ST segment evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ST segment evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ST segment evaluation US Medical PG Question 1: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
ST segment evaluation Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
ST segment evaluation US Medical PG Question 2: A 43-year-old woman presents to a physician with weakness and fatigue for a week. She mentions that she has been taking oral fluconazole for the last 4 weeks for the treatment of tinea capitis. She also says that she loves coffee and usually consumes 4–6 cups of coffee every day. On physical examination, her vital signs are stable and examination of all systems, including nervous system, is normal. Her laboratory evaluation reveals that her serum potassium level is 3.1 mmol/L (3.1 mEq/L). The physician orders an ECG. Which of the following findings is most likely to be present?
- A. Shortened QT interval
- B. Tall peaked T waves
- C. Disappearing P waves
- D. Depression of ST segment (Correct Answer)
- E. Widening of QRS complexes
ST segment evaluation Explanation: ***Depression of ST segment***
- The patient presents with **hypokalemia** (serum potassium 3.1 mmol/L), which is commonly associated with **ST segment depression** on an ECG.
- Fluconazole can cause hypokalemia, and coffee consumption can exacerbate it due to its diuretic effect, further contributing to the likelihood of this ECG finding.
*Shortened QT interval*
- A **shortened QT interval** is typically associated with **hypercalcemia** rather than hypokalemia.
- Hypokalemia is more commonly associated with **QT prolongation** or prominent U waves, not shortening.
*Tall peaked T waves*
- **Tall, peaked T waves** are characteristic of **hyperkalemia**, which is the opposite of the patient's condition.
- In hypokalemia, T waves tend to be flattened or inverted.
*Disappearing P waves*
- **Disappearing P waves** are often seen in conditions like **atrial fibrillation** or severe hyperkalemia, where atrial activity is affected.
- They are not a characteristic finding of hypokalemia.
*Widening of QRS complexes*
- **Widening of QRS complexes** is typically associated with conditions like **bundle branch blocks**, certain intoxications, or severe **hyperkalemia**, not hypokalemia.
- Hypokalemia does not directly lead to a widened QRS complex.
