Pancreatic endocrine function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pancreatic endocrine function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pancreatic endocrine function US Medical PG Question 1: A 41-year-old female complains of frequent diarrhea and abdominal pain between meals. Endoscopy reveals a duodenal ulcer distal to the duodenal bulb. CT scan of the abdomen demonstrates a pancreatic mass, and subsequent tissue biopsy of the pancreas reveals a malignant islet cell tumor. Which of the following hormones is likely to be markedly elevated in this patient:
- A. Secretin
- B. Vasoactive intestinal peptide
- C. Cholecystokinin
- D. Gastrin (Correct Answer)
- E. Motilin
Pancreatic endocrine function Explanation: ***Gastrin***
- A pancreatic mass (likely a **gastrinoma**) producing excess **gastrin** leads to Zollinger-Ellison syndrome, characterized by refractory **peptic ulcers** (especially distal to the duodenal bulb) and **diarrhea** due to increased gastric acid.
- The high gastrin levels stimulate parietal cells to secrete an excessive amount of **hydrochloric acid**, overwhelming the neutralizing capacity of the duodenum and causing ulcers.
*Secretin*
- Secretin is released from S cells in the duodenum in response to acid and fatty acids, stimulating **bicarbonate secretion** from the pancreas and bile ducts.
- While secretin can be used diagnostically to confirm gastrinoma (paradoxical increase in gastrin), it is not the primary hormone elevated in this syndrome causing the symptoms.
*Vasoactive intestinal peptide*
- Elevated vasoactive intestinal peptide (VIP) is characteristic of a **VIPoma**, which causes **profuse watery diarrhea** (pancreatic cholera), hypokalemia, and achlorhydria.
- This patient's symptoms include abdominal pain and duodenal ulcers which are not typical for a VIPoma.
*Cholecystokinin*
- **Cholecystokinin (CCK)** is primarily involved in stimulating gallbladder contraction and pancreatic enzyme secretion in response to fats and proteins.
- While it can be produced by some neuroendocrine tumors, it does not typically cause the constellation of symptoms (refractory duodenal ulcers, severe diarrhea) seen in this patient.
*Motilin*
- Motilin is responsible for initiating the **migrating motor complex** during the interdigestive phase, promoting gut motility.
- While altered motility can contribute to diarrhea, motilin is not typically associated with ulcer formation or pancreatic islet cell tumors causing gastric hypersecretion.
Pancreatic endocrine function US Medical PG Question 2: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Pancreatic endocrine function Explanation: ***Papilledema***
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Pancreatic endocrine function US Medical PG Question 3: A 24-year-old man presents for an annual check-up. He is a bodybuilder and tells you he is on a protein-rich diet that only allows for minimal carbohydrate intake. His friend suggests he try exogenous glucagon to help him lose some excess weight before an upcoming competition. Which of the following effects of glucagon is he attempting to exploit?
- A. Increased glucose utilization by tissues
- B. Decreased blood cholesterol level
- C. Increased hepatic gluconeogenesis
- D. Increased lipolysis in adipose tissues (Correct Answer)
- E. Increased hepatic glycogenolysis
Pancreatic endocrine function Explanation: ***Increased lipolysis in adipose tissues***
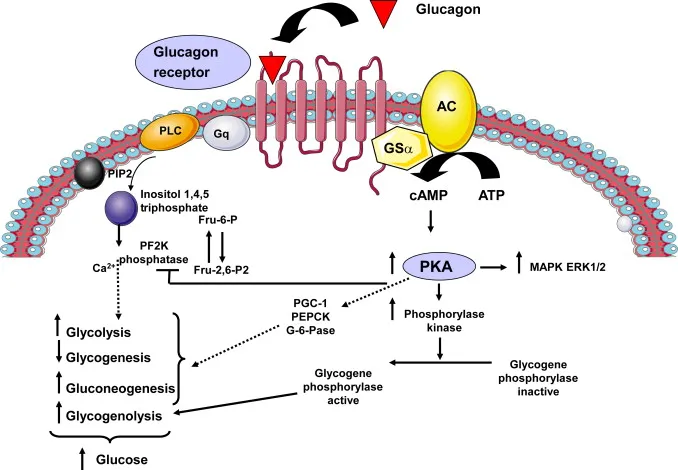
- While **glucagon's primary target is the liver**, it can have **modest lipolytic effects** on adipose tissue by opposing insulin's anti-lipolytic actions.
