Endocrine feedback systems US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endocrine feedback systems. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endocrine feedback systems US Medical PG Question 1: A 42-year-old woman presents to the physician with symptoms of vague abdominal pain and bloating for several months. Test results indicate that she has ovarian cancer. Her physician attempts to reach her by phone multiple times but cannot reach her. Next of kin numbers are in her chart. According to HIPAA regulations, who should be the primary person the doctor discusses this information with?
- A. The patient's brother
- B. The patient's husband
- C. The patient's daughter
- D. All of the options
- E. The patient (Correct Answer)
Endocrine feedback systems Explanation: ***The patient***
- Under **HIPAA**, the patient has the **right to privacy** regarding their protected health information (PHI). Therefore, the physician must make all reasonable attempts to contact the patient directly to convey their diagnosis.
- Sharing sensitive medical information like a cancer diagnosis with anyone other than the patient, without their explicit consent, would be a **violation of HIPAA regulations**.
*The patient's brother*
- The patient's brother is not automatically authorized to receive her medical information, even if listed as **next of kin**, without the patient's explicit consent or a documented **healthcare power of attorney**.
- Discussing the diagnosis with the brother without the patient's direct consent would be a **breach of patient confidentiality**.
*The patient's husband*
- Even a spouse does not automatically have the right to access a patient's **PHI** without the patient's express permission, according to **HIPAA**.
- While often a trusted contact, without explicit consent, revealing the diagnosis to the husband would still violate the patient's **privacy rights**.
*The patient's daughter*
- Similar to other family members, the patient's daughter is not legally entitled to receive her mother's confidential medical information without explicit authorization or a medical **power of attorney**.
- The physician's primary responsibility is to the patient herself, ensuring her **privacy** is maintained.
*All of the options*
- According to **HIPAA**, sharing the patient's diagnosis with any family member without her explicit consent would be a **breach of confidentiality**.
- This option incorrectly assumes that **next of kin** automatically have the right to receive sensitive medical information.
Endocrine feedback systems US Medical PG Question 2: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
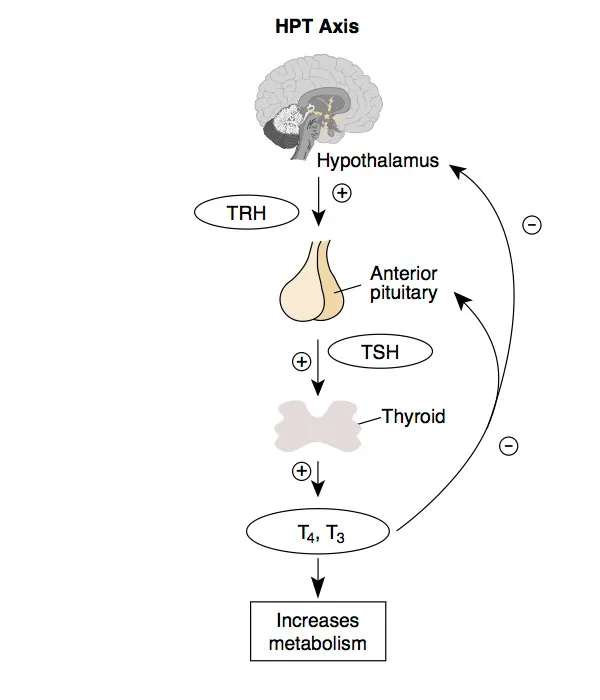
Endocrine feedback systems Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Endocrine feedback systems US Medical PG Question 3: A 32-year-old female presents to her obstetrician 3 weeks postpartum for failure to lactate. Of note, she has been unable to tolerate cold environments since the birth of her child. Review of systems is positive for fatigue, lightheadedness, and a 3-pound weight gain over the last 3 weeks. Her delivery was complicated by placenta accreta with postpartum blood loss. Her newborn infant is doing well on formula. She denies any personal or family history of thyroid disease. Physical exam is overall unremarkable. On a panel of hormone testing, which of the following levels is most likely to be normal in this patient?
