T wave and repolarization US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for T wave and repolarization. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
T wave and repolarization US Medical PG Question 1: A 70-year-old man presents to his primary care physician for a general checkup. He states that he has been doing well and taking his medications as prescribed. He recently started a new diet and supplement to improve his health and has started exercising. The patient has a past medical history of diabetes, a myocardial infarction, and hypertension. He denies any shortness of breath at rest or with exertion. An ECG is performed and is within normal limits. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 6.7 mEq/L
HCO3-: 25 mEq/L
Glucose: 133 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Medication (Correct Answer)
- B. Acute renal failure
- C. Hemolysis
- D. Dietary changes
- E. Rhabdomyolysis
T wave and repolarization Explanation: ***Medication***
- The patient's **hyperkalemia** (K+ 6.7 mEq/L) despite feeling well, suggests a common side effect of medications, particularly those used for his pre-existing conditions like **hypertension** (**ACE inhibitors**, **ARBs**, **spironolactone**) and **diabetes**.
- Medications are a frequent cause of asymptomatic electrolyte abnormalities, and given his complex medical history and the absence of acute symptoms, this is the most likely culprit.
*Acute renal failure*
- While acute renal failure can cause **hyperkalemia**, it typically presents with other symptoms such as **oliguria**, **fluid retention**, or other signs of organ dysfunction, which are not described.
- The patient is reported to be "doing well" without **shortness of breath** or other acute complaints, making acute renal failure less likely as the primary cause of isolated hyperkalemia.
*Hemolysis*
- **Hemolysis** can release intracellular potassium, leading to **pseudohyperkalemia**, but it would typically be suspected in cases of **blood draw errors** or conditions causing red blood cell breakdown, none of which are indicated.
- The patient's presentation does not include any signs or symptoms suggestive of red cell destruction.
*Dietary changes*
- While an extremely **high-potassium diet** or certain **supplements** could contribute to hyperkalemia, it is less common for dietary changes alone to cause such a significant elevation in a patient with normal organ function.
- Given his medical history, medication-induced hyperkalemia is a more direct and common explanation.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves the breakdown of muscle tissue, releasing potassium and other intracellular contents, but it is usually associated with significant **muscle pain**, **weakness**, and elevated **creatine kinase**.
- The patient denies these symptoms and has no other indicators pointing towards severe muscle injury.
T wave and repolarization US Medical PG Question 2: A 67-year-old man comes to the emergency department because of retrosternal chest pressure and shortness of breath for 4 hours. The symptoms started while he was walking to work and have only minimally improved with rest. He has a history of type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 35 years. He appears uncomfortable. His pulse is 95/min. Serum studies show a normal troponin concentration. An ECG shows no abnormalities. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Atherosclerotic plaque thrombus with complete coronary artery occlusion
- B. Stable atherosclerotic plaque with 85% coronary artery occlusion
- C. Aortic valve thickening and calcification
- D. Disruption of an atherosclerotic plaque with a non-occlusive coronary artery thrombus (Correct Answer)
- E. Coronary artery occlusion due to transient increase in vascular tone
T wave and repolarization Explanation: **Disruption of an atherosclerotic plaque with a non-occlusive coronary artery thrombus**
- This scenario describes **unstable angina (UA)**, characterized by chest pain at rest or with minimal exertion, increased frequency/intensity of angina, or new-onset severe angina.
- While troponin is normal and ECG shows no abnormalities, the persistent symptoms and minimal improvement with rest, along with risk factors like **diabetes** and **smoking**, strongly suggest an **unstable coronary lesion** that is not yet fully occlusive.