- Glucagon stimulates cAMP production, which can activate **hormone-sensitive lipase** to break down triglycerides into **fatty acids** and **glycerol**.
- However, **catecholamines (epinephrine/norepinephrine)** are far more potent direct stimulators of adipose tissue lipolysis than glucagon.
- The friend is attempting to exploit this lipolytic effect for fat loss, though **exogenous glucagon is not an evidence-based or safe weight-loss strategy**.
*Increased glucose utilization by tissues*
- This is **opposite** to glucagon's actual effect. **Glucagon raises blood glucose** levels; it does not promote glucose uptake by peripheral tissues.
- **Insulin** is the hormone responsible for promoting glucose uptake and utilization by muscle, adipose, and other tissues.
*Decreased blood cholesterol level*
- Glucagon does not have a direct, clinically significant effect on reducing blood cholesterol levels.
- While glucagon affects overall lipid metabolism through its catabolic actions, it is not used therapeutically for hypercholesterolemia.
*Increased hepatic gluconeogenesis*
- **Glucagon strongly stimulates hepatic gluconeogenesis**, which is the synthesis of glucose from non-carbohydrate precursors (amino acids, lactate, glycerol) in the liver.
- This action **raises blood glucose** levels and would not directly contribute to fat loss or weight reduction.
- In the context of a low-carbohydrate diet, increased gluconeogenesis would maintain blood glucose but not promote the fat loss the bodybuilder seeks.
*Increased hepatic glycogenolysis*
- **Glucagon is a potent stimulator of hepatic glycogenolysis**, the breakdown of stored liver glycogen into glucose.
- This rapidly increases blood glucose levels during fasting or hypoglycemia.
- However, this does not directly target adipose tissue for fat loss; it mobilizes glucose stores rather than fat stores, so it's not the mechanism relevant to weight loss goals.
Pancreatic endocrine function US Medical PG Question 4: A 45-year-old woman comes to the emergency department with recurrent episodes of shaking, sweating, and palpitations. The patient is confused and complains of hunger. One week ago, she had similar symptoms that improved after eating. She has hypertension and a history of biliary pancreatitis. She underwent cholecystectomy 1 year ago. She works as a nurse aide in a nursing care facility. She does not smoke or drink alcohol. She does not exercise. Her temperature is 36.7°C (98°F), pulse is 104/min, respirations are 20/min, and blood pressure is 135/88 mm Hg. Examination shows tremors and diaphoresis. Laboratory studies show:
Blood glucose 50 mg/dL
Thyroid-stimulating hormone 1 mU/L
C-peptide 0.50 ng/mL (N=0.8–3.1)
Abdominal ultrasound reveals a 1-cm anechoic lesion in the head of the pancreas. Which of the following is the most likely cause of this patient's symptoms?
- A. Pancreatic neoplasm
- B. Pancreatic pseudocyst
- C. Graves' disease
- D. Surreptitious insulin use (Correct Answer)
- E. Type 1 diabetes mellitus
Pancreatic endocrine function Explanation: ***Surreptitious insulin use***
- The patient's symptoms of **hypoglycemia** (shaking, sweating, palpitations, confusion, hunger) combined with a **low C-peptide level** (0.50 ng/mL) and a normal TSH strongly suggest **exogenous insulin administration**.
- As a nurse aide, she has access to insulin, and the normal pancreatic ultrasound (1 cm anechoic lesion is non-specific and unlikely to cause these symptoms) rules out an **insulinoma**, which would present with high C-peptide.