- A. Thyroid hormone
- B. Cortisol
- C. Luteinizing hormone
- D. Antidiuretic hormone (Correct Answer)
- E. Aldosterone
Endocrine feedback systems Explanation: ***Antidiuretic hormone***
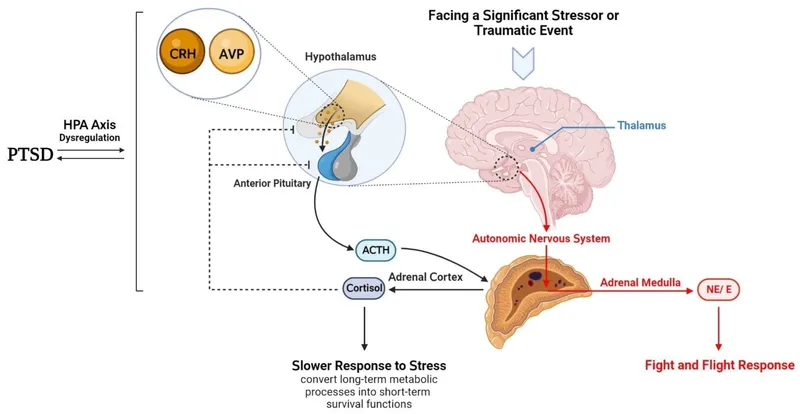
- This patient is presenting with symptoms consistent with **Sheehan syndrome**, which is postpartum pituitary necrosis due to severe hemorrhage and hypovolemic shock.
- Sheehan syndrome **primarily affects the anterior pituitary**, where most pituitary hormones are produced.
- **Antidiuretic hormone (ADH)** is synthesized by the **hypothalamus** and stored/released by the **posterior pituitary**, which is typically **spared** in Sheehan syndrome due to its separate blood supply.
- Therefore, **ADH levels would be normal** in this patient, making this the correct answer.
*Aldosterone*
- The **renin-angiotensin-aldosterone system (RAAS)** is regulated independently by the kidneys and is preserved in pituitary disorders.
- Aldosterone levels would also likely be **normal** in this patient.
- However, ADH is the better answer as it specifically demonstrates the anatomical distinction between anterior and posterior pituitary function.
*Thyroid hormone*
- The **anterior pituitary** fails to produce **thyroid-stimulating hormone (TSH)** in Sheehan syndrome, leading to secondary hypothyroidism.
- This results in **low thyroid hormone levels**.
- Her symptoms of **cold intolerance**, **fatigue**, and **weight gain** are classic manifestations of hypothyroidism.
*Cortisol*
- The anterior pituitary produces **adrenocorticotropic hormone (ACTH)**, which stimulates cortisol release from the adrenal glands.
- In Sheehan syndrome, failure of ACTH production leads to **secondary adrenal insufficiency** with **low cortisol levels**.
- This contributes to her **fatigue** and **lightheadedness**.
*Luteinizing hormone*
- The anterior pituitary produces **luteinizing hormone (LH)**, which is crucial for ovarian function and ovulation.
- The patient's **failure to lactate** is due to **prolactin deficiency** (another anterior pituitary hormone), not LH deficiency.
- Lack of LH and other gonadotropins would contribute to amenorrhea and loss of reproductive function that often accompany Sheehan syndrome.