*Atherosclerotic plaque thrombus with complete coronary artery occlusion*
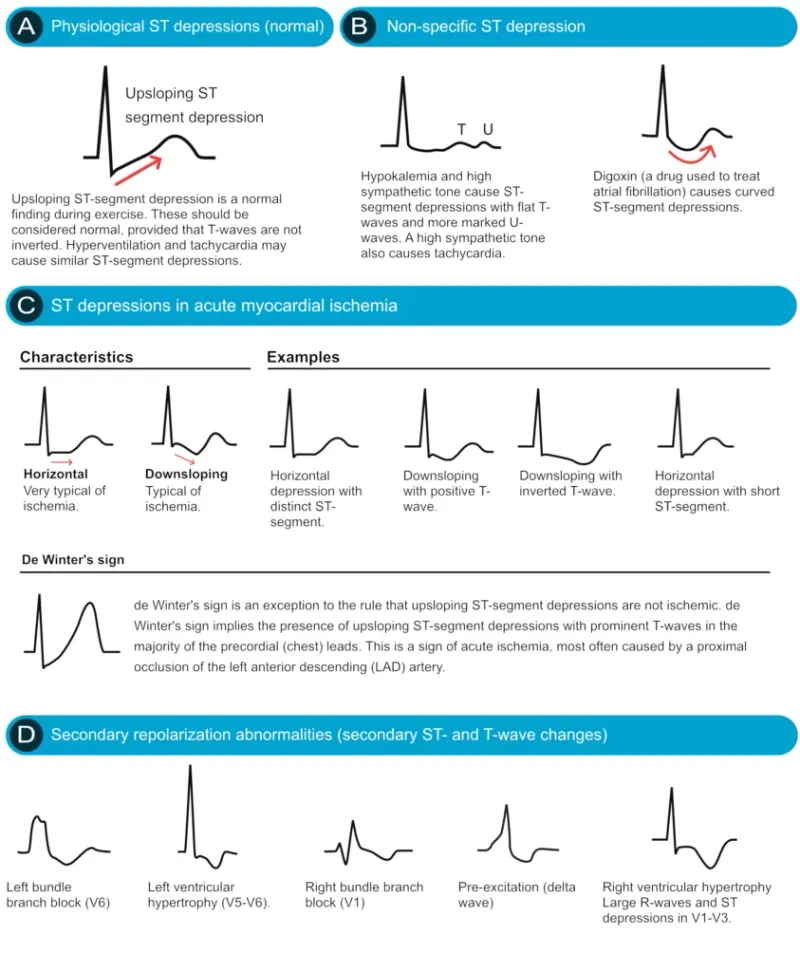
- **Complete coronary artery occlusion** typically leads to myocardial infarction (MI), which would manifest with **elevated troponin levels** and often **ECG changes** (e.g., ST elevation or depression).
- The patient's normal troponin and ECG rule out an acute MI at this stage.
*Stable atherosclerotic plaque with 85% coronary artery occlusion*
- **Stable angina** symptoms usually improve promptly with rest and are predictable, occurring only during significant exertion.
- The described symptoms, including minimal improvement with rest and 4 hours duration, are not typical of stable angina.
*Aortic valve thickening and calcification*
- While **aortic stenosis** can cause chest pain and shortness of breath, these symptoms are typically exertional and not usually described as "retrosternal pressure" that minimally improves with rest in this acute context without other signs of flow obstruction.
- This condition is unlikely to be the sole cause of these acute, persistent symptoms without findings on initial workup.
*Coronary artery occlusion due to transient increase in vascular tone*
- **Coronary vasospasm** (Prinzmetal angina) can cause chest pain at rest and transient ECG changes, but it's typically **recurrent** and responds well to **vasodilators**.
- This patient's symptoms, combined with risk factors for atherosclerosis and the prolonged nature of the pain, are less indicative of vasospasm as the primary underlying cause.
T wave and repolarization US Medical PG Question 3: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
T wave and repolarization Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
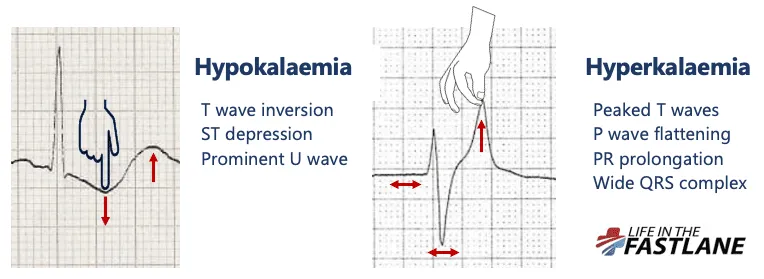
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
T wave and repolarization US Medical PG Question 4: A 32-year-old woman is hospitalized after developing an allergic reaction to the contrast medium used for a cerebral angiography. The study was initially ordered as part of the diagnostic approach of a suspected case of pseudotumor cerebri. Her medical history is unremarkable. On physical examination she has stable vital signs, a diffuse maculopapular rash over her neck and chest, and a mild fever. She is started on hydrocortisone and monitored for the next 8 hours. After the monitoring period, a laboratory test shows significant azotemia. The patient complains of generalized weakness and palpitations. Tall-peaked T waves are observed on ECG. Which of the following explains this clinical manifestation?