*Pancreatic neoplasm*
- While a pancreatic neoplasm can cause various symptoms, an **insulinoma** (a type of pancreatic neuroendocrine tumor) would present with **hypoglycemia** but typically with **elevated C-peptide levels**, as it produces endogenous insulin.
- The ultrasound finding of a 1-cm anechoic lesion is **non-specific** and not definitively indicative of an insulinoma or any other functional neoplasm causing these specific symptoms.
*Pancreatic pseudocyst*
- Pancreatic pseudocysts are collections of fluid that can occur after **pancreatitis** or trauma, and while this patient has a history of biliary pancreatitis, pseudocysts generally cause symptoms like **abdominal pain, distension, and early satiety**, not hypoglycemia.
- They also do not explain the **low C-peptide** and recurrent episodes of neuroglycopenic symptoms.
*Graves' disease*
- Graves' disease is an **autoimmune hyperthyroid condition** that causes symptoms like palpitations, sweating, and tremors, but it is characterized by **low TSH** with elevated free T3/T4 due to negative feedback, not hypoglycemia or low C-peptide.
- The patient's **normal TSH** (1 mU/L) rules out Graves' disease as the cause of her current symptoms.
*Type 1 diabetes mellitus*
- Type 1 diabetes is characterized by **insulin deficiency** due to autoimmune destruction of pancreatic beta cells, leading to **hyperglycemia**, not hypoglycemia.
- While patients with type 1 diabetes may experience hypoglycemia if they administer too much insulin, the underlying disease itself causes high blood glucose, and the C-peptide would be very low or undetectable in a new diagnosis, but not as the cause of recurrent spontaneous hypoglycemia.
Pancreatic endocrine function US Medical PG Question 5: A 60-year-old African-American female presents to your office complaining of dysuria, paresthesias, and blurry vision. Her body mass index is 37.2 kg/m2. Which of the following drugs would most significantly increase the levels of C-peptide in the blood when administered to this patient?
- A. Acarbose
- B. Glipizide (Correct Answer)
- C. Insulin
- D. Metformin
- E. NPH
Pancreatic endocrine function Explanation: ***Glipizide***
- **Glipizide** is a **sulfonylurea** that stimulates insulin secretion from pancreatic beta cells, leading to increased C-peptide levels.
- Increased insulin secretion by glipizide is independent of meals and can cause **hypoglycemia**.
*Acarbose*
- **Acarbose** is an **alpha-glucosidase inhibitor** that delays glucose absorption from the gut, reducing post-prandial glucose spikes.
- It does not directly affect insulin secretion or C-peptide levels.
*Insulin*
- Administering exogenous **insulin** directly lowers blood glucose but does not stimulate endogenous insulin production, and therefore does not increase C-peptide.
- C-peptide is a marker of endogenous insulin secretion; an increase would only be seen if the body produced more insulin.
*Metformin*
- **Metformin** primarily reduces **hepatic glucose production** and improves insulin sensitivity in peripheral tissues.
- It does not directly stimulate insulin secretion from the pancreas and therefore does not increase C-peptide levels.
*NPH*
- **NPH (Neutral Protamine Hagedorn)** is an intermediate-acting exogenous insulin formulation.
- As an exogenous insulin, it does not stimulate the pancreas to produce more insulin or C-peptide.
Pancreatic endocrine function US Medical PG Question 6: Pancreatic islets were isolated from a healthy, non-diabetic donor to perform an experiment to look at insulin secretion inhibition. Compounds would be added to separate wells containing the islets bathed in a high glucose solution for one hour. After one hour, the supernatant would be collected, and the insulin content would be measured with an enzyme-linked immunosorbent assay (ELISA). Which of the following compounds would result in the least insulin secretion when added to the islets?