Endocrine feedback systems US Medical PG Question 4: A 65-year-old obese man presents to his primary care clinic feeling weak. He was in the military and stationed in Vietnam in his youth. His current weakness gradually worsened to the point that he had to call his son to help him stand to get on the ambulance. He smokes a pack of cigarettes every day and drinks a bottle of vodka a week. He has been admitted for alcohol withdrawal multiple times and has been occasionally taking thiamine, folic acid, and naltrexone. He denies taking steroids. His temperature is 98°F (36.7°C), blood pressure is 170/90 mmHg, pulse is 75/min, and respirations are 20/min. He is obese with a significant pannus. Hepatomegaly is not appreciable. Abdominal striae are present. His workup is notable for the following:
Serum:
Na+: 142 mEq/L
Cl-: 102 mEq/L
K+: 3.9 mEq/L
HCO3-: 25 mEq/L
BUN: 24 mg/dL
Glucose: 292 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.1 mg/dL
AST: 7 U/L
ALT: 14 U/L
24-hour urinary cortisol: 400 µg (reference range < 300 µg)
Serum cortisol: 45 pg/mL (reference range < 15 pg/mL)
A 48-hour high dose dexamethasone suppression trial shows that his serum cortisol levels partially decrease to 25 pg/mL and his adrenocorticotropin-releasing hormone (ACTH) level decreases from 10 to 6 pg/mL (reference range > 5 pg/mL). What is the best next step in management?
- A. MRI of the pituitary gland (Correct Answer)
- B. MRI of the adrenal glands
- C. Low-dose dexamethasone therapy for 3 months
- D. CT of the chest
- E. High-dose dexamethasone therapy for 3 months
Endocrine feedback systems Explanation: ***MRI of the pituitary gland***
- The elevated 24-hour urinary cortisol and serum cortisol levels, along with **partial suppression on the high-dose dexamethasone suppression test** and a decrease in ACTH, strongly suggest a pituitary source of **Cushing's disease**.
- An MRI of the pituitary gland is the appropriate next step to visualize an **adenoma** responsible for the excess ACTH production.
*MRI of the adrenal glands*
- An adrenal MRI would be indicated if the ACTH levels were **low or undetectable**, suggesting an adrenal tumor as the primary cause of Cushing's syndrome.
- Since ACTH levels decreased, but remained elevated, an adrenal origin is less likely.
*Low-dose dexamethasone therapy for 3 months*
- Dexamethasone therapy is not a treatment for Cushing's syndrome; instead, it is used as a **diagnostic tool** to assess cortisol suppression.
- Long-term administration of dexamethasone would mimic iatrogenic Cushing's syndrome and **exacerbate the patient's condition**.
*CT of the chest*
- A CT of the chest would be considered if an **ectopic ACTH-producing tumor** (e.g., small cell lung cancer) was suspected, which typically presents with very high ACTH levels and no suppression with high-dose dexamethasone.
- The partial suppression and lower ACTH levels make an ectopic source less likely in this case.
*High-dose dexamethasone therapy for 3 months*
- Similar to low-dose dexamethasone therapy, high-dose dexamethasone is a **diagnostic test**, not a long-term treatment for Cushing's syndrome.
- Such therapy would worsen the patient's condition and **does not address the underlying pathology**.
Endocrine feedback systems US Medical PG Question 5: A 44-year-old woman comes to the physician because of a 6-month history of fatigue, constipation, and a 7-kg (15.4-lb) weight gain. Menses occur irregularly in intervals of 40–50 days. Her pulse is 51/min, and blood pressure is 145/86 mm Hg. Examination shows conjunctival pallor and cool, dry skin. There is mild, nonpitting periorbital edema. Serum thyroid-stimulating hormone concentration is 8.1 μU/mL. Treatment with the appropriate pharmacotherapy is initiated. After several weeks of therapy with this drug, which of the following hormonal changes is expected?
- A. Increased TRH
- B. Increased T3
- C. Decreased T4
- D. Increased T4
- E. Decreased TSH (Correct Answer)
Endocrine feedback systems Explanation: ***Decreased TSH***
- The patient has **primary hypothyroidism** (elevated TSH 8.1 μU/mL, symptoms of fatigue, constipation, bradycardia, weight gain, cool dry skin) and is treated with **levothyroxine (synthetic T4)**.
- The phrase **"after several weeks of therapy"** is key: while T4 levels rise within days of starting levothyroxine, **TSH takes 6-8 weeks to normalize** due to the negative feedback loop.