- A. Anemia
- B. Platelet dysfunction
- C. Uremic pericarditis
- D. Metabolic acidosis
- E. Hyperkalemia (Correct Answer)
T wave and repolarization Explanation: ***Hyperkalemia***
- The combination of **significant azotemia** (indicating acute kidney injury), **generalized weakness**, and **peaked T waves on ECG** are classic signs of hyperkalemia.
- The allergic reaction and subsequent treatment may have exacerbated kidney dysfunction, leading to impaired potassium excretion and subsequent elevated serum potassium levels.
*Anemia*
- While anemia can cause weakness and palpitations, it does not typically manifest with **peaked T waves** on ECG or directly explain the presence of **azotemia**.
- Anemia is common in chronic kidney disease but is not the primary cause of acute symptoms and ECG changes described here.
*Platelet dysfunction*
- Uremia can lead to **platelet dysfunction**, causing bleeding tendencies, but it does not account for the **generalized weakness**, **azotemia**, or the characteristic **peaked T waves** on ECG.
- Platelet dysfunction is typically associated with bruising or prolonged bleeding, not the cardiovascular and neurological symptoms observed.
*Uremic pericarditis*
- **Uremic pericarditis** can cause chest pain, a friction rub, and sometimes palpitations, but it does not directly explain the **peaked T waves** or generalized weakness in the context of acute azotemia.
- The primary symptoms of pericarditis are often related to inflammation of the pericardium rather than electrolyte imbalances.
*Metabolic acidosis*
- **Metabolic acidosis** is common in acute kidney injury and can contribute to weakness and dyspnea, but it does not directly cause **peaked T waves** on ECG.
- While clinically important, acidosis itself doesn't explain the specific ECG findings, which are more indicative of hyperkalemia.
T wave and repolarization US Medical PG Question 5: An abnormal wave is noted on a routine ECG. The wave in question represents which of the following electrical events in the cardiac cycle?
- A. Period between ventricular depolarization and repolarization
- B. Atrial repolarization
- C. Ventricular repolarization (Correct Answer)
- D. Ventricular depolarization
- E. Atrial depolarization
T wave and repolarization Explanation: ***Ventricular repolarization***
- The **T wave** represents ventricular repolarization, which is the electrical recovery phase of the ventricles after contraction
- T wave abnormalities are among the most common ECG findings and include **T wave inversions** (myocardial ischemia, ventricular hypertrophy), **peaked T waves** (hyperkalemia), **flattened T waves** (hypokalemia, ischemia), and **biphasic T waves**
- The T wave corresponds to **phase 3** of the ventricular action potential when potassium channels open and the membrane repolarizes
*Period between ventricular depolarization and repolarization*
- This describes the **ST segment**, which represents the period when ventricles are completely depolarized before repolarization begins
- The **QT interval** encompasses both ventricular depolarization and repolarization (QRS + ST segment + T wave)
- These are intervals or segments, not waves
*Atrial repolarization*
- Atrial repolarization occurs during ventricular depolarization and is represented by the **Ta wave**
- This wave is typically **not visible** on standard ECG because it is **masked by the much larger QRS complex** and has very low amplitude
- It cannot be identified as a distinct wave on routine ECGs
*Ventricular depolarization*
- The **QRS complex** represents ventricular depolarization, the electrical activation that triggers ventricular contraction
- Normal QRS duration is **0.06-0.10 seconds** (3 small boxes or less)
- QRS abnormalities include bundle branch blocks, ventricular hypertrophy patterns, and pre-excitation
*Atrial depolarization*
- The **P wave** represents atrial depolarization, the electrical activation that triggers atrial contraction
- Normal P wave characteristics: **upright in leads I, II, aVF**; duration less than 0.12 seconds; amplitude less than 2.5 mm
- P wave abnormalities include left atrial enlargement (broad, notched P waves) and right atrial enlargement (tall, peaked P waves)
T wave and repolarization US Medical PG Question 6: A 17-year-old girl suddenly grabs her chest and collapses to the ground while playing volleyball at school. The teacher rushes to evaluate the situation and finds that the girl has no pulse and is not breathing. He starts chest compressions. An automated external defibrillator (AED) is brought to the scene within 3 minutes and a shock is delivered. The girl regains consciousness and regular sinus rhythm. She is rushed to the emergency department. The vital signs include: blood pressure 122/77 mm Hg and pulse 65/min. The pulse is regular. An electrocardiogram (ECG) shows a shortened PR interval, a wide QRS complex, a delta wave, and an inverted T wave. Which of the following is the most likely pathology in the conduction system of this patient’s heart?
