Adrenal medulla and catecholamines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adrenal medulla and catecholamines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adrenal medulla and catecholamines US Medical PG Question 1: A previously healthy 61-year-old man comes to the physician because of a 6-month history of morning headaches. He also has fatigue and trouble concentrating on his daily tasks at work. He sleeps for 8 hours every night; his wife reports that he sometimes stops breathing for a few seconds while sleeping. His pulse is 71/min and blood pressure is 158/96 mm Hg. He is 178 cm (5 ft 10 in) tall and weighs 100 kg (220 lb); BMI is 31.6 kg/m2 . Which of the following is the most likely cause of this patient's hypertension?
- A. Proliferation of adrenal chromaffin cells
- B. Overproduction of cortisol
- C. Hypophyseal neoplasm
- D. Nocturnal upper airway obstruction (Correct Answer)
- E. Hypersecretion of aldosterone
Adrenal medulla and catecholamines Explanation: ***Nocturnal upper airway obstruction***
- The patient's **obesity (BMI 31.6)**, **morning headaches**, fatigue, difficulty concentrating, and spousal report of **witnessed apneic episodes during sleep** are classic signs of **obstructive sleep apnea (OSA)**.
- OSA causes **intermittent hypoxia and hypercapnia** during sleep, leading to **sympathetic nervous system activation**, increased catecholamine release, and **sustained hypertension** even during waking hours.
- OSA is one of the most common **secondary causes of hypertension**, especially in obese patients.
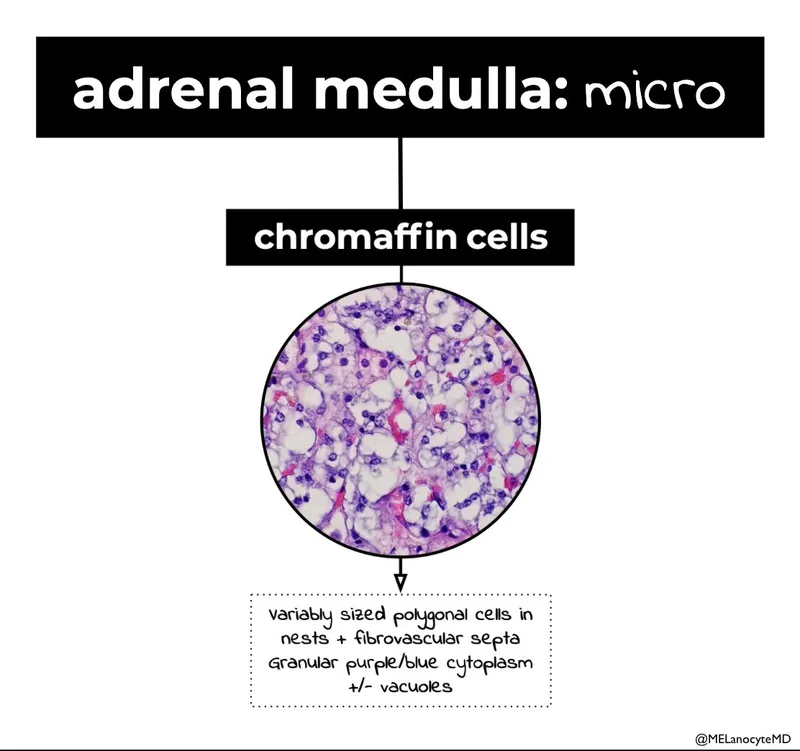
*Proliferation of adrenal chromaffin cells*
- This describes a **pheochromocytoma**, which typically presents with **paroxysmal hypertension**, severe episodic headaches, palpitations, and diaphoresis (the classic "triad").
- While headaches are present, the **sleep-related breathing disturbances** and obesity are not consistent with pheochromocytoma.
*Overproduction of cortisol*
- This suggests **Cushing's syndrome**, which includes symptoms like central obesity, **moon facies, buffalo hump, purple striae**, muscle weakness, and easy bruising, along with hypertension.
- The patient lacks the classic cushingoid features, and the symptoms are more consistent with sleep-disordered breathing.
*Hypophyseal neoplasm*
- A pituitary tumor could cause hypertension if it leads to conditions like **Cushing's disease** (ACTH-secreting) or **acromegaly** (growth hormone excess).
- However, there are no specific symptoms pointing towards a pituitary tumor (no visual field defects, acromegalic features, or cushingoid appearance), and the prominent **witnessed apneas** fit OSA much better.