- As circulating thyroid hormone levels are restored, the **hypothalamic-pituitary-thyroid axis** re-establishes negative feedback, leading to **decreased TSH secretion** from the pituitary.
- **Decreased TSH is the primary clinical marker** used to assess adequacy of thyroid hormone replacement after several weeks of therapy.
*Increased T4*
- While T4 levels do increase with levothyroxine therapy, this occurs **rapidly (within days)**, not over "several weeks."
- The question's timeframe of "several weeks" directs attention to the **delayed TSH response**, which is what clinicians monitor at 6-8 weeks to adjust dosing.
- T4 elevation is immediate; TSH normalization takes weeks and is the endpoint being tested.
*Increased T3*
- T3 levels will increase as **T4 is peripherally converted to the active form T3**, but this is not the primary hormonal change being monitored after several weeks.
- The question asks about expected hormonal changes in the context of treatment monitoring, where **TSH is the gold standard**.
*Increased TRH*
- **Thyrotropin-releasing hormone (TRH)** from the hypothalamus stimulates TSH release. In primary hypothyroidism, both TRH and TSH are elevated.
- With thyroid hormone replacement, negative feedback would lead to **decreased TRH**, not increased.
*Decreased T4*
- This is the opposite of what occurs with levothyroxine therapy.
- The goal of treatment is to **increase** deficient T4 levels to the physiological range.
Endocrine feedback systems US Medical PG Question 6: A 25-year-old man is rushed to the emergency department following a motor vehicle accident. After an initial evaluation, he is found to have bilateral femoral fractures. After surgical fixation of his fractures, he suddenly starts to feel nauseated and becomes agitated. Past medical history is significant for a thyroid disorder. His temperature is 40.0°C (104°F), blood pressure is 165/100 mm Hg, pulse is 170/min and irregularly irregular, and respirations are 20/min. On physical examination, the patient is confused and delirious. Oriented x 0. Laboratory studies are significant for the following:
Thyroxine (T4), free 5 ng/dL
Thyroid stimulating hormone (TSH) 0.001 mU/L
The patient is started on propranolol to control his current symptoms. Which of the following best describes the mechanism of action of this new medication?
- A. Inhibition of an underlying autoimmune process
- B. Interference with enterohepatic circulation and recycling of thyroid hormones
- C. Inhibition of release of thyroid hormones
- D. Inhibition of thyroid peroxidase enzyme
- E. Decrease the peripheral conversion of T4 to T3 (Correct Answer)
Endocrine feedback systems Explanation: ***Decrease the peripheral conversion of T4 to T3***
- **Propranolol**, a non-selective beta-blocker, plays a crucial role in thyroid storm management by **blocking beta-adrenergic receptors**, thereby mitigating the cardiovascular symptoms like tachycardia and hypertension.
- Furthermore, at high doses, propranolol directly **inhibits the peripheral conversion of T4 to T3**, which is the more biologically active thyroid hormone, thus reducing the overall thyroid hormone effect.
*Inhibition of an underlying autoimmune process*
- This mechanism describes drugs like **glucocorticoids** or **immunosuppressants**, which are effective in autoimmune thyroid diseases like Graves' disease but are not the primary mechanism of action for propranolol.
- While thyroid storm is often triggered by **Graves' disease**, initial management focuses on symptom control and blocking hormone effects, not primarily immune suppression by propranolol.
*Interference with enterohepatic circulation and recycling of thyroid hormones*
- This mechanism is characteristic of **cholestyramine** or **iodinated contrast agents**, which bind to thyroid hormones in the gut, preventing their reabsorption and increasing their fecal excretion.
- Propranolol does not significantly influence the enterohepatic circulation or recycling of thyroid hormones.
*Inhibition of release of thyroid hormones*
- This action is primarily achieved by **iodine preparations** (e.g., Lugol's iodine, potassium iodide) given after antithyroid drugs, which acutely block the release of preformed thyroid hormones from the gland.
- Although propranolol can reduce some aspects of sympathetic stimulation, it does not directly inhibit the release of thyroid hormones from the thyroid gland.
*Inhibition of thyroid peroxidase enzyme*
- This mechanism is specific to **thionamides** like **propylthiouracil (PTU)** and **methimazole**, which block the organification of iodine and coupling of iodotyrosines, thereby inhibiting thyroid hormone synthesis.
- Propranolol does not directly affect the thyroid peroxidase enzyme or thyroid hormone synthesis.
Endocrine feedback systems US Medical PG Question 7: Researchers are experimenting with hormone levels in mice in fasting and fed states. To test hormone levels in the fed state, the mice are given an oral glucose load and various hormones are measured in a blood sample. Researchers are most interested in the hormone whose blood levels track evenly with C-peptide levels. The hormone the researchers are most interested in is responsible for which of the following actions in the body?
- A. Protein catabolism
- B. Fatty acid breakdown
- C. Fatty acid synthesis (Correct Answer)
- D. Ketogenesis
- E. Lipolysis
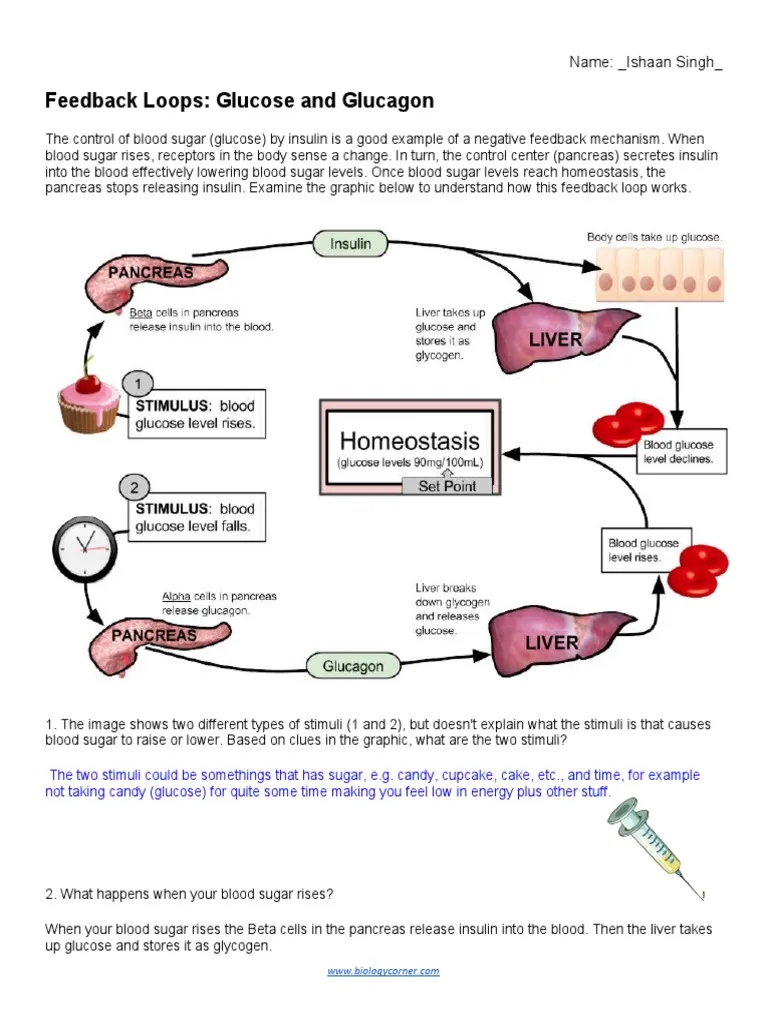
Endocrine feedback systems Explanation: ***Fatty acid synthesis***
- The hormone whose blood levels track evenly with **C-peptide** levels after a glucose load is **insulin**.
- Insulin is a key anabolic hormone that promotes **fatty acid synthesis** from excess glucose in the fed state, particularly in the liver and adipose tissue.