- A. Isoproterenol
- B. Dobutamine
- C. Glyburide
- D. Tolbutamide
- E. Clonidine (Correct Answer)
Pancreatic endocrine function Explanation: ***Clonidine***
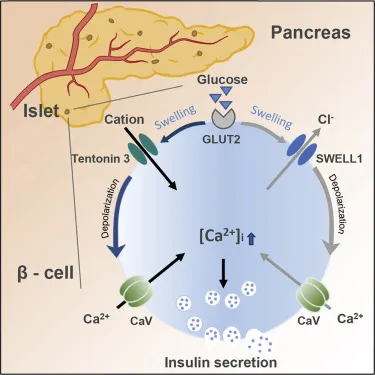
- Clonidine is an **alpha-2 adrenergic agonist**, which acts to inhibit insulin secretion from pancreatic beta cells. Alpha-2 receptors, when activated, reduce intracellular cAMP levels, thereby **suppressing insulin release**.
- In a high glucose environment, this inhibitory action of clonidine would result in the **least insulin secretion** compared to other listed compounds which either stimulate insulin secretion or have less direct inhibitory effects.
*Isoproterenol*
- Isoproterenol is a **non-selective beta-adrenergic agonist** (β1 and β2). Activation of beta-adrenergic receptors on pancreatic beta cells generally **stimulates insulin secretion** by increasing intracellular cAMP.
- Therefore, adding isoproterenol would lead to **increased insulin release**, not decreased.
*Dobutamine*
- Dobutamine is primarily a **beta-1 adrenergic agonist**, though it has some beta-2 effects. Beta-1 activation on pancreatic cells is not the primary mechanism associated with insulin regulation.
- While it may have some minor impact, its main action is on cardiac contractility and it is **not known to significantly inhibit insulin secretion** from beta cells.
*Glyburide*
- Glyburide is a **sulfonylurea drug** that works by binding to the SUR1 subunit of the **ATP-sensitive potassium (KATP) channel** on pancreatic beta cells, thereby closing it.
- This closure leads to **depolarization of the cell membrane**, calcium influx, and ultimately **increased insulin secretion**.
*Tolbutamide*
- Tolbutamide is another **sulfonylurea drug**, similar to glyburide, that acts by binding to and blocking the **ATP-sensitive potassium (KATP) channels** on pancreatic beta cells.
- This mechanism leads to beta cell depolarization, **calcium entry**, and **stimulation of insulin release**.
Pancreatic endocrine function US Medical PG Question 7: A 16-year-old girl is brought to the emergency department unresponsive. A witness reports that she became anxious, lightheaded, and began sweating and trembling a few minutes before she lost consciousness. Her vitals are as follows: blood pressure 95/60 mm Hg, heart rate 110/min, respiratory rate 21/min, and temperature 35.5°C (95.5°F). She becomes responsive but is still somnolent. She complains of dizziness and weakness. A more detailed history reveals that she has drastically restricted her diet to lose weight for the past 18 hours, and has not eaten today. Her skin is pale, wet, and cold. The rest of the physical examination is unremarkable. Blood testing shows a plasma glucose level of 2.8 mmol/L (50.5 mg/dL). Which of the following statements is true?
- A. Hypoglycemia in this patient is being compensated with an increased glycogenolysis rate. (Correct Answer)
- B. Epinephrine-induced gluconeogenesis is the main process that allows for the compensation of a decreased glucose level.
- C. There is an increase in the glycogen synthesis rate in this patient’s hepatocytes.
- D. The patient’s symptoms are most likely the consequence of increased insulin secretion from the pancreatic islets.
- E. The patient’s hypoglycemia inhibits glucagon release from pancreatic alpha cells.
Pancreatic endocrine function Explanation: ***Hypoglycemia in this patient is being compensated with an increased glycogenolysis rate.***
- The patient's symptoms (anxiety, sweating, trembling, dizziness, weakness) and **low blood glucose (2.8 mmol/L)** confirm hypoglycemia. The immediate physiological response to hypoglycemia is the release of counter-regulatory hormones (glucagon, epinephrine, cortisol, growth hormone) which stimulate **glycogenolysis** (breakdown of glycogen to glucose) in the liver to maintain blood glucose, especially in the initial hours of fasting.