*Hypersecretion of aldosterone*
- This is characteristic of **primary hyperaldosteronism (Conn's syndrome)**, which commonly presents with hypertension, often accompanied by **hypokalemia**, muscle weakness, and polyuria.
- The patient's symptoms do not suggest electrolyte abnormalities or other classic signs of mineralocorticoid excess.
Adrenal medulla and catecholamines US Medical PG Question 2: A drug research team has synthesized a novel oral drug that acts as an agonist at multiple adrenergic receptors. When administered in animals, it has been shown to produce urinary retention at therapeutic doses with the absence of other manifestations of adrenergic stimulation. The researchers are interested in understanding signal transduction and molecular mechanisms behind the action of the novel drug. Which of the following receptors would most likely transduce signals across the plasma membrane following the administration of this novel drug?
- A. GoPCRs (Go protein-coupled receptors)
- B. GsPCRs (Gs protein-coupled receptors)
- C. GqPCRs (Gq protein-coupled receptors) (Correct Answer)
- D. GtPCRs (Gt protein-coupled receptors)
- E. GiPCRs (Gi protein-coupled receptors)
Adrenal medulla and catecholamines Explanation: ***GqPCRs (Gq protein-coupled receptors)***
- **Urinary retention** is primarily mediated by the activation of **alpha-1 adrenergic receptors** in the bladder neck and prostate, which are classically Gq-protein coupled receptors.
- Activation of **GqPCRs** leads to the activation of **phospholipase C**, increased **IP3 (inositol trisphosphate)** and **DAG (diacylglycerol)**, and subsequently, a rise in intracellular **calcium**, causing smooth muscle contraction.
*GoPCRs (Go protein-coupled receptors)*
- While Go proteins are a subtype of Gi/Go family, their direct primary role in mediating **urinary retention** via **adrenergic agonism** is not as well-established as Gq.
- Go signaling often involves modulation of **ion channels** and can be involved in neuronal signaling, not directly causing smooth muscle contraction in the bladder.
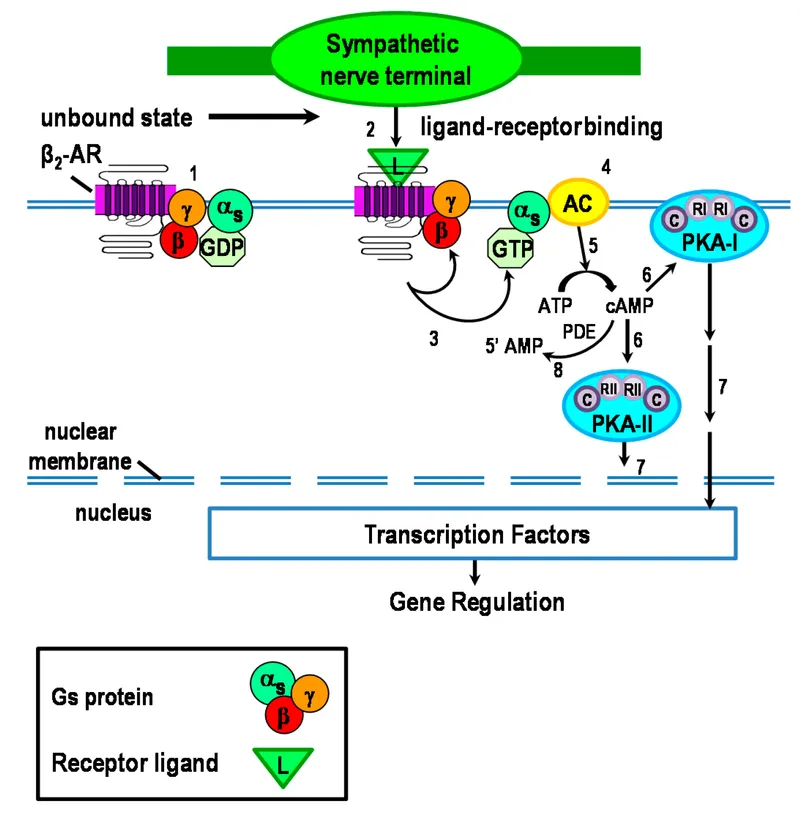
*GsPCRs (Gs protein-coupled receptors)*
- **GsPCRs** (e.g., beta-adrenergic receptors) activate **adenylate cyclase**, leading to increased **cAMP** levels, which typically causes smooth muscle relaxation.