- A. Impulse generation by tissue in atrioventricular node
- B. Accessory pathway from atria to ventricles (Correct Answer)
- C. Automatic discharge of irregular impulses in the atria
- D. Wandering atrial pacemaker
- E. Blockage in conduction pathway
T wave and repolarization Explanation: ***Accessory pathway from atria to ventricles***
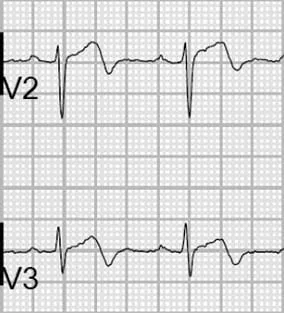
- The ECG findings of a **shortened PR interval**, **delta wave**, and **wide QRS complex** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, which involves an **accessory pathway** (Bundle of Kent) bypassing the AV node.
- This accessory pathway allows for pre-excitation of the ventricles, predisposing patients to **tachyarrhythmias** like the one experienced by the patient (sudden cardiac arrest).
*Impulse generation by tissue in atrioventricular node*
- This describes a **junctional rhythm**, which would present with a **normal or long PR interval** and a **narrow QRS complex**, contrasting with the given ECG findings.
- A junctional rhythm typically results in a slower heart rate and is not generally associated with sudden cardiac arrest in healthy individuals.
*Automatic discharge of irregular impulses in the atria*
- This typically refers to **atrial fibrillation** or multifocal atrial tachycardia, which would show an **irregularly irregular rhythm** or multiple P-wave morphologies, not the specific PR and QRS abnormalities seen.
- While atrial fibrillation can occur with WPW, the primary pathology described by the ECG findings is the accessory pathway itself.
*Wandering atrial pacemaker*
- A **wandering atrial pacemaker** is characterized by varying P-wave morphology and PR intervals as the pacemaker shifts between different atrial sites, but it generally maintains a normal QRS duration.
- It is typically a benign arrhythmia and does not cause the pre-excitation or the risk of sudden cardiac death seen in this patient.
*Blockage in conduction pathway*
- A **blockage in the conduction pathway** (e.g., AV block) would result in a **prolonged PR interval** or dropped QRS complexes, which is the opposite of the shortened PR interval observed.
- While heart block can cause syncope, it wouldn't explain the pre-excitation pattern (delta wave, wide QRS) seen in the ECG.
T wave and repolarization US Medical PG Question 7: In the coronary steal phenomenon, vessel dilation is paradoxically harmful because blood is diverted from ischemic areas of the myocardium. Which of the following is responsible for the coronary steal phenomenon?
- A. Venodilation
- B. Microvessel dilation (Correct Answer)
- C. Dilation of the large coronary arteries
- D. Systemic arterial dilation
- E. Volume loss of fluid in the periphery
T wave and repolarization Explanation: ***Microvessel dilation***
- The coronary steal phenomenon occurs when **vasodilators** are administered, causing dilation of **healthy coronary microvessels** and a decrease in resistance.
- This preferentially diverts blood flow away from already **ischemic areas** with maximally dilated intrinsic microvessels, worsening myocardial ischemia.
*Venodilation*
- **Venodilation** primarily reduces **preload** by increasing venous capacitance, not by directly altering coronary microcirculatory blood flow distribution in a way that causes "steal."
- While some vasodilators have venodilatory effects, this specific effect is not the mechanism behind coronary steal.
*Dilation of the large coronary arteries*
- Dilation of large coronary arteries alone doesn't cause the "steal" but rather improves overall blood flow. The critical issue is the differential response of **collateral** and **non-collateral microvessels**.
- **Stenoses** in large coronary arteries are the underlying pathology, but the steal phenomenon itself results from changes in **downstream microvascular resistance**.
*Systemic arterial dilation*
- **Systemic arterial dilation** primarily reduces afterload and can lower blood pressure, but it does not specifically explain the redistribution of coronary blood flow to the detriment of ischemic zones within the myocardium.
- The key to coronary steal is the **heterogeneity of response** at the microvascular level within the coronary circulation.
*Volume loss of fluid in the periphery*
- **Volume loss** in the periphery would influence overall circulatory dynamics and cardiac output but is not directly responsible for the **localized myocardial blood flow redistribution** characteristic of the coronary steal phenomenon.
- Coronary steal is a physiological process related to **vasoreactivity** and not hypovolemia.