- Given that she has only fasted for 18 hours, her **hepatic glycogen stores** would still be recruited to provide glucose, making increased glycogenolysis a primary compensatory mechanism before gluconeogenesis becomes dominant.
*Epinephrine-induced gluconeogenesis is the main process that allows for the compensation of a decreased glucose level.*
- While epinephrine promotes **gluconeogenesis**, it is not the *main* compensatory process in the *initial* stages of fasting (0-24 hours). **Glycogenolysis** is the primary response in the first few hours.
- Gluconeogenesis becomes the predominant source of glucose after glycogen stores are significantly depleted, typically after 24 hours of fasting or longer.
*There is an increase in the glycogen synthesis rate in this patient’s hepatocytes.*
- **Glycogen synthesis (glycogenesis)** occurs when blood glucose levels are high, typically after a meal, to store excess glucose as glycogen.
- In a state of hypoglycemia, the liver's priority is to *release* glucose, meaning **glycogenolysis** is increased, and glycogen synthesis is inhibited.
*The patient’s symptoms are most likely the consequence of increased insulin secretion from the pancreatic islets.*
- **Increased insulin secretion** would *cause* hypoglycemia, not be a consequence. In response to hypoglycemia, insulin secretion is *reduced* to prevent further lowering of blood glucose.
- The symptoms described (anxiety, sweating, trembling) are characteristic of the **adrenergic response** to hypoglycemia, mediated by epinephrine and norepinephrine, which are counter-regulatory hormones.
*The patient’s hypoglycemia inhibits glucagon release from pancreatic alpha cells.*
- **Hypoglycemia** is a strong stimulant for **glucagon release** from pancreatic alpha cells. Glucagon's primary role is to raise blood glucose levels by promoting hepatic glycogenolysis and gluconeogenesis.
- Therefore, glucagon release would be *stimulated*, not inhibited, in this patient's condition.
Pancreatic endocrine function US Medical PG Question 8: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Pancreatic endocrine function Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Pancreatic endocrine function US Medical PG Question 9: Certain glucose transporters that are expressed predominantly on skeletal muscle cells and adipocytes are unique compared to those transporters found on other cell types within the body. Without directly affecting glucose transport in other cell types, which of the following would be most likely to selectively increase glucose uptake in skeletal muscle cells and adipocytes?
- A. Increased plasma glucose concentration
- B. It is physiologically impossible to selectively increase glucose uptake in specific cells
- C. Increased levels of circulating insulin (Correct Answer)
- D. Decreased plasma glucose concentration
- E. Decreased levels of circulating insulin
Pancreatic endocrine function Explanation: ***Increased levels of circulating insulin***
- Insulin stimulates the translocation of **GLUT4 transporters** from intracellular vesicles to the cell membrane in **skeletal muscle** and **adipocytes**, thereby increasing glucose uptake.
- This mechanism is **selective** because other cell types (e.g., brain, liver) primarily use insulin-independent glucose transporters (e.g., GLUT1, GLUT2, GLUT3) that are constitutively active or respond to different signals.
*Increased plasma glucose concentration*
- While increased glucose concentration would drive glucose uptake in many cells, it is not **selective** for skeletal muscle and adipocytes since other cells also take up glucose.
- Insulin-independent tissues would also increase glucose uptake, making this a non-specific effect.
*It is physiologically impossible to selectively increase glucose uptake in specific cells*
- This statement is incorrect because the body has mechanisms, such as **insulin-mediated GLUT4 translocation**, that specifically regulate glucose uptake in certain cell types like skeletal muscle and adipocytes.
- This regulatory specificity is crucial for maintaining **glucose homeostasis**.
*Decreased plasma glucose concentration*
- A decrease in plasma glucose would generally **reduce** glucose uptake across all cell types, including skeletal muscle and adipocytes.
- It would not selectively increase uptake in any specific cell population.
*Decreased levels of circulating insulin*
- Decreased insulin levels would lead to **reduced** glucose uptake in insulin-sensitive tissues like skeletal muscle and adipocytes, as GLUT4 transporters would remain sequestered intracellularly.
- This would result in higher circulating glucose levels rather than increased uptake.
Pancreatic endocrine function US Medical PG Question 10: A 38-year-old female presents to her primary care physician with complaints of several episodes of palpitations accompanied by panic attacks over the last month. She also is concerned about many instances over the past few weeks where food has been getting stuck in her throat and she has had trouble swallowing. She denies any prior medical problems and reports a family history of cancer in her mother and maternal grandfather but cannot recall any details regarding the type of cancer(s) or age of diagnosis. Her vital signs at today's visit are as follows: T 37.6 deg C, HR 106, BP 158/104, RR 16, SpO2 97%. Physical examination is significant for a nodule on the anterior portion of the neck that moves with swallowing, accompanied by mild lymphadenopathy. A preliminary work-up is initiated, which shows hypercalcemia, elevated baseline calcitonin, and an inappropriately elevated PTH level. Diagnostic imaging shows bilateral adrenal lesions on an MRI of the abdomen/pelvis. Which of the following is the most likely diagnosis in this patient?
- A. Familial medullary thyroid cancer (FMTC)
- B. Li-Fraumeni syndrome
- C. Multiple endocrine neoplasia (MEN) IIa (Correct Answer)
- D. Multiple endocrine neoplasia (MEN) I
- E. Multiple endocrine neoplasia (MEN) IIb
Pancreatic endocrine function Explanation: ***Multiple endocrine neoplasia (MEN) IIa***
- This patient presents with **medullary thyroid cancer** (due to the thyroid nodule, elevated calcitonin, and family history of cancer), **pheochromocytoma** (indicated by palpitations, panic attacks, hypertension, and adrenal lesions), and **primary hyperparathyroidism** (evidenced by hypercalcemia and inappropriately elevated PTH). These three conditions are the classic triad of MEN IIa.
- The symptoms of food getting stuck in her throat are also consistent with the presence of a **thyroid nodule**.
*Familial medullary thyroid cancer (FMTC)*
- While the patient has **medullary thyroid cancer**, FMTC is typically characterized solely by medullary thyroid carcinoma without the associated pheochromocytoma or primary hyperparathyroidism seen in this case.
- This patient's presentation includes **adrenal lesions** and **hyperparathyroidism**, which are not features of isolated FMTC.
*Li-Fraumeni syndrome*
- This syndrome is associated with a high risk of various cancers, including sarcomas, breast cancer, brain tumors, and adrenocortical carcinoma, but it is not typically associated with **medullary thyroid cancer, pheochromocytoma, or primary hyperparathyroidism** as a primary presentation.
- The genetic basis is a mutation in the **TP53 gene**, and the clinical picture does not match the specific endocrine tumors observed here.
*Multiple endocrine neoplasia (MEN) I*
- MEN I is characterized by tumors of the **parathyroid, pituitary, and pancreas** (the 3 Ps).
- This patient's presentation of medullary thyroid cancer, pheochromocytoma, and primary hyperparathyroidism does not include pituitary or pancreatic tumors, and medullary thyroid cancer and pheochromocytoma are not part of the MEN I spectrum.
*Multiple endocrine neoplasia (MEN) IIb*
- MEN IIb includes **medullary thyroid cancer** and **pheochromocytoma**, which are present in this patient.
- However, MEN IIb also classically presents with characteristic **mucosal neuromas** and a **marfanoid habitus**, and *lacks* primary hyperparathyroidism, which this patient clearly exhibits.
More Pancreatic endocrine function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.