- This effect would promote **urinary relaxation** and flow, not retention, and hence is contrary to the observed drug effect.
*GtPCRs (Gt protein-coupled receptors)*
- **GtPCRs** (transducin) are primarily involved in the **phototransduction** cascade in the retina, mediating vision.
- They have no known central role in mediating adrenergic effects on the **urinary tract smooth muscle**.
*GiPCRs (Gi protein-coupled receptors)*
- **GiPCRs** (e.g., alpha-2 adrenergic receptors) inhibit **adenylate cyclase**, leading to decreased **cAMP** levels, which generally causes smooth muscle contraction in some tissues, but also presynaptic inhibition.
- While Gi activation can lead to contraction in some contexts, the primary mechanism of **urinary retention** via bladder neck contraction is through alpha-1 receptors linked to Gq.
Adrenal medulla and catecholamines US Medical PG Question 3: A 65-year-old male with a history of CHF presents to the emergency room with shortness of breath, lower leg edema, and fatigue. He is diagnosed with acute decompensated congestive heart failure, was admitted to the CCU, and treated with a medication that targets beta-1 adrenergic receptors preferentially over beta-2 adrenergic receptors. The prescribing physician explained that this medication would only be used temporarily as its efficacy decreases within 2-3 days due to receptor downregulation. Which of the following was prescribed?
- A. Epinephrine
- B. Norepinephrine
- C. Milrinone
- D. Isoproterenol
- E. Dobutamine (Correct Answer)
Adrenal medulla and catecholamines Explanation: ***Dobutamine***
- **Dobutamine** is a beta-1 adrenergic agonist preferentially acting on beta-1 receptors in the heart, increasing contractility and heart rate during acute decompensated heart failure.
- Its efficacy reduces over time due to **receptor downregulation**, making it effective for only short-term use, typically less than 72 hours.
*Epinephrine*
- **Epinephrine** is a non-selective adrenergic agonist acting on both alpha and beta receptors, causing vasoconstriction and bronchodilation in addition to cardiac stimulation.
- It is typically used in emergency situations like **cardiac arrest** and **anaphylaxis**, not primarily for acute CHF exacerbation in this manner.
*Norepinephrine*
- **Norepinephrine** primarily acts on alpha-1 adrenergic receptors, causing significant vasoconstriction, and has some beta-1 agonistic effects.
- It is mainly used as a **vasopressor** in septic shock or severe hypotension to increase systemic vascular resistance, rather than directly improving cardiac output in decompensated CHF.
*Milrinone*
- **Milrinone** is a phosphodiesterase-3 inhibitor, increasing intracellular cAMP levels and leading to positive inotropy and vasodilation.
- While used in acute heart failure, its mechanism is distinct from adrenergic agonists, and its efficacy is not limited by a rapid receptor downregulation mechanism as described.
*Isoproterenol*
- **Isoproterenol** is a non-selective beta-adrenergic agonist, stimulating both beta-1 and beta-2 receptors, leading to increased heart rate and contractility, as well as bronchodilation and vasodilation.
- Due to its strong chronotropic effects and potential for severe arrhythmias and hypotension, it is rarely used in CHF and is primarily reserved for conditions like **bradycardia** or **torsades de pointes**.
Adrenal medulla and catecholamines US Medical PG Question 4: A 25-year-old man presents to the emergency department with a severe pulsatile headache for an hour. He says that he is having palpitations as well. He adds that he has had several episodes of headache in the past which resolved without seeking medical attention. He is a non-smoker and does not drink alcohol. He denies use of any illicit drugs. He looks scared and anxious. His temperature is 37°C (98.6°F), respirations are 25/min, pulse is 107/min, and blood pressure is 221/161 mm Hg. An urgent urinalysis reveals elevated plasma metanephrines. What is the next best step in the management of this patient?
- A. Hydralazine
- B. Amlodipine
- C. Phenoxybenzamine followed by propranolol (Correct Answer)
- D. Propranolol followed by phenoxybenzamine
- E. Emergent surgery
Adrenal medulla and catecholamines Explanation: ***Phenoxybenzamine followed by propranolol***
- This patient presents with symptoms highly suggestive of a **pheochromocytoma crisis**, including **severe headache**, **palpitations**, **hypertension**, **tachycardia**, and **anxiety**, along with elevated **plasma metanephrines**. The initial management for a pheochromocytoma crisis is **alpha-blockade** (e.g., with phenoxybenzamine) to control the severe hypertension, followed by **beta-blockade** (e.g., with propranolol) to manage tachycardia and prevent unopposed alpha-agonist effects.