T wave and repolarization US Medical PG Question 8: An investigator develops a new drug that decreases the number of voltage-gated potassium channels in cardiac muscle cell membranes. Which of the following is the most likely effect of this drug on the myocardial action potential?
- A. Delayed repolarization (Correct Answer)
- B. Delayed depolarization
- C. Accelerated repolarization
- D. Decreased resting membrane potential
- E. Accelerated depolarization
T wave and repolarization Explanation: ***Delayed repolarization***
- **Voltage-gated potassium channels** are primarily responsible for the efflux of potassium ions during the **repolarization phase** (phase 3) of the cardiac action potential.
- A decrease in the number of these channels would reduce potassium efflux, thus slowing down the repolarization process and prolonging the **action potential duration**.
*Delayed depolarization*
- **Depolarization** (phase 0) of the cardiac action potential is primarily mediated by the rapid influx of **sodium ions** through voltage-gated sodium channels.
- Changes in potassium channels do not directly affect the speed of depolarization.
*Accelerated repolarization*
- Accelerated repolarization would occur if there were an *increase* in the number or activity of **potassium channels**, leading to a faster efflux of potassium ions.
- A *decrease* in these channels would have the opposite effect.
*Decreased resting membrane potential*
- The **resting membrane potential** is primarily maintained by the **leak potassium channels** and the **Na+/K+ ATPase pump**, not directly by voltage-gated potassium channels involved in repolarization.
- A decrease in voltage-gated potassium channels would not significantly alter the resting membrane potential.
*Accelerated depolarization*
- Accelerated depolarization would result from an *increase* in the speed or magnitude of **sodium influx** during phase 0.
- A reduction in potassium channels has no direct impact on the rate of sodium channel activation or current.
T wave and repolarization US Medical PG Question 9: A 55-year-old man presents to his physician with weakness and fatigue for 1 week. There is no significant past medical history. He mentions that he is very health conscious and has heard about the health benefits of juices. He is following a juice-only diet for the last 2 weeks. His physical examination is completely normal, except for depressed deep tendon reflexes. The only abnormality in a complete laboratory evaluation is a serum potassium level of 6.0 mEq/L (6.0 mmol/L). There are significantly peaked T-waves on ECG. Which of the following pathophysiologic mechanisms best explains the patient’s symptoms?
- A. Decreased resting membrane potential of skeletal muscle cells (Correct Answer)
- B. Prolonged release of Ca2+ ions after stimulation of Ryanodine receptors
- C. Hyperpolarization of skeletal muscle cells
- D. Dysfunction of Na+ channels
- E. Dysfunction of dystrophin-glycoprotein complex
T wave and repolarization Explanation: ***Decreased resting membrane potential of skeletal muscle cells***
- The patient's **hyperkalemia** (serum potassium 6.0 mEq/L), evidenced by peaked T-waves, reduces the electrochemical gradient for potassium, making the **resting membrane potential less negative (more depolarized)**.
- While seemingly contradictory, a persistent partial depolarization due to high extracellular potassium can lead to inactivation of voltage-gated sodium channels, preventing the generation of new action potentials and causing **muscle weakness and depressed reflexes**.
*Prolonged release of Ca2+ ions after stimulation of Ryanodine receptors*
- This mechanism is associated with conditions like **malignant hyperthermia** or certain myopathies, characterized by muscle rigidity, cramps, or excessive heat production, which are not seen here.
- Hyperkalemia primarily affects **membrane excitability** rather than intracellular calcium release pathways directly.
*Hyperpolarization of skeletal muscle cells*
- **Hyperpolarization** would make the resting membrane potential more negative, making it harder to reach the threshold for an action potential, leading to weakness.
- This typically occurs in conditions causing **hypokalemia**, as a lower extracellular potassium concentration increases the electrochemical gradient and causes a net efflux of potassium ions.
*Dysfunction of Na+ channels*
- Dysfunction of **sodium channels** can cause various neuromuscular disorders, including periodic paralysis or myotonic conditions.
- While hyperkalemia indirectly affects sodium channel function by altering the resting membrane potential, the primary pathophysiologic insult here is the altered potassium gradient, not an intrinsic channel defect.
*Dysfunction of dystrophin-glycoprotein complex*
- This complex is crucial for maintaining muscle fiber integrity and is defective in **muscular dystrophies** (e.g., Duchenne muscular dystrophy).
- Such conditions cause progressive muscle degeneration and weakness, which develop over a much longer period than the acute symptoms described here and are not related to electrolyte imbalances.
More T wave and repolarization US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.