Hypothalamic-pituitary axis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypothalamic-pituitary axis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypothalamic-pituitary axis US Medical PG Question 1: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Hypothalamic-pituitary axis Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
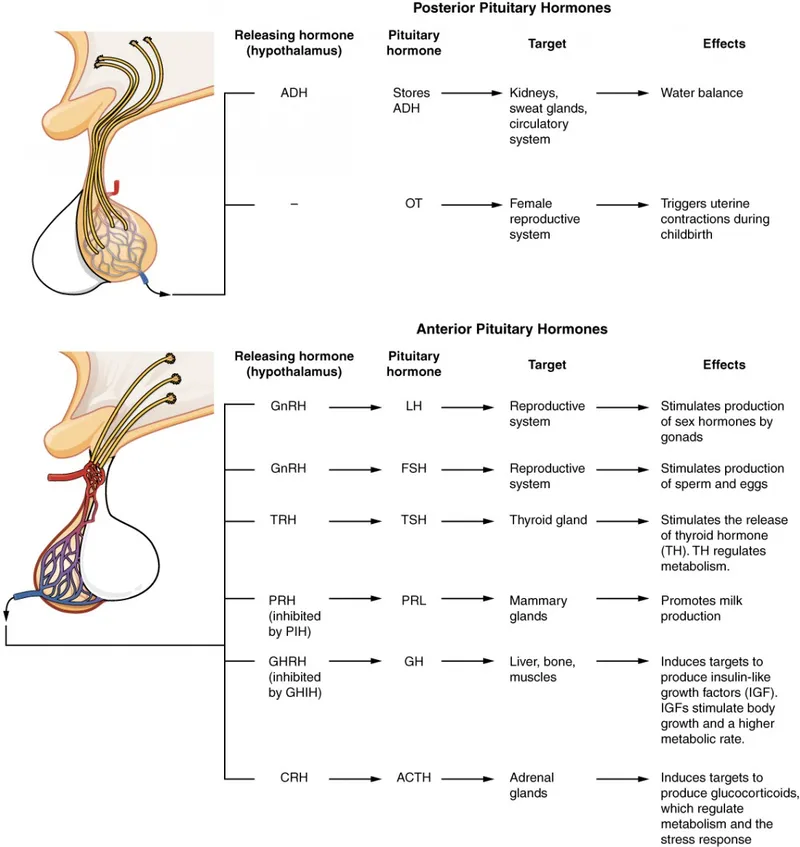
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
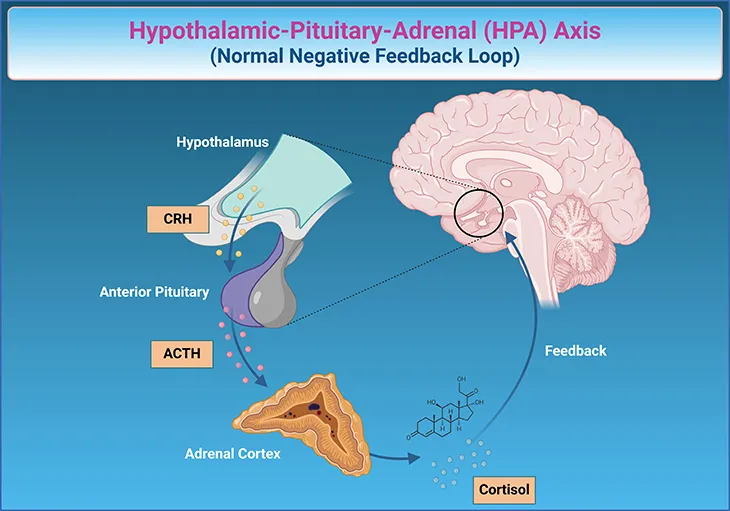
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Hypothalamic-pituitary axis US Medical PG Question 2: A 28-year-old patient comes to the physician’s office with complaints of headaches and difficulty seeing out of the corner of her eye. She gave birth to her son 1 year ago. Further visual testing reveals the patient has bitemporal hemianopsia. The patient undergoes brain MRI which shows an anterior pituitary mass, likely adenoma. The patient has her blood tested to see if the adenoma is secreting extra hormone. The patient is found to have a slight excess of a hormone that uptakes a basophilic stain. Which of the following is most likely to be the hormone detected in her blood?
- A. Prolactin
- B. Growth hormone
- C. Thyroid stimulating hormone (Correct Answer)
- D. Antidiuretic hormone
- E. Oxytocin
Hypothalamic-pituitary axis Explanation: ***Thyroid stimulating hormone***
- **Thyroid-stimulating hormone (TSH)** is synthesized by **thyrotroph cells** which are basophilic, making it the most likely hormone to stain basophilically in this context.
- An excess of TSH from a pituitary adenoma could lead to clinical symptoms of **hyperthyroidism**, although the question states it's only a "slight excess."
*Prolactin*
- **Prolactin** is secreted by **lactotrophs**, which are acidophilic and would not take up a basophilic stain.
- While **prolactinomas** are the most common pituitary adenomas, their cells are not basophilic, and this patient does not exhibit common symptoms of hyperprolactinemia (galactorrhea, amenorrhea).
*Growth hormone*
- **Growth hormone (GH)** is produced by **somatotrophs**, which are acidophilic and would not take up a basophilic stain.
- Excess GH typically causes **acromegaly** in adults, characterized by distinctive physical changes not mentioned in the patient's presentation.
*Antidiuretic hormone*
- **Antidiuretic hormone (ADH)**, also known as vasopressin, is synthesized in the **hypothalamus** and released from the posterior pituitary, not secreted by basophilic cells of the anterior pituitary.
- Overproduction of ADH leads to **SIADH**, characterized by hyponatremia and concentrated urine, none of which are described.
*Oxytocin*
- **Oxytocin** is also produced in the **hypothalamus** and released from the posterior pituitary, not by basophilic cells in the anterior pituitary.
- Its primary functions relate to uterine contractions and milk ejection and are not associated with pituitary adenomas causing bitemporal hemianopsia.
Hypothalamic-pituitary axis US Medical PG Question 3: A 22-year-old G1P1 has an uncomplicated vaginal delivery and delivers a newborn boy at 39 + 1 weeks. The APGAR scores are 8 and 9 at 1 and 5 minutes, respectively. Shortly after the delivery, the child is put on his mother's chest for skin-to-skin and the mother is encouraged to initiate breastfeeding. Which of the following cells produces the hormone responsible for establishing lactation during this process?
- A. Lactotropes (Correct Answer)
- B. Corticotropes
- C. Thyrotropes
- D. Somatotropes
- E. Gonadotropes
Hypothalamic-pituitary axis Explanation: ***Lactotropes***
- **Lactotropes** are cells in the **anterior pituitary gland** that primarily produce and secrete **prolactin**, the hormone essential for initiating and maintaining lactation.
- The drop in **progesterone** and **estrogen** levels after placental delivery removes the inhibitory effect on prolactin, allowing it to stimulate milk production.
*Corticotropes*
- **Corticotropes** produce **adrenocorticotropic hormone (ACTH)**, which stimulates the adrenal cortex to secrete cortisol and other corticosteroids.
- While corticosteroids play a role in mammary gland development, ACTH is not directly responsible for establishing lactation.
*Thyrotropes*
- **Thyrotropes** produce **thyroid-stimulating hormone (TSH)**, which regulates the function of the thyroid gland.
- Thyroid hormones are important for overall metabolism and can influence general reproductive health, but they do not directly establish lactation.
*Somatotropes*
- **Somatotropes** produce **growth hormone (GH)**, which is involved in growth, metabolism, and cell reproduction.
- Although GH has some lactogenic properties and can act synergistically with prolactin, it is not the primary hormone responsible for establishing lactation.
*Gonadotropes*
- **Gonadotropes** produce **luteinizing hormone (LH)** and **follicle-stimulating hormone (FSH)**, which regulate the function of the ovaries and testes.
- These hormones are crucial for ovulation and ovarian steroid production, but they do not directly contribute to the establishment of lactation.
Hypothalamic-pituitary axis US Medical PG Question 4: A 43-year-old woman is found in the hospital to have a plasma sodium concentration of 126 mg/dL. She was hospitalized after she expressed suicidal ideations and was started on a medication for major depressive disorder. Her past medical history is significant for diabetes for which she is currently taking metformin. Her blood pressure while in the hospital has been around 130/85 mmHg and she is not taking any other medications. Laboratory studies show a serum osmolality of 265 mOsm/kg. Which of the following best describes the cell bodies of the cells that are behaving abnormally in this patient?
- A. Basophils in the anterior pituitary
- B. Chromophobes in the anterior pituitary
- C. Acidophils in the anterior pituitary
- D. Located in the hypothalamus (Correct Answer)
- E. Located in the posterior pituitary
Hypothalamic-pituitary axis Explanation: ***Located in the hypothalamus***
- The patient's **hyponatremia** (126 mg/dL) with a **low serum osmolality** (265 mOsm/kg) in the presence of depression and medication suggests **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
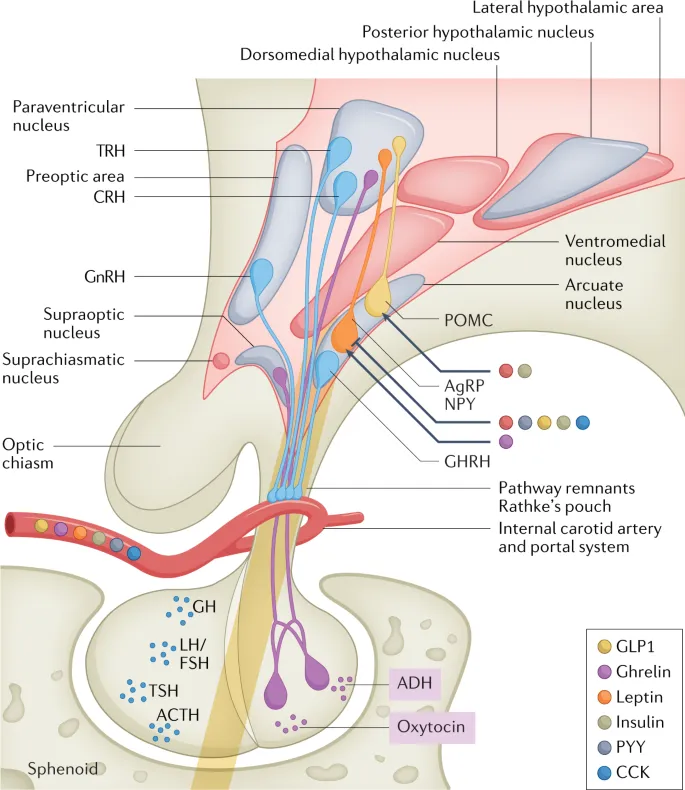
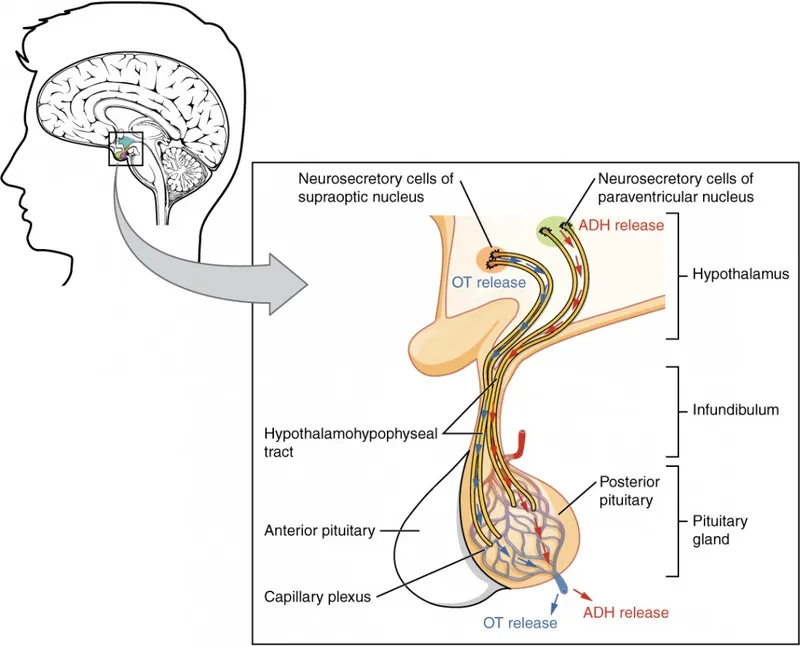
- **ADH (vasopressin)** is synthesized in the magnocellular neurosecretory cells of the **hypothalamus** (specifically the supraoptic and paraventricular nuclei) and then transported to the posterior pituitary for release. Since the patient's condition is due to inappropriate ADH secretion, the abnormality originates in the hypothalamus where these cells are located.
*Basophils in the anterior pituitary*
- **Basophils** in the anterior pituitary produce hormones like **TSH, FSH, and LH**, which are not directly involved in the regulation of water balance and sodium levels in the context of SIADH.
- An abnormality in these cells would lead to endocrine dysfunction related to thyroid or gonadal axes, not hyponatremia.
*Chromophobes in the anterior pituitary*
- **Chromophobes** are cells in the anterior pituitary that are typically undifferentiated or degranulated, often representing cells that have released their stored hormones.
- They are not primarily responsible for the production or release of hormones involved in water balance, so an abnormality here is unlikely to cause SIADH.
*Acidophils in the anterior pituitary*
- **Acidophils** in the anterior pituitary produce **growth hormone (GH)** and **prolactin**.
- Abnormalities in these cells would lead to conditions like acromegaly or hyperprolactinemia, neither of which explains the patient's hyponatremia and low serum osmolality.
*Located in the posterior pituitary*
- While the **posterior pituitary** stores and releases **ADH**, it does not synthesize it; the cell bodies responsible for ADH production are in the hypothalamus.
- Therefore, the primary abnormal cells in SIADH are the ones synthesizing ADH in the hypothalamus, not merely storing it in the posterior pituitary.
Hypothalamic-pituitary axis US Medical PG Question 5: Steroid hormone synthesis, lipid synthesis, and chemical detoxification are activities of which of the following?
- A. Peroxisomes
- B. Nucleolus
- C. Rough Endoplasmic Reticulum
- D. Smooth Endoplasmic Reticulum (Correct Answer)
- E. Golgi bodies
Hypothalamic-pituitary axis Explanation: ***Smooth Endoplasmic Reticulum***
- The **smooth endoplasmic reticulum (SER)** is rich in enzymes that catalyze the synthesis of **lipids**, including steroid hormones, and is crucial for the detoxification of drugs and poisons, particularly in liver cells.
- Its tubular structure, devoid of ribosomes, differentiates its functions from the rough ER, focusing on metabolic processes like **calcium ion storage** and carbohydrate metabolism.
*Peroxisomes*
- Peroxisomes are primarily involved in the breakdown of **fatty acids** and amino acids, producing hydrogen peroxide as a byproduct.
- They also play a role in detoxification but are not the primary site for steroid hormone or general lipid synthesis.
*Nucleolus*
- The **nucleolus** is a dense structure within the nucleus responsible for synthesizing **ribosomal RNA (rRNA)** and assembling ribosomes.
- It has no direct role in steroid hormone synthesis, lipid metabolism, or chemical detoxification.
*Rough Endoplasmic Reticulum*
- The **rough endoplasmic reticulum (RER)** is studded with **ribosomes** and is primarily involved in the synthesis and modification of **proteins** destined for secretion or insertion into membranes.
- While it's part of the endomembrane system, it does not directly perform lipid synthesis or chemical detoxification as its main functions.
*Golgi bodies*
- **Golgi bodies (or Golgi apparatus)** are responsible for modifying, sorting, and packaging **proteins and lipids** synthesized in the ER into vesicles for secretion or delivery to other organelles.
- They do not perform the initial synthesis of steroid hormones or lipids, nor are they the primary site for chemical detoxification.
Hypothalamic-pituitary axis US Medical PG Question 6: An investigator studying hormone synthesis and transport uses immunocytochemical techniques to localize a carrier protein in the central nervous system of an experimental animal. The investigator finds that this protein is synthesized together with a specific hormone from a composite precursor. The protein is involved in the transport of the hormone from the supraoptic and paraventricular nuclei to its destination. The hormone transported by these carrier proteins is most likely responsible for which of the following functions?
- A. Stimulation of thyroglobulin cleavage
- B. Upregulation of renal aquaporin-2 channels (Correct Answer)
- C. Hyperplasia of the adrenal zona fasciculata
- D. Increased insulin-like growth factor 1 production
- E. Maturation of primordial germ cells
Hypothalamic-pituitary axis Explanation: ***Upregulation of renal aquaporin-2 channels***
- The description of a hormone synthesized in the **supraoptic** and **paraventricular nuclei** and transported by a carrier protein refers to **antidiuretic hormone (ADH)**, also known as vasopressin.
- ADH's primary function in the kidney is to **increase water reabsorption** by upregulating **aquaporin-2 channels** in the principal cells of the collecting ducts.
*Stimulation of thyroglobulin cleavage*
- **Thyroglobulin cleavage** and subsequent release of thyroid hormones (T3, T4) are stimulated by **thyroid-stimulating hormone (TSH)**, which is produced by the anterior pituitary, not the hypothalamus.
- The described origin in the supraoptic and paraventricular nuclei is inconsistent with TSH.
*Hyperplasia of the adrenal zona fasciculata*
- **Adrenocorticotropic hormone (ACTH)** from the anterior pituitary stimulates the adrenal cortex, including the zona fasciculata, to produce cortisol.
- The hormone described here originates in the hypothalamus and is transported to the posterior pituitary, not stimulating adrenal hyperplasia.
*Increased insulin-like growth factor 1 production*
- **Insulin-like growth factor 1 (IGF-1)** production is stimulated primarily by **growth hormone (GH)**, which is secreted by the anterior pituitary.
- This function is not associated with hormones produced in the supraoptic and paraventricular nuclei.
*Maturation of primordial germ cells*
- The maturation of **primordial germ cells** is regulated by **gonadotropins (FSH and LH)**, which are secreted by the anterior pituitary, and sex steroids.
- This process is not directly controlled by hormones originating from the supraoptic and paraventricular nuclei.
Hypothalamic-pituitary axis US Medical PG Question 7: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
Hypothalamic-pituitary axis Explanation: ***Antidiuretic hormone***
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
Hypothalamic-pituitary axis US Medical PG Question 8: A 60-year-old man with type 2 diabetes on metformin and insulin presents with 3 days of nausea, vomiting, and diffuse abdominal pain. He appears ill and confused. Vital signs: BP 95/60 mmHg, HR 115/min, RR 28/min, T 37.2°C. Labs show glucose 380 mg/dL, pH 7.28, HCO3 18 mEq/L, anion gap 24, serum osmolality 310 mOsm/kg, negative urine ketones, creatinine 2.8 mg/dL (baseline 1.1), lactate 8.2 mmol/L. Apply physiological principles to determine the primary acid-base and metabolic disturbance.
- A. Sepsis-induced lactic acidosis with stress hyperglycemia
- B. Hyperosmolar hyperglycemic state complicated by lactic acidosis from metformin (Correct Answer)
- C. Alcoholic ketoacidosis with concurrent diabetic emergency
- D. Diabetic ketoacidosis with renal failure from volume depletion
- E. Mixed metabolic acidosis from uremia and starvation ketosis
Hypothalamic-pituitary axis Explanation: ***Hyperosmolar hyperglycemic state complicated by lactic acidosis from metformin***
- The patient exhibits features of **Hyperosmolar Hyperglycemic State (HHS)**, including significant hyperglycemia and confusion, but the **negative urine ketones** effectively rule out DKA.
- The severe **high anion gap metabolic acidosis** is driven by a **lactate of 8.2 mmol/L**, likely due to **Metformin-Associated Lactic Acidosis (MALA)** triggered by **acute kidney injury** (creatinine 2.8).
*Sepsis-induced lactic acidosis with stress hyperglycemia*
- While the patient is hypotensive and tachycardic, the **serum glucose of 380 mg/dL** and history of insulin use point primarily to a diabetic emergency rather than simple stress hyperglycemia.
- **Lactic acidosis** in sepsis usually occurs alongside clinical signs of infection, which are not the focus of this metformin-using patient's profile.
*Alcoholic ketoacidosis with concurrent diabetic emergency*
- **Alcoholic ketoacidosis** would typically present with a history of alcohol abuse and **positive ketones** (specifically beta-hydroxybutyrate), which contradicts the **negative urine ketones** found here.
- The primary source of acidosis in this patient is clearly identified as **lactate (8.2 mmol/L)**, not ketoacids.
*Diabetic ketoacidosis with renal failure from volume depletion*
- **Diabetic Ketoacidosis (DKA)** is unlikely given the **negative urine ketones** and a pH/bicarbonate profile that is less severe than typically seen in profound ketoacidosis.
- DKA usually presents with a lower glucose level (often <250-300 mg/dL) compared to the hyperosmolar states seen in **Type 2 Diabetes** patients.
*Mixed metabolic acidosis from uremia and starvation ketosis*
- While **uremia** contributes to the anion gap when creatinine is elevated (2.8 mg/dL), it is rarely the primary cause of an **anion gap of 24** without more advanced renal failure.
- **Starvation ketosis** would result in positive ketones and a much milder acidosis than the profound **lactic acidosis** (8.2 mmol/L) observed in this case.
Hypothalamic-pituitary axis US Medical PG Question 9: A 38-year-old woman presents with hypertension (170/105 mmHg), hypokalemia (2.9 mEq/L), and metabolic alkalosis. Plasma aldosterone is elevated at 35 ng/dL (normal 4-31) and plasma renin activity is suppressed at 0.2 ng/mL/hr (normal 0.5-3.5). CT scan shows a 2.5 cm left adrenal mass. She also reports recent diagnosis of hyperthyroidism and is being evaluated for a neck mass. Synthesize these findings to evaluate for an underlying unifying diagnosis requiring modified treatment approach.
- A. Ectopic ACTH syndrome from thyroid carcinoma causing bilateral adrenal hyperplasia
- B. Multiple endocrine neoplasia type 2 requiring RET proto-oncogene testing and comprehensive screening (Correct Answer)
- C. Carney complex requiring cardiac myxoma screening before adrenal surgery
- D. Isolated aldosterone-producing adenoma requiring unilateral adrenalectomy only
- E. Coincidental adrenal adenoma and Graves' disease requiring separate standard treatments
Hypothalamic-pituitary axis Explanation: ***Multiple endocrine neoplasia type 2 requiring RET proto-oncogene testing and comprehensive screening***
- The presence of an **adrenal mass** and a **neck mass** in a relatively young patient with hypertension points toward **Multiple Endocrine Neoplasia type 2 (MEN 2)**, specifically medullary thyroid cancer and potential pheochromocytoma.
- While the labs mimic **primary hyperaldosteronism**, the high-risk combination requires **RET proto-oncogene** testing to identify a syndromic association and prevent surgical catastrophes.
*Ectopic ACTH syndrome from thyroid carcinoma causing bilateral adrenal hyperplasia*
- Ectopic ACTH typically results from **small cell lung cancer** or bronchial carcinoids and presents with **hypercortisolism** (Cushing syndrome), not primary hyperaldosteronism.
- The CT scan specifically identified a **unilateral 2.5 cm mass**, which is inconsistent with the **bilateral adrenal hyperplasia** seen in ACTH-secreting tumors.
*Carney complex requiring cardiac myxoma screening before adrenal surgery*
- Carney complex usually involves **Primary Pigmented Nodular Adrenocortical Disease (PPNAD)**, which presents with Cushing syndrome, not the mineralocorticoid excess seen here.
- This syndrome is characterized by **skin lentigines**, **blue nevi**, and **atrial myxomas**, which are not reported in this patient's clinical presentation.
*Isolated aldosterone-producing adenoma requiring unilateral adrenalectomy only*
- While the **high aldosterone** and **low renin** (ARR > 30) suggest an **aldosteronoma (Conn syndrome)**, this diagnosis does not account for the concurrent thyroid and neck masses.
- Proceeding with surgery based on an isolated diagnosis would be dangerous if the mass is actually a **pheochromocytoma** (common in MEN 2) disguised by confounding labs.
*Coincidental adrenal adenoma and Graves' disease requiring separate standard treatments*
- **Graves' disease** typically presents with a diffuse goiter and ophthalmopathy rather than a discrete **neck mass**, which is more indicative of a thyroid nodule or carcinoma.
- In medical examinations, clusters of endocrine findings are rarely coincidental; assuming they are unrelated misses the opportunity to screen for **hereditary syndromes**.
Hypothalamic-pituitary axis US Medical PG Question 10: A 32-year-old pregnant woman at 28 weeks gestation with type 1 diabetes presents with recurrent severe hypoglycemia despite reducing her insulin dose. Her insulin requirements have decreased by 40% over the past week. She reports decreased fetal movement. Fetal ultrasound shows intrauterine fetal demise. Evaluate the physiological mechanism explaining her changing insulin requirements in the context of pregnancy loss.
- A. Increased maternal growth hormone from pituitary compensation for fetal loss
- B. Maternal thyroid hormone surge causing enhanced glucose utilization
- C. Loss of placental lactogen and other diabetogenic hormones that normally increase insulin resistance (Correct Answer)
- D. Increased maternal cortisol from stress of fetal loss improving insulin sensitivity
- E. Placental glucose consumption cessation leading to maternal hyperglycemia compensation
Hypothalamic-pituitary axis Explanation: ***Loss of placental lactogen and other diabetogenic hormones that normally increase insulin resistance***
- Sudden **intrauterine fetal demise** leads to the cessation of placental function and a rapid drop in **human placental lactogen (hPL)**, which normally promotes maternal **insulin resistance**.
- Without these antagonizing hormones, the patient's **insulin sensitivity** returns to pre-pregnancy levels, causing a dramatic decrease in insulin requirements and severe **hypoglycemia**.
*Increased maternal growth hormone from pituitary compensation for fetal loss*
- Maternal **pituitary growth hormone** is actually suppressed during pregnancy as placental growth hormone takes over; there is no compensatory surge upon fetal loss.
- Even if growth hormone were to increase, it is a **diabetogenic hormone** that would increase insulin resistance rather than cause hypoglycemia.
*Maternal thyroid hormone surge causing enhanced glucose utilization*
- Pregnancy loss does not trigger a maternal **thyroid hormone surge**; thyroid levels typically stabilize or decrease following placental dysfunction.
- While hyperthyroidism can affect metabolism, it more commonly causes **glucose intolerance** rather than a 40% reduction in insulin needs.
*Increased maternal cortisol from stress of fetal loss improving insulin sensitivity*
- **Cortisol** is a stress hormone that increases gluconeogenesis and **decreases insulin sensitivity**, which would lead to hyperglycemia.
- Normal pregnancy is already a state of **physiologic hypercortisolism**; the loss of placental function actually reduces the contributions of placental CRH and cortisol.
*Placental glucose consumption cessation leading to maternal hyperglycemia compensation*
- While the fetus and placenta stop consuming glucose after demise, the loss of **anti-insulin hormones** has a much larger impact on the maternal metabolic state.
- The clinical presentation clearly shows **hypoglycemia**, which contradicts a compensatory mechanism for maternal hyperglycemia.
More Hypothalamic-pituitary axis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.