- Giving a beta-blocker before an alpha-blocker can lead to **unopposed alpha-adrenergic stimulation**, which can cause a life-threatening increase in blood pressure due to vasoconstriction.
*Hydralazine*
- While **hydralazine** is a potent direct vasodilator used for hypertensive emergencies, it is generally **not the first-line treatment for pheochromocytoma** crisis.
- It can cause reflex **tachycardia**, which might be detrimental in a patient with excessive catecholamine release.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** that can lower blood pressure.
- However, it is **not the preferred initial agent for the acute hypertensive crisis** associated with pheochromocytoma, which requires specific alpha-blockade.
*Propranolol followed by phenoxybenzamine*
- Administering a **beta-blocker** (propranolol) before an **alpha-blocker** (phenoxybenzamine) in a patient with pheochromocytoma is **contraindicated** and potentially dangerous.
- This sequence could lead to **unopposed alpha-adrenergic stimulation**, resulting in profound **vasoconstriction** and an extreme, life-threatening increase in blood pressure.
*Emergent surgery*
- While surgical removal of the tumor (adrenalectomy) is the **definitive treatment** for pheochromocytoma, it is **not the immediate next step** in a hypertensive crisis.
- The patient needs **pharmacological stabilization** of blood pressure and heart rate first to reduce surgical risks.
Adrenal medulla and catecholamines US Medical PG Question 5: A 20-year-old man is brought to the emergency room for evaluation of a back injury sustained while at work. A CT scan of the lumbar spine shows an incidental 2-cm mass adjacent to the inferior vena cava. Histologic examination of a biopsy specimen of the mass shows clusters of chromaffin cells. This mass is most likely to secrete which of the following substances?
- A. Aldosterone
- B. Dehydroepiandrosterone
- C. Norepinephrine (Correct Answer)
- D. Cortisol
- E. Estrogen
Adrenal medulla and catecholamines Explanation: **Norepinephrine**
- The description of a mass with **clusters of chromaffin cells** is characteristic of a **pheochromocytoma**, a tumor typically arising from the **adrenal medulla**.
- **Pheochromocytomas** are known to secrete catecholamines, primarily **norepinephrine** and epinephrine.
*Aldosterone*
- **Aldosterone** is secreted by the **zona glomerulosa** of the **adrenal cortex** and is involved in blood pressure regulation.
- Tumors secreting aldosterone are usually **aldosteronomas** (Conn's syndrome) and do not arise from chromaffin cells.
*Dehydroepiandrosterone*
- **Dehydroepiandrosterone (DHEA)** is an **adrenal androgen** secreted by the **zona reticularis** of the adrenal cortex.
- Its secretion is associated with cortical tumors or hyperplasia, not chromaffin cell tumors.
*Cortisol*
- **Cortisol** is a glucocorticoid produced by the **zona fasciculata** of the **adrenal cortex**.
- Elevated cortisol levels are usually due to **Cushing's syndrome**, often caused by adrenal adenomas or hyperplasia, not chromaffin cell tumors.
*Estrogen*
- While small amounts of **estrogen** can be produced by the adrenal glands, the primary sites of estrogen synthesis are the **ovaries** and **placenta**.
- A tumor composed of **chromaffin cells** is not typically associated with significant estrogen secretion.
Adrenal medulla and catecholamines US Medical PG Question 6: An investigator is studying the mechanism regulating pigment production in the skin. She has isolated a hormone produced by the anterior and intermediate lobe of the pituitary gland that stimulates neural crest-derived cells to produce pigments through the oxidation and polymerization of the amino acid tyrosine. This hormone is most likely cosecreted with a substance that acts on which of the following receptors?
- A. TSH receptor
- B. Glucocorticoid receptor
- C. Vasopressin receptor
- D. Dopamine receptor
- E. Mu receptor (Correct Answer)
Adrenal medulla and catecholamines Explanation: ***Mu receptor***
- The hormone described, which stimulates pigment production in neural crest-derived cells, is **melanocyte-stimulating hormone (MSH)**.
- **MSH** is derived from the pro-opiomelanocortin (POMC) precursor, which also gives rise to **β-endorphin**, a potent opioid peptide that acts on **mu opioid receptors**.
*TSH receptor*
- The **TSH receptor** binds thyroid-stimulating hormone (TSH), which primarily regulates thyroid hormone production and is not directly related to pigment production or opioid co-secretion from POMC.
- TSH is produced by the anterior pituitary but from a different lineage than POMC-derived hormones.
*Glucocorticoid receptor*
- The **glucocorticoid receptor** binds cortisol and other glucocorticoids, which are involved in stress response and metabolism.
- While ACTH (also derived from POMC) can stimulate adrenal glucocorticoid release, the question specifically refers to a substance *cosecreted* with MSH, not one that is *regulated* by MSH or its derivatives.
*Vasopressin receptor*
- **Vasopressin receptors** bind antidiuretic hormone (ADH), which regulates water balance and blood pressure.
- ADH is produced by the posterior pituitary (though synthesized in the hypothalamus) and is not cosecreted with MSH from the anterior/intermediate pituitary.
*Dopamine receptor*
- **Dopamine receptors** bind dopamine, a neurotransmitter involved in various functions, including the inhibition of prolactin release from the pituitary.
- While dopamine can influence pituitary function, it is not cosecreted with MSH in the manner described, nor is it a direct product of POMC cleavage.
Adrenal medulla and catecholamines US Medical PG Question 7: An endocrine surgeon wants to evaluate the risk of multiple endocrine neoplasia (MEN) type 2 syndromes in patients who experienced surgical hypertension during pheochromocytoma resection. She conducts a case-control study that identifies patients who experienced surgical hypertension and subsequently compares them to the control group with regard to the number of patients with underlying MEN type 2 syndromes. The odds ratio of MEN type 2 syndromes in patients with surgical hypertension during pheochromocytoma removal was 3.4 (p < 0.01). Given the rare disease assumption, this odds ratio can be interpreted as an approximation of the relative risk. The surgeon concludes that the risk of surgical hypertension during pheochromocytoma removal is 3.4 times greater in patients with MEN type 2 syndromes than in patients without MEN syndromes. This conclusion is best supported by which of the following assumptions?
- A. The case-control study used a large sample size
- B. The relationship between MEN syndromes and surgical hypertension is not due to random error
- C. Pheochromocytoma is common in MEN type 2 syndromes
- D. The 95% confidence interval for the odds ratio does not include 1.0
- E. Surgical hypertension associated with pheochromocytoma is rare (Correct Answer)
Adrenal medulla and catecholamines Explanation: ***Surgical hypertension associated with pheochromocytoma is rare***
- The phrase "given the **rare disease assumption**" is critical here, as it allows the **odds ratio** to approximate the **relative risk**. This assumption is valid when the outcome (surgical hypertension) is rare in the general population.
- If the outcome is rare, the odds ratio provides a good estimate of how many times more likely the outcome is in the exposed group compared to the unexposed group.
*The case-control study used a large sample size*
- A large sample size increases the **precision** of the estimate and the **statistical power** but does not inherently allow an odds ratio to be interpreted as a relative risk.
- While important for reliable results, sample size alone doesn't validate the "rare disease assumption."
*The relationship between MEN syndromes and surgical hypertension is not due to random error*
- This statement refers to the **statistical significance** of the findings (p < 0.01), indicating the observed effect is unlikely due to chance.
- It does not, however, relate to the specific condition under which an odds ratio approximates a relative risk.
*Pheochromocytoma is common in MEN type 2 syndromes*
- This statement addresses the prevalence of pheochromocytoma in patients with MEN type 2, not the rarity of the outcome (surgical hypertension) in the general population.
- While pheochromocytoma is indeed a feature of MEN2, this fact alone doesn't validate the rare disease assumption regarding surgical hypertension.
*The 95% confidence interval for the odds ratio does not include 1.0*
- This indicates **statistical significance**, meaning the odds ratio is significantly different from 1, suggesting an association between the exposure and the outcome.
- It does not provide the basis for interpreting the odds ratio as a relative risk under the rare disease assumption.
Adrenal medulla and catecholamines US Medical PG Question 8: An investigator is studying the principles of cell-to-cell signaling of the autonomic nervous system. It is found that the adrenal medulla has receptors that, when activated, result in the immediate opening of Na+, Ca2+, and K+ channels, which subsequently leads to the secretion of epinephrine and norepinephrine. These receptors are structurally most similar to which of the following receptors?
- A. Alpha 1 receptors of the bladder neck
- B. D2 receptors of the basal ganglia
- C. M2 receptors of heart
- D. NM receptors of the quadriceps femoris muscle (Correct Answer)
- E. H2 receptors of the stomach
Adrenal medulla and catecholamines Explanation: ***NM receptors of the quadriceps femoris muscle***
- The adrenal medulla's chromaffin cells are modified **postganglionic sympathetic neurons** that release catecholamines upon stimulation by preganglionic neurons.
- The activation of **Na+, Ca2+, and K+ channels** leading to rapid depolarization and neurotransmitter release is characteristic of **nicotinic acetylcholine receptors (NM type)**, which are ligand-gated ion channels.
*Alpha 1 receptors of the bladder neck*
- **Alpha-1 receptors** are **G-protein coupled receptors** that primarily activate phospholipase C, leading to increased intracellular calcium and smooth muscle contraction.
- Their activation does not directly result in the immediate opening of Na+, Ca2+, and K+ channels.
*D2 receptors of the basal ganglia*
- **D2 receptors** are **G-protein coupled receptors**, specifically inhibitory (Gi-coupled), that decrease adenylyl cyclase activity and reduce intracellular cAMP.
- They do not function as direct ligand-gated ion channels.
*M2 receptors of heart*
- **M2 receptors** are **G-protein coupled receptors** (Gi-coupled) that decrease heart rate by inhibiting adenylyl cyclase and opening potassium channels indirectly via G-protein subunits.
- While they affect ion channels, this is an indirect G-protein mediated process, not a direct ligand-gated ion channel mechanism.
*H2 receptors of the stomach*
- **H2 receptors** are **G-protein coupled receptors** (Gs-coupled) that increase adenylyl cyclase activity, leading to increased cAMP and stimulation of gastric acid secretion.
- They are not ligand-gated ion channels and do not directly open Na+, K+, and Ca2+ channels.
Adrenal medulla and catecholamines US Medical PG Question 9: A 9-year-old girl is admitted to the hospital with a one-day history of acute abdominal pain and vomiting. She also has a two-day history of fever, headache, and neck pain. Her immunizations are up-to-date. She is confused and oriented only to place and person. Her temperature is 39.7°C (103.5°F), pulse is 148/min, blood pressure is 90/50 mm Hg, and respiratory rate is 28/min. Cervical range of motion is limited by pain. The remainder of the neurologic examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.9 g/dL
Leukocyte count 44,000/mm3
Serum
pH 7.33
Na+ 130 mEq/L
Cl- 108 mEq/L
K+ 6.1 mEq/L
HCO3- 20 mEq/L
Urea nitrogen 34 mg/dL
Glucose 180 mg/dL
Creatinine 2.4 mg/dL
Urine ketones negative
A CT scan of the head shows enhancement of the arachnoid and pia mater. Cerebrospinal fluid analysis shows a leukocyte count of 3,400/μL (90% neutrophils), a glucose concentration of 50 mg/dL, protein concentration of 81 mg/dL, and no erythrocytes. Gram stain of the CSF shows gram-negative diplococci. This patient is at increased risk for which of the following complications?
- A. Vesicular skin eruptions
- B. Adrenal hemorrhage (Correct Answer)
- C. Pancreatitis
- D. Temporal lobe inflammation
- E. Deep neck abscess
Adrenal medulla and catecholamines Explanation: **Adrenal hemorrhage**
- The clinical picture of **fever, acute abdominal pain, confusion, hypotension, and a high WBC count (44,000/mm³)**, along with **Gram-negative diplococci in CSF**, indicates **meningococcal meningitis with sepsis**. This rapidly progressive infection by *Neisseria meningitidis* can lead to **Waterhouse-Friderichsen syndrome**, characterized by **adrenal hemorrhage** and profound shock.
- The **elevated potassium (6.1 mEq/L)** and **hyponatremia (130 mEq/L)** are consistent with **adrenal insufficiency** resulting from adrenal hemorrhage.
*Vesicular skin eruptions*
- **Vesicular skin eruptions** are characteristic of viral infections such as **herpes simplex virus (HSV)** or **varicella-zoster virus**, which would present differently (e.g., HSV encephalitis often causes temporal lobe involvement).
- While various infections can cause skin rashes, this specific presentation with extensive meningeal inflammation and septic shock points away from typical vesicular eruptions.
*Pancreatitis*
- **Pancreatitis** is characterized by severe epigastric pain radiating to the back, often with nausea and vomiting, and elevated lipase/amylase. While **abdominal pain** is present, other symptoms like **neck stiffness, confusion, and CSF findings of bacterial meningitis** are not typical for pancreatitis.
- There is no specific evidence, such as imaging findings or elevated pancreatic enzymes, to suggest pancreatitis in this case.
*Temporal lobe inflammation*
- **Temporal lobe inflammation** is a hallmark of **HSV encephalitis**, which often presents with seizures, bizarre behavior, and specific MRI findings in the temporal lobes. While a CT scan showed arachnoid and pia mater enhancement, this indicates **meningeal inflammation**, not specifically temporal lobe parenchymal inflammation (encephalitis).
- The presence of **Gram-negative diplococci in the CSF** strongly indicates bacterial meningitis, not viral encephalitis, making temporal lobe inflammation less likely.
*Deep neck abscess*
- A **deep neck abscess** would typically cause localized neck pain, swelling, dysphagia, and stridor, potentially with fever, but would not explain the widespread CNS symptoms (confusion, meningeal signs, CSF findings) or systemic signs of shock and coagulopathy seen here.
- While the patient has neck pain, it is due to **meningismus**, not a localized abscess, and there is no mention of local swelling or airway compromise.
Adrenal medulla and catecholamines US Medical PG Question 10: A 14-year-old girl presents with her mother to a physician's office. They are both concerned with the amount of hair growing on the girl's upper lip and cheeks. There are also sparse hairs on her chest. The mother reports that her daughter has not started menstruating either. The girl was born at 39 weeks gestation via spontaneous vaginal delivery. She is up to date on all vaccines and is meeting all developmental milestones. On examination, the patient is in the 55th percentile for her height. Her blood pressure is 90/50 mm Hg, pulse is 75/min, and respirations are 15/min. There is thin dark hair on her upper lip and on her cheeks. She also has pustular acne on her face and shoulders. Her breasts are in the initial stages of development and she speaks with a deep voice describing her concerns to the physician. Based on her clinical history, which of the following enzymes are most likely deficient?
- A. 17-α-hydroxylase
- B. 5-α-reductase
- C. 21-hydroxylase (Correct Answer)
- D. Aromatase
- E. 11-β-hydroxylase
Adrenal medulla and catecholamines Explanation: ***21-hydroxylase***
- **21-hydroxylase deficiency** is the most common cause of congenital adrenal hyperplasia (CAH), leading to a buildup of **androgen precursors**.
- The patient's symptoms of **hirsutism** (upper lip, cheeks, chest hair), **acne**, **deep voice**, and **primary amenorrhea** are all consistent with **virilization** due to excess androgens.
*17-α-hydroxylase*
- **17-α-hydroxylase deficiency** impairs the production of all sex steroids and cortisol, leading to **hypertension**, **hypokalemia**, and **female pseudohermaphroditism** in XY individuals or **lack of secondary sexual characteristics** in XX individuals.
- This patient presents with signs of **androgen excess**, not deficiency, and her blood pressure is normal, making 17-α-hydroxylase deficiency an unlikely diagnosis.
*5-α-reductase*
- **5-α-reductase deficiency** prevents the conversion of **testosterone to dihydrotestosterone (DHT)**, affecting external male genitalia development but not adrenal steroid synthesis.
- This typically presents as **ambiguous genitalia** in males (XY individuals) but would not cause the signs of **virilization** and **amenorrhea** observed in this female patient.
*Aromatase*
- **Aromatase deficiency** prevents the conversion of androgens to estrogens, leading to **virilization** in XX individuals due to unopposed androgen action.
- While it can manifest with similar symptoms of **hirsutism** and **amenorrhea**, it is much rarer than 21-hydroxylase deficiency and doesn't explain the potential for **adrenal crisis** issues associated with CAH.
*11-β-hydroxylase*
- **11-β-hydroxylase deficiency** leads to an accumulation of **11-deoxycorticosterone (DOC)**, causing **hypertension** and **virilization** due to increased androgen production.
- While virilization is present, the patient's **normal blood pressure** (90/50 mm Hg) makes this diagnosis less likely compared to 21-hydroxylase deficiency, which typically presents with normal or low blood pressure (salt-wasting forms) unless a salt-retaining form is present.
More Adrenal medulla and catecholamines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.