*Protein catabolism*
- **Insulin** is an anabolic hormone that generally **inhibits protein catabolism** and promotes protein synthesis.
- Conditions like **glucagon excess** or **cortisol excess** promote protein catabolism, not insulin.
*Fatty acid breakdown*
- **Insulin inhibits fatty acid breakdown** (beta-oxidation) by suppressing hormone-sensitive lipase.
- **Glucagon** and **epinephrine** promote fatty acid breakdown, especially during fasting.
*Ketogenesis*
- **Insulin inhibits ketogenesis** by reducing the supply of fatty acids to the liver and inhibiting the enzymes involved in ketone body formation.
- **Glucagon** and **low insulin levels** (as in uncontrolled diabetes or prolonged fasting) promote ketogenesis.
*Lipolysis*
- **Insulin is a potent inhibitor of lipolysis** (breakdown of triglycerides into fatty acids and glycerol) in adipose tissue.
- **Glucagon**, **catecholamines**, and **growth hormone** stimulate lipolysis.
Endocrine feedback systems US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Endocrine feedback systems Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Endocrine feedback systems US Medical PG Question 9: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Endocrine feedback systems Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
Endocrine feedback systems US Medical PG Question 10: A 17-year-old boy is brought to the physician because of a sore throat, nonproductive cough, and bloody urine for 3 days. He has had 2 similar episodes involving a sore throat and bloody urine over the past year. His sister has systemic lupus erythematosus. His temperature is 38.1°C (100.6°F). Serum studies show a urea nitrogen concentration of 8 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows acanthocytes and red blood cell casts. Renal ultrasonography shows no abnormalities. A renal biopsy is most likely to show which of the following findings?
- A. Capillary wire looping
- B. IgA mesangial deposition (Correct Answer)
- C. Splitting of the glomerular basement membrane
- D. Effacement of the foot processes
- E. Granular deposits of IgG, IgM, and C3 complement
Endocrine feedback systems Explanation: ***IgA mesangial deposition***
- The patient's history of recurrent gross **hematuria** following pharyngitis, presence of **acanthocytes** and **RBC casts** in urine, and mild renal impairment with normal renal ultrasound strongly suggest **IgA nephropathy (Berger's disease)**.
- **IgA nephropathy** is characterized by the deposition of **IgA immune complexes** in the **glomerular mesangium**, which is the hallmark finding on renal biopsy.
*Capillary wire looping*
- This finding is characteristic of **diffuse proliferative glomerulonephritis**, often associated with **lupus nephritis class IV**, a severe manifestation of **systemic lupus erythematosus (SLE)**.
- While the patient's sister has SLE, his clinical presentation of recurrent hematuria linked to pharyngitis makes IgA nephropathy more likely than lupus nephritis in this individual.
*Splitting of the glomerular basement membrane*
- This is a classic finding in **Alport syndrome**, an inherited disorder characterized by progressive kidney disease, hearing loss, and ocular abnormalities.
- While Alport syndrome can cause recurrent hematuria, the history of episodes following pharyngitis and the family history of SLE (rather than Alport) make it less probable.
*Effacement of the foot processes*
- **Effacement of foot processes (podocytes)** is a characteristic feature of **minimal change disease** and **focal segmental glomerulosclerosis (FSGS)**, which typically present with **nephrotic syndrome** (heavy proteinuria, edema) rather than isolated recurrent gross hematuria.
- This patient's symptoms are more indicative of a nephritic rather than nephrotic process.
*Granular deposits of IgG, IgM, and C3 complement*
- Widespread granular deposits of IgG, IgM, and C3 are typical of **post-streptococcal glomerulonephritis (PSGN)**, which usually presents 1-3 weeks after a **streptococcal infection**.
- While PSGN can cause hematuria, the recurrent nature of his symptoms over a year and rapid onset after pharyngitis are less typical for PSGN, which is usually a single, self-limited episode.
More Endocrine feedback systems US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.