Mineralocorticoid actions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mineralocorticoid actions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mineralocorticoid actions US Medical PG Question 1: A 32-year-old woman comes to the physician because of a 2-month history of fatigue, muscle weakness, paresthesias, headache, and palpitations. Her pulse is 75/min and blood pressure is 152/94 mm Hg. Physical examination shows no abnormalities. Serum studies show:
Sodium 144 mEq/L
Potassium 2.9 mEq/L
Bicarbonate 31 mEq/L
Creatinine 0.7 mg/dL
Further evaluation shows low serum renin activity. Which of the following is the most likely diagnosis?
- A. Aldosteronoma (Correct Answer)
- B. Cushing syndrome
- C. Renal artery stenosis
- D. Pheochromocytoma
- E. Laxative abuse
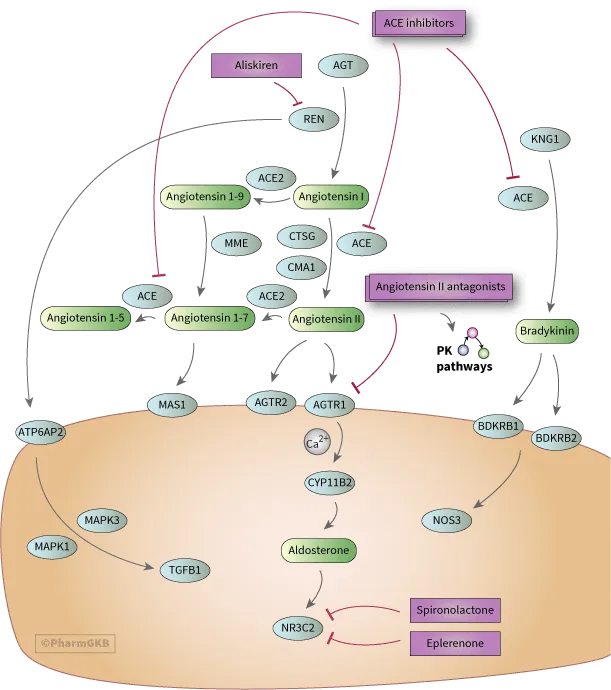
Mineralocorticoid actions Explanation: ***Aldosteronoma***
- The patient presents with **hypertension**, **hypokalemia**, and **metabolic alkalosis** (elevated bicarbonate), which are classic signs of primary hyperaldosteronism.
- **Low serum renin activity** in conjunction with these findings points directly to an **aldosterone-producing adenoma (aldosteronoma)** as the most likely cause.
*Cushing syndrome*
- While Cushing syndrome can cause **hypertension** and **hypokalemia**, it is primarily characterized by features of **hypercortisolism** such as central obesity, moon facies, striae, and muscle wasting, which are not described here.
- The primary defect in Cushing syndrome relates to cortisol excess, not primary aldosterone overproduction leading to low renin.
*Renal artery stenosis*
- **Renal artery stenosis** causes **secondary hyperaldosteronism**, typically presenting with **hypertension** and **elevated renin activity** due to decreased renal perfusion.
- This contradicts the patient's low serum renin activity, making it an unlikely diagnosis.
*Pheochromocytoma*
- **Pheochromocytoma** presents with paroxysmal or sustained **hypertension**, **palpitations**, **headaches**, and **sweating** due to catecholamine excess.
- It does not typically cause **hypokalemia** or **metabolic alkalosis** as seen in this patient.
*Laxative abuse*
- **Laxative abuse** can cause hypokalemia and metabolic alkalosis, but it is typically associated with **chronic diarrhea** and volume depletion, which are not mentioned.
- It does not directly cause **hypertension** and is not associated with low renin activity in the context of aldosterone excess.
Mineralocorticoid actions US Medical PG Question 2: A 33-year-old woman presents to her primary care physician for a wellness check-up. She states that recently she has been feeling well other than headaches that occur occasionally, which improve with ibuprofen and rest. She has a past medical history of hypertension and headaches and is currently taking hydrochlorothiazide. Her temperature is 99.2°F (37.3°C), blood pressure is 157/108 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals a young woman who appears healthy. A normal S1 and S2 are auscultated on cardiac exam, and her lungs are clear with good air movement bilaterally. From her previous visit, it was determined that she has an elevated aldosterone and low renin level. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 3.7 mEq/L
HCO3-: 29 mEq/L
BUN: 20 mg/dL
Creatinine: 1.1 mg/dL
Which of the following is the most likely diagnosis?
- A. Benign essential hypertension
- B. Pheochromocytoma
- C. Cushing syndrome
- D. Narrowing of the renal arteries
- E. Primary hyperaldosteronism (Correct Answer)
Mineralocorticoid actions Explanation: ***Primary hyperaldosteronism***
- The patient presents with **hypertension**, **mild hypokalemia (K+ of 3.7 mEq/L)**, and **metabolic alkalosis (HCO3- of 29 mEq/L)**, which are classic signs of primary hyperaldosteronism.
- The elevated aldosterone and low renin levels, as noted from her previous visit, are diagnostic for primary hyperaldosteronism.
*Benign essential hypertension*
- While essential hypertension is common, the presence of **hypokalemia**, **metabolic alkalosis**, and particularly the **elevated aldosterone with low renin** points away from benign essential hypertension, which typically has normal renin-aldosterone ratios.
- This patient's hypertension is likely **secondary** due to a specific endocrine imbalance.
*Pheochromocytoma*
- This condition presents with **episodic or paroxysmal hypertension**, **tachycardia**, **sweating**, and headaches, often in a more dramatic fashion.
- The patient's blood pressure is consistently elevated, and she lacks the typical paroxysmal symptoms and signs of catecholamine excess.
*Cushing syndrome*
- Cushing syndrome is characterized by **hypertension**, central obesity, moon facies, buffalo hump, and striae, none of which are described.
- While it can cause hypertension, it is due to cortisol excess and does not typically present with the specific aldosterone-renin profile seen in this patient.
*Narrowing of the renal arteries*
- **Renal artery stenosis** causes **renovascular hypertension** and is associated with **elevated renin levels** as the kidney perceives hypoperfusion and activates the renin-angiotensin-aldosterone system.
- This patient presents with **low renin levels**, which directly contradicts the pathophysiology of renal artery stenosis.
Mineralocorticoid actions US Medical PG Question 3: A 42-year-old man is brought to the emergency room because of confusion. His wife says he has been urinating more frequently than usual for the past 3 days. He has not had fever or dysuria. He has bipolar disorder, for which he takes lithium. His pulse is 105/min, and respirations are 14/min. He is lethargic and oriented only to person. Physical examination shows dry mucous membranes and increased capillary refill time. Laboratory studies show a serum sodium concentration of 158 mEq/L and an antidiuretic hormone (ADH) concentration of 8 pg/mL (N = 1–5). Which of the following is the most likely site of dysfunction in this patient?
- A. Hypothalamic supraoptic nucleus
- B. Descending loop of Henle
- C. Juxtaglomerular apparatus
- D. Collecting duct (Correct Answer)
- E. Posterior pituitary gland
Mineralocorticoid actions Explanation: ***Collecting duct***
- The patient presents with **hypernatremia** (Na 158 mEq/L), **polyuria**, and **dehydration** (dry mucous membranes, increased capillary refill time, confusion), indicative of **nephrogenic diabetes insipidus**.
- His ADH level is **elevated** (8 pg/mL), suggesting that the kidneys are not responding to ADH; the **collecting ducts** are the primary site where ADH exerts its effect via aquaporin-2 channels to reabsorb water.
- **Lithium**, which this patient is taking for bipolar disorder, is a well-known cause of nephrogenic diabetes insipidus by interfering with ADH action at the collecting duct level.
*Hypothalamic supraoptic nucleus*
- This nucleus is responsible for synthesizing **ADH**. Dysfunction here would lead to **decreased ADH production** (central diabetes insipidus), but the patient's ADH level is elevated.
- A lack of ADH from this area would not explain the kidney's unresponsiveness to the high ADH levels observed.
*Descending loop of Henle*
- The descending loop of Henle is permeable to water but not directly responsible for ADH-mediated water reabsorption that is impaired in diabetes insipidus.
- Its primary role is to concentrate the filtrate as it descends into the hypertonic medulla.
*Juxtaglomerular apparatus*
- The juxtaglomerular apparatus regulates **blood pressure** and **glomerular filtration rate** through the **renin-angiotensin-aldosterone system**.
- While important for kidney function, it's not directly involved in the ADH-mediated water reabsorption whose impairment leads to nephrogenic diabetes insipidus.
*Posterior pituitary gland*
- This gland stores and releases ADH, which is synthesized in the hypothalamus.
- If the posterior pituitary were dysfunctional, it would lead to **decreased ADH release** (central diabetes insipidus), contradicting the patient's **elevated ADH level**.
Mineralocorticoid actions US Medical PG Question 4: A new drug has been shown to block epithelial sodium channels in the cortical collecting duct. Which of the following is most likely to be decreased upon drug administration?
- A. Urea reabsorption in the collecting tubules
- B. Hydrogen ion secretion in the collecting tubules
- C. Potassium secretion in the collecting tubules (Correct Answer)
- D. Sodium secretion in the collecting tubules
- E. Sodium chloride reabsorption in the distal tubule
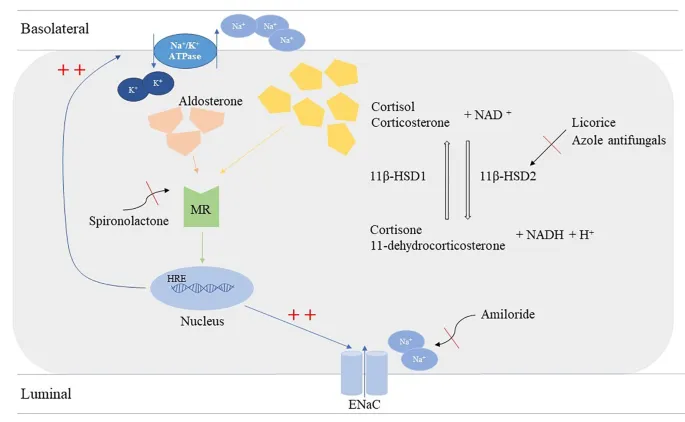
Mineralocorticoid actions Explanation: ***Potassium secretion in the collecting tubules***
- Blocking **epithelial sodium channels (ENaC)** in the cortical collecting duct reduces sodium reabsorption, which in turn diminishes the electrochemical gradient driving **potassium secretion** into the lumen.
- This is because sodium reabsorption creates a more negative luminal charge, attracting potassium ions to move from the cell into the tubule.
- This is the mechanism of **potassium-sparing diuretics** like amiloride and triamterene.
*Urea reabsorption in the collecting tubules*
- Urea **reabsorption** primarily occurs in the **medullary collecting duct** via urea transporters (UT-A1, UT-A3) and is influenced by the inner medullary osmolarity and ADH.
- Blocking ENaC would primarily affect sodium flux and potassium secretion, with minimal direct impact on urea reabsorption in the collecting duct.
*Hydrogen ion secretion in the collecting tubules*
- **Hydrogen ion (H+) secretion** occurs in the collecting tubules via intercalated cells (α-intercalated cells), which is important for acid-base balance.
- While blocking ENaC can indirectly reduce H+ secretion (by decreasing the lumen-negative potential), the primary and most significant effect is on **potassium secretion**, making this a less likely answer.
*Sodium secretion in the collecting tubules*
- The primary function of ENaC is to **reabsorb sodium** from the tubular lumen back into the blood, not to secrete it.
- Sodium is not normally secreted in the collecting tubules; blocking ENaC would decrease sodium **reabsorption**, not affect sodium secretion.
*Sodium chloride reabsorption in the distal tubule*
- **Sodium chloride reabsorption** in the distal convoluted tubule is mainly mediated by the **thiazide-sensitive Na-Cl co-transporter (NCC)**.
- ENaC are predominantly located in the cortical collecting duct (downstream from the DCT), so blocking them would not directly impact NaCl reabsorption in the distal tubule.
Mineralocorticoid actions US Medical PG Question 5: A new drug X is being tested for its effect on renal function. During the experiments, the researchers found that in patients taking substance X, the urinary concentration of sodium decreases while urine potassium concentration increase. Which of the following affects the kidneys in the same way as does substance X?
- A. Aldosterone (Correct Answer)
- B. Furosemide
- C. Spironolactone
- D. Atrial natriuretic peptide
- E. Hydrochlorothiazide
Mineralocorticoid actions Explanation: ***Aldosterone***
- **Aldosterone** acts on the **principal cells** of the **collecting duct** to increase sodium reabsorption and potassium secretion.
- This action leads to a decrease in urinary sodium concentration and an increase in urinary potassium concentration, matching the effects of drug X.
*Furosemide*
- **Furosemide** is a **loop diuretic** that inhibits the **Na-K-2Cl cotransporter** in the **thick ascending limb** of the loop of Henle.
- This inhibition leads to increased excretion of sodium, potassium, and water, resulting in higher urinary sodium concentration.
*Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that blocks aldosterone's effects on the collecting duct.
- This leads to increased sodium excretion and decreased potassium excretion (potassium-sparing effect), which is the opposite of drug X.
*Atrial natriuretic peptide*
- **Atrial natriuretic peptide (ANP)** is released in response to atrial stretch and causes **natriuresis** (increased sodium excretion) and **diuresis**.
- It works by dilating afferent arterioles and constricting efferent arterioles, increasing GFR, and inhibiting sodium reabsorption, thus increasing urinary sodium concentration.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic** that inhibits the **Na-Cl cotransporter** in the **distal convoluted tubule**.
- This leads to increased sodium and chloride excretion but typically causes potassium wasting (hypokalemia), which differs from the increased urinary potassium concentration seen with drug X.
Mineralocorticoid actions US Medical PG Question 6: Activation of the renin-angiotensin-aldosterone system yields a significant physiological effect on renal blood flow and filtration. Which of the following is most likely to occur in response to increased levels of Angiotensin-II?
- A. Decreased renal plasma flow, decreased filtration fraction
- B. Decreased renal plasma flow, increased glomerular capillary oncotic pressure
- C. Increased renal plasma flow, decreased filtration fraction
- D. Increased renal plasma flow, increased filtration fraction
- E. Decreased renal plasma flow, increased filtration fraction (Correct Answer)
Mineralocorticoid actions Explanation: ***Decreased renal plasma flow, increased filtration fraction***
- **Angiotensin II** causes **efferent arteriolar constriction**, which reduces blood flow leaving the glomerulus, thereby **decreasing renal plasma flow**.
- This efferent constriction also increases **glomerular hydrostatic pressure** and reduces plasma flow distal to the glomerulus, leading to a **higher filtration fraction** (GFR/RPF).
*Decreased renal plasma flow, decreased filtration fraction*
- While **renal plasma flow decreases**, a **decreased filtration fraction** would imply that either GFR decreases disproportionately more than RPF or GFR does not increase despite the RPF reduction, which is not the typical response to **angiotensin II** due to its predominant effect on the **efferent arteriole**.
*Decreased renal plasma flow, increased glomerular capillary oncotic pressure*
- **Increased glomerular capillary oncotic pressure** is a consequence of increased filtration fraction, as more fluid is filtered out, leaving behind a more concentrated plasma. This option includes a correct element (decreased RPF) but pairs it with a less direct and defining outcome of acute Angiotensin II action as the primary physiological effect.
*Increased renal plasma flow, decreased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, predominantly of the efferent arteriole, which by definition would **decrease renal plasma flow**, not increase it.
- A **decreased filtration fraction** would be inconsistent with efferent arteriolar constriction which typically raises GFR relative to RPF.
*Increased renal plasma flow, increased filtration fraction*
- **Angiotensin II** causes **vasoconstriction**, leading to a **decrease in renal plasma flow**, not an increase.
- While **filtration fraction is increased**, the initial premise of increased renal plasma flow is incorrect.
Mineralocorticoid actions US Medical PG Question 7: A 69-year-old woman is brought to the emergency department because of fatigue and lethargy for 5 days. She has also had weakness and nausea for the last 3 days. She has sarcoidosis, major depressive disorder, and hypertension. She had a stroke 5 years ago. Current medications include aspirin, nifedipine, prednisolone, fluoxetine, and rosuvastatin, but she has not taken any of her medications for 7 days due to international travel. Her temperature is 36.1°C (96.9°F), pulse is 95/min, and blood pressure is 85/65 mm Hg. She is lethargic but oriented. Examination shows no other abnormalities. Her hemoglobin concentration is 13.4 g/dL and leukocyte count is 9,600/mm3. Both serum cortisol and ACTH levels are decreased. This patient is most likely to have which of the following additional laboratory abnormalities?
- A. Hyperglycemia
- B. Hyperkalemia
- C. Hyponatremia (Correct Answer)
- D. Hypokalemia
- E. Normal anion gap metabolic acidosis
Mineralocorticoid actions Explanation: ***Hyponatremia***
- This patient has **secondary adrenal insufficiency** due to **HPA axis suppression** from chronic prednisolone use, precipitated by abrupt withdrawal after 7 days without medication.
- **Both decreased cortisol and ACTH** confirm secondary (central) adrenal insufficiency, distinguishing it from primary adrenal insufficiency where ACTH would be elevated.
- **Hyponatremia** develops due to **cortisol deficiency** impairing free water excretion, leading to dilutional hyponatremia—a hallmark laboratory finding in adrenal insufficiency.
- Clinical features include **fatigue, lethargy, hypotension, nausea, and weakness**, consistent with adrenal crisis.
*Hyperglycemia*
- While **glucocorticoids** cause hyperglycemia, **cortisol deficiency** in adrenal insufficiency leads to **impaired gluconeogenesis** and a tendency toward **hypoglycemia**, not hyperglycemia.
- The patient's presentation with hypotension and weakness is consistent with adrenal crisis, not hyperglycemia.
*Hyperkalemia*
- **Hyperkalemia** is characteristic of **primary adrenal insufficiency** (Addison's disease) due to **aldosterone deficiency** affecting the renin-angiotensin-aldosterone system.
- In **secondary adrenal insufficiency**, the hypothalamic-pituitary axis is suppressed but the **renin-angiotensin-aldosterone system remains intact**, so aldosterone secretion is preserved and significant hyperkalemia does not occur.
*Hypokalemia*
- **Hypokalemia** is not a typical feature of adrenal insufficiency and is more commonly associated with diuretic use, primary hyperaldosteronism, or other conditions not present in this case.
- The patient's condition reflects cortisol deficiency with preserved aldosterone function.
*Normal anion gap metabolic acidosis*
- **Normal anion gap metabolic acidosis** occurs in conditions like **renal tubular acidosis** or **diarrhea**, but is not a direct or common consequence of secondary adrenal insufficiency.
- The acute presentation with hypotension and electrolyte disturbance (hyponatremia) is the primary metabolic derangement in this case.
Mineralocorticoid actions US Medical PG Question 8: A group of scientists is studying the mechanism of action of various pancreatic hormones in rats. The scientists studied hormone A, which is secreted by the β-cells of the pancreas, and found that hormone A binds to a complex dimeric receptor on the cell membrane and exerts its effects via phosphorylation and subsequent downstream signaling that includes dephosphorylation of different intracellular proteins. Now they are studying hormone B, which is secreted by the α-cells and antagonizes the actions of hormone A. Which 2nd messenger system would hormone B utilize to exert its cellular effects?
- A. Direct cytoplasmic receptor binding
- B. Phospholipase C
- C. Tyrosine kinase
- D. Direct nuclear receptor binding
- E. Adenylyl cyclase-cyclic AMP (Correct Answer)
Mineralocorticoid actions Explanation: ***Adenylyl cyclase-cyclic AMP***
- Hormone B is **glucagon**, secreted by pancreatic α-cells, which antagonizes the effects of insulin (hormone A). Glucagon primarily acts through a **G protein-coupled receptor** that activates **adenylyl cyclase**, leading to an increase in intracellular **cyclic AMP (cAMP)**.
- Increased cAMP then activates **protein kinase A (PKA)**, which phosphorylates various intracellular proteins to promote **glycogenolysis** and **gluconeogenesis**, thereby raising blood glucose levels.
*Direct cytoplasmic receptor binding*
- This mechanism is characteristic of **steroid hormones**, which are lipid-soluble and can diffuse across the cell membrane to bind to receptors in the cytoplasm.
- Pancreatic hormones like glucagon are **peptide hormones**, which are water-soluble and typically bind to cell surface receptors.
*Phospholipase C*
- Activation of **phospholipase C (PLC)** leads to the production of **inositol triphosphate (IP3)** and **diacylglycerol (DAG)**, which mobilize intracellular calcium and activate protein kinase C, respectively.
- While some G protein-coupled receptors activate PLC, **glucagon's primary signaling pathway** involves adenylyl cyclase.
*Tyrosine kinase*
- **Tyrosine kinase receptors** are often associated with growth factors and insulin (hormone A) signaling, leading to phosphorylation of tyrosine residues on target proteins.
- Glucagon's receptor is a **G protein-coupled receptor**, not a receptor tyrosine kinase, and its actions are mediated through serine/threonine phosphorylation via PKA.
*Direct nuclear receptor binding*
- This mechanism is typical for **steroid hormones** and **thyroid hormones**, which are lipid-soluble and bind to receptors in the nucleus to directly influence gene transcription.
- As a peptide hormone, glucagon binds to cell surface receptors and does not directly interact with nuclear receptors.
Mineralocorticoid actions US Medical PG Question 9: A researcher measures action potential propagation velocity in various regions of the heart in a 42-year-old Caucasian female. Which of the following set of measurements corresponds to the velocities found in the atrial muscle, AV Node, Purkinje system, and ventricular muscle, respectively?
- A. 0.05 m/s, 1.1 m/s, 2.2 m/s, 3.3 m/s
- B. 2.2 m/s, 0.3 m/s, 0.05 m/s, 1.1 m/s
- C. 0.3 m/s, 2.2 m/s, 0.05 m/s, 1.1 m/s
- D. 0.5 m/s, 1.1 m/s, 2.2 m/s, 3 m/s
- E. 1.1 m/s, 0.05 m/s, 2.2 m/s, 0.3 m/s (Correct Answer)
Mineralocorticoid actions Explanation: ***1.1 m/s, 0.05 m/s, 2.2 m/s, 0.3 m/s***
- This option correctly lists the approximate conduction velocities for the **atrial muscle (1.1 m/s)**, **AV node (0.05 m/s)**, **Purkinje system (2.2 m/s)**, and **ventricular muscle (0.3 m/s)**, respectively.
- The **AV node has the slowest conduction velocity (~0.05 m/s)**, which is crucial for delaying ventricular contraction and allowing complete ventricular filling.
- The **Purkinje system has the fastest conduction velocity (~2-4 m/s)**, ensuring rapid and coordinated ventricular depolarization.
- **Atrial muscle (~1 m/s)** and **ventricular muscle (~0.3-0.5 m/s)** have intermediate velocities.
*0.05 m/s, 1.1 m/s, 2.2 m/s, 3.3 m/s*
- This sequence is incorrect because it places the **AV node's velocity (0.05 m/s)** first (as atrial muscle) and significantly overestimates ventricular muscle velocity (3.3 m/s).
- Atrial muscle conducts faster than 0.05 m/s, and ventricular muscle velocity should be approximately 0.3-0.5 m/s, not 3.3 m/s.
*2.2 m/s, 0.3 m/s, 0.05 m/s, 1.1 m/s*
- This option incorrectly assigns the **highest velocity (2.2 m/s)** to atrial muscle, which is characteristic of the Purkinje system, and misplaces the **slowest velocity (0.05 m/s)** in the Purkinje system instead of the AV node.
- The values do not align with known physiological conduction speeds across cardiac tissues.
*0.3 m/s, 2.2 m/s, 0.05 m/s, 1.1 m/s*
- This sequence incorrectly places the **slowest velocity (0.05 m/s)** in the Purkinje system, which is known for the most rapid conduction, and assigns an unrealistically high velocity (2.2 m/s) to the AV node.
- The arrangement directly contradicts the physiological function and relative speeds within the cardiac conduction system.
*0.5 m/s, 1.1 m/s, 2.2 m/s, 3 m/s*
- This option underestimates the **atrial muscle velocity** (0.5 m/s instead of ~1 m/s) and significantly overestimates the **ventricular muscle velocity** (3 m/s instead of ~0.3-0.5 m/s).
- The provided values do not accurately represent the typical ranges of conduction velocities for each specified cardiac region.
Mineralocorticoid actions US Medical PG Question 10: A 38-year-old woman presents to the physician’s clinic with a 6-month history of generalized weakness that usually worsens as the day progresses. She also complains of the drooping of her eyelids and double vision that is worse in the evening. Physical examination reveals bilateral ptosis after a sustained upward gaze and loss of eye convergence which improves upon placing ice packs over the eyes and after the administration of edrophonium. Which of the following is an intrinsic property of the muscle group affected in this patient?
- A. A small mass per motor unit
- B. High ATPase activity (Correct Answer)
- C. High myoglobin content
- D. High density of mitochondria
- E. Increased amount of ATP generated per molecule of glucose
Mineralocorticoid actions Explanation: ***High ATPase activity***
- This patient presents with **myasthenia gravis (MG)**, an autoimmune disorder affecting the neuromuscular junction through antibodies against acetylcholine receptors.
- **Extraocular muscles** and other muscles affected early in MG contain a high proportion of **fast-twitch (Type II) muscle fibers**, which are characterized by **high ATPase activity**.
- **Type II fibers** with high ATPase activity generate rapid, powerful contractions but are **more susceptible to neuromuscular junction dysfunction** due to their higher firing rates and greater dependence on efficient neuromuscular transmission.
- This intrinsic property (high ATPase activity) is why these muscles are preferentially affected in myasthenia gravis.
*A small mass per motor unit*
- While extraocular muscles do have **small motor units** (allowing for precise eye movements), this describes the **innervation pattern** rather than an intrinsic biochemical property of the muscle fibers themselves.
- The question specifically asks about an intrinsic property of the muscle group, referring to the metabolic and contractile characteristics of the muscle fibers.
*High myoglobin content*
- **High myoglobin content** is characteristic of **Type I (slow-twitch) oxidative fibers**, which rely on sustained oxygen delivery for prolonged, fatigue-resistant contractions.
- Muscles preferentially affected in MG have a higher proportion of **Type II fibers**, which have lower myoglobin content compared to Type I fibers.
*High density of mitochondria*
- **High mitochondrial density** is characteristic of **Type I (slow-twitch) oxidative fibers** that depend on aerobic metabolism for sustained energy production.
- While extraocular muscles do have oxidative capacity, the **Type II fibers** preferentially affected in MG have relatively lower mitochondrial density compared to Type I fibers and rely more on glycolytic metabolism for rapid energy needs.
*Increased amount of ATP generated per molecule of glucose*
- **Aerobic respiration** in Type I fibers generates approximately 32 ATP molecules per glucose through oxidative phosphorylation.
- **Type II fibers** rely more heavily on **anaerobic glycolysis**, which produces only 2 ATP per glucose molecule, making them less efficient in ATP generation per glucose.
- The muscles affected in MG have higher proportions of Type II fibers with lower ATP efficiency per glucose molecule.
More Mineralocorticoid actions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.