inhibitors (like NSAIDs) are used for pain and inflammation, not for managing the hyperactive thyroid gland in Graves' disease.
*Phosphatase*
- **Phosphatases** are enzymes that remove phosphate groups from molecules. They play a role in various cellular processes but are not the primary target for drugs treating Graves' disease.
- While important in metabolic regulation, they are not directly inhibited by thionamide drugs used in hyperthyroidism.
Regulation of thyroid function US Medical PG Question 5: A 25-year-old man is rushed to the emergency department following a motor vehicle accident. After an initial evaluation, he is found to have bilateral femoral fractures. After surgical fixation of his fractures, he suddenly starts to feel nauseated and becomes agitated. Past medical history is significant for a thyroid disorder. His temperature is 40.0°C (104°F), blood pressure is 165/100 mm Hg, pulse is 170/min and irregularly irregular, and respirations are 20/min. On physical examination, the patient is confused and delirious. Oriented x 0. Laboratory studies are significant for the following:
Thyroxine (T4), free 5 ng/dL
Thyroid stimulating hormone (TSH) 0.001 mU/L
The patient is started on propranolol to control his current symptoms. Which of the following best describes the mechanism of action of this new medication?
- A. Inhibition of an underlying autoimmune process
- B. Interference with enterohepatic circulation and recycling of thyroid hormones
- C. Inhibition of release of thyroid hormones
- D. Inhibition of thyroid peroxidase enzyme
- E. Decrease the peripheral conversion of T4 to T3 (Correct Answer)
Regulation of thyroid function Explanation: ***Decrease the peripheral conversion of T4 to T3***
- **Propranolol**, a non-selective beta-blocker, plays a crucial role in thyroid storm management by **blocking beta-adrenergic receptors**, thereby mitigating the cardiovascular symptoms like tachycardia and hypertension.
- Furthermore, at high doses, propranolol directly **inhibits the peripheral conversion of T4 to T3**, which is the more biologically active thyroid hormone, thus reducing the overall thyroid hormone effect.
*Inhibition of an underlying autoimmune process*
- This mechanism describes drugs like **glucocorticoids** or **immunosuppressants**, which are effective in autoimmune thyroid diseases like Graves' disease but are not the primary mechanism of action for propranolol.
- While thyroid storm is often triggered by **Graves' disease**, initial management focuses on symptom control and blocking hormone effects, not primarily immune suppression by propranolol.
*Interference with enterohepatic circulation and recycling of thyroid hormones*
- This mechanism is characteristic of **cholestyramine** or **iodinated contrast agents**, which bind to thyroid hormones in the gut, preventing their reabsorption and increasing their fecal excretion.
- Propranolol does not significantly influence the enterohepatic circulation or recycling of thyroid hormones.
*Inhibition of release of thyroid hormones*
- This action is primarily achieved by **iodine preparations** (e.g., Lugol's iodine, potassium iodide) given after antithyroid drugs, which acutely block the release of preformed thyroid hormones from the gland.
- Although propranolol can reduce some aspects of sympathetic stimulation, it does not directly inhibit the release of thyroid hormones from the thyroid gland.
*Inhibition of thyroid peroxidase enzyme*
- This mechanism is specific to **thionamides** like **propylthiouracil (PTU)** and **methimazole**, which block the organification of iodine and coupling of iodotyrosines, thereby inhibiting thyroid hormone synthesis.
- Propranolol does not directly affect the thyroid peroxidase enzyme or thyroid hormone synthesis.
Regulation of thyroid function US Medical PG Question 6: A 43-year-old woman comes to the physician because of a 3-month history of tremor, diarrhea, and a 5-kg (11-lb) weight loss. Her pulse is 110/min. Examination shows protrusion of the eyeball when looking forward. A bruit is heard over the anterior neck on auscultation. Serum studies show autoantibodies to the thyroid-stimulating hormone receptor. The patient decides to undergo definitive treatment for her condition with a radioactive tracer. The success of this treatment directly depends on the activity of which of the following?
- A. Anion-oxidizing enzyme
- B. Transmembrane carrier (Correct Answer)
- C. Lysosomal protease
- D. Binding globulin
- E. Hormone-activating enzyme
Regulation of thyroid function Explanation: ***Transmembrane carrier***
- Radioactive iodine treatment relies on the uptake of iodine by thyroid follicular cells via the **sodium-iodide symporter (NIS)**, a **transmembrane carrier protein**.
- NIS actively transports iodide into thyroid cells, allowing the radioactive iodine to concentrate in the thyroid and destroy overactive tissue.
*Anion-oxidizing enzyme*
- This refers to **thyroid peroxidase (TPO)**, an enzyme that oxidizes iodide to iodine, incorporates iodine into thyroglobulin, and couples iodinated tyrosines.
- While essential for thyroid hormone synthesis, TPO's activity does not directly determine the success of **radioactive iodine uptake** for treatment.
*Lysosomal protease*
- **Lysosomal proteases** are involved in the breakdown of thyroglobulin to release thyroid hormones (T3 and T4) into circulation.
- They are important for the *release* of hormones but not for the *uptake* of iodine for radioactive treatment.
*Binding globulin*
- **Thyroxine-binding globulin (TBG)** is a plasma protein that transports thyroid hormones in the blood, maintaining a reservoir of T3 and T4.
- TBG's activity affects the availability of free thyroid hormones but has no direct role in the cellular uptake of radioactive iodine by the thyroid gland.
*Hormone-activating enzyme*
- This typically refers to deiodinases, enzymes that convert T4 (prohormone) into the more active T3 in peripheral tissues.
- These enzymes act *outside* the thyroid gland to activate hormones, and their activity does not directly influence the uptake of radioactive iodine.
Regulation of thyroid function US Medical PG Question 7: A 28-year-old woman, gravida 1, para 0, at 10 weeks gestation comes to the physician for her first prenatal visit. Today, she feels well. She has no history of serious illness. Her pulse is 75/min and blood pressure is 110/74 mm Hg. Examination shows no abnormalities. Ultrasonography shows a pregnancy consistent in size with a 10-week gestation. Serum studies in this patient are most likely to show which of the following sets of laboratory values?
$$$ Thyroid-binding globulin %%% Free Triiodothyronine (T3) %%% Free Thyroxine (T4) %%% Total T3+T4 $$$
- A. Normal ↑ ↑ ↑
- B. ↑ normal normal ↑ (Correct Answer)
- C. Normal normal normal normal
- D. ↓ normal normal ↓
- E. ↓ ↓ normal ↓
Regulation of thyroid function Explanation: ***↑ normal normal ↑***
- This option correctly reflects the typical changes in thyroid economy during pregnancy: **increased thyroid-binding globulin (TBG)** due to estrogen, leading to **increased total T3 and T4**, while **free T3 and free T4 remain normal** as the thyroid gland compensates.
- The elevated TBG binds more thyroid hormones, initially decreasing free hormone levels slightly, but the thyroid gland responds by producing more T3 and T4 to maintain **euthyroid** state with normal free hormone levels.
*Normal ↑ ↑ ↑*
- This option incorrectly suggests that **free T3 and free T4 would be elevated** along with total T3 and T4, which is not typical in a healthy pregnant woman.
- While total T3 and T4 increase, the body maintains **euthyroidism** by keeping free thyroid hormone levels within the normal range.
*Normal normal normal normal*
- This option incorrectly suggests that all thyroid parameters remain normal, which is not true for **TBG, total T3, and total T4** in pregnancy.
- The significant physiological changes during pregnancy, particularly the increase in **estrogen**, directly impact TBG levels and subsequently total thyroid hormone levels.
*↓ normal normal ↓*
- This option is incorrect as **TBG and total T3+T4 generally increase** during pregnancy, not decrease.
- A decrease in these values, especially with normal free hormones, is not consistent with the typical **euthyroid state** of a healthy pregnant woman.
*↓ ↓ normal ↓*
- This option incorrectly suggests a decrease in **TBG, free T3, and total T3+T4**, which would indicate a hypothyroid state, inconsistent with the patient's well-being and normal examination findings.
- A healthy pregnant woman maintains **euthyroidism** with normal free thyroid hormone levels.
Regulation of thyroid function US Medical PG Question 8: A 37-year-old man with a history of schizophrenia, obesity, anxiety, recurrent pneumonia, and depression is brought to the emergency department. He was recently discharged from inpatient psychiatric care where he was treated for an acute psychotic episode with fluphenazine and started on a new antidepressant. One week after discharge, during a period of cold weather, he is found outdoors confused and poorly dressed. His rectal temperature is 93.2°F (34°C). Which of the following medications is most likely contributing to his hypothermia?
- A. Fluphenazine (Correct Answer)
- B. Valproic acid
- C. Diphenhydramine
- D. Fluoxetine
- E. Lithium
Regulation of thyroid function Explanation: **Fluphenazine**
- **First-generation antipsychotics** like fluphenazine can impair the body's ability to **thermoregulate** by interfering with dopaminergic pathways in the hypothalamus, increasing susceptibility to hypothermia in cold environments.
- Given the patient's recent discharge from inpatient care and exposure to cold weather while poorly dressed, the addition of an antipsychotic affecting thermoregulation strongly contributes to his hypothermia.
*Valproic acid*
- Valproic acid is an **anticonvulsant** and **mood stabilizer** primarily used for bipolar disorder and epilepsy.
- While it can have various side effects, **hypothermia** is not a commonly reported or significant side effect of valproic acid.
*Diphenhydramine*
- Diphenhydramine is an **antihistamine** with significant **sedative** and **anticholinergic** properties.
- While it can cause sedation and anticholinergic effects that might impact a patient's awareness or ability to seek shelter, it is not directly implicated in causing hypothermia through thermoregulatory dysfunction.
*Fluoxetine*
- Fluoxetine is a **selective serotonin reuptake inhibitor (SSRI)** commonly used for depression and anxiety.
- While SSRIs can have various side effects, **hypothermia** is not a characteristic or significant side effect of fluoxetine.
*Lithium*
- Lithium is a **mood stabilizer** used primarily for bipolar disorder.
- **Hypothyroidism** is a known side effect of long-term lithium use, which could theoretically contribute to an inability to maintain body temperature, but it is less likely to cause acute hypothermia compared to antipsychotics directly affecting thermoregulation.
Regulation of thyroid function US Medical PG Question 9: A 27-year-old woman presents to her doctor complaining of pain in her neck that radiates to her left ear. The pain has been more or less constant for the last 3 weeks and increases when she chews and swallows. She was in her normal state of health before the pain started. She also mentions that she has been experiencing palpitations, muscle weakness, and increased sweating for the last 2 weeks. Past medical history is significant for a flu-like illness 2 months ago. She currently takes no medication and neither consumes alcohol nor smokes cigarettes. Her pulse is 104/min and irregular with a blood pressure of 140/80 mm Hg. On examination, the physician notices that the patient is restless. There is a presence of fine tremors in both hands. The anterior neck is swollen, warm to the touch, and markedly tender on palpation. Thyroid function tests and a biopsy are ordered. Which of the following deviations from the normal is expected to be seen in her thyroid function tests?
- A. Normal Serum TSH, ↑ Total T4, Normal Free T4, Normal I131 Uptake
- B. ↓ Serum TSH, ↑ Total T4, ↑ Free T4, ↑ I131 Uptake
- C. Normal Serum TSH, ↓ Total T4, Normal Free T4, Normal I131 Uptake
- D. ↑ Serum TSH, ↑ Total T4, ↑ Free T4, ↑ I 131 Uptake
- E. ↓ Serum TSH, ↑ Total T4, ↑ Free T4, ↓ I131 Uptake (Correct Answer)
Regulation of thyroid function Explanation: ***↓ Serum TSH, ↑ Total T4, ↑ Free T4, ↓ I131 Uptake***
- This pattern is characteristic of **thyrotoxicosis** (increased thyroid hormone levels) combined with decreased thyroid gland activity, which is typical for conditions like **subacute thyroiditis** (as suggested by the flu-like illness and painful, tender thyroid).
- The elevated **T3/T4** (Total and Free) results from the release of preformed hormones from the inflamed thyroid, while the **low TSH** is due to negative feedback. The **decreased I-131 uptake** indicates that the thyroid gland is not actively synthesizing new hormones.
*Normal Serum TSH, ↑ Total T4, Normal Free T4, Normal I131 Uptake*
- This combination is inconsistent with the patient's symptoms of hyperthyroidism (palpitations, sweating, tremors) and a **tender, swollen thyroid**.
- **Normal Free T4** and **Normal TSH** would suggest euthyroid status, which is not what the clinical presentation indicates.
*↓ Serum TSH, ↑ Total T4, ↑ Free T4, ↑ I131 Uptake*
- This pattern suggests a hyperthyroid state where the thyroid gland is actively overproducing hormones, as seen in **Graves' disease** or toxic nodular goiter.
- However, subacute thyroiditis is characterized by **low I-131 uptake** because the thyroid gland is damaged and releases preformed hormones rather than actively synthesizing new ones.
*Normal Serum TSH, ↓ Total T4, Normal Free T4, Normal I131 Uptake*
- This combination is not indicative of the patient's hyperthyroid symptoms (- **palpitations, muscle weakness, increased sweating**).
- **Normal Free T4** and **Normal TSH** would suggest euthyroid status, which is inconsistent with the clinical picture.
*↑ Serum TSH, ↑ Total T4, ↑ Free T4, ↑ I 131 Uptake*
- An **elevated TSH** would indicate **primary hypothyroidism**, where the thyroid gland is underactive, and the pituitary tries to stimulate it.
- This contradicts the patient's clinical signs of **hyperthyroidism** (palpitations, sweating, tremors) and the elevated Total and Free T4.
Regulation of thyroid function US Medical PG Question 10: A 38-year-old woman undergoes hemithyroidectomy for treatment of localized, well-differentiated papillary thyroid carcinoma. The lesion is removed with clear margins. However, during the surgery, a structure lying directly adjacent to the superior thyroid artery at the upper pole of the thyroid lobe is damaged. This patient is most likely to experience which of the following symptoms?
- A. Shortness of breath
- B. Weakness of shoulder shrug
- C. Voice pitch limitation (Correct Answer)
- D. Difficulty swallowing
- E. Ineffective cough
Regulation of thyroid function Explanation: ***Voice pitch limitation***
- Damage to the structure directly adjacent to the **superior thyroid artery** at the upper pole of the thyroid likely involves the **external branch of the superior laryngeal nerve (EBSLN)**.
- This nerve innervates the **cricothyroid muscle**, which is responsible for **tensing the vocal cords** and controlling **voice pitch**.
- Injury results in inability to change pitch, voice fatigue during prolonged speaking, and reduced vocal range.
*Shortness of breath*
- While damage to other nerves like the **recurrent laryngeal nerve** could cause vocal cord paralysis and potentially lead to airway compromise, this is less directly associated with the superior thyroid artery.
- Shortness of breath is not the specific consequence of EBSLN injury near the superior thyroid artery.
*Weakness of shoulder shrug*
- Weakness of shoulder shrug is associated with damage to the **spinal accessory nerve (cranial nerve XI)**, which innervates the **trapezius muscle**.
- This nerve is anatomically distinct from structures near the superior thyroid artery at the upper pole of the thyroid.
*Difficulty swallowing*
- Difficulty swallowing (dysphagia) can result from damage to the **vagus nerve (cranial nerve X)** or its pharyngeal branches, but it is not the direct consequence of injury near the superior thyroid artery.
- Damage to the EBSLN primarily affects voice pitch and quality, not swallowing.
*Ineffective cough*
- An ineffective cough results from paralysis of the vocal cords (preventing glottic closure) or weakness of respiratory muscles, typically from **recurrent laryngeal nerve** damage or phrenic nerve injury.
- EBSLN damage primarily affects voice pitch and does not significantly impair cough effectiveness.
More Regulation of thyroid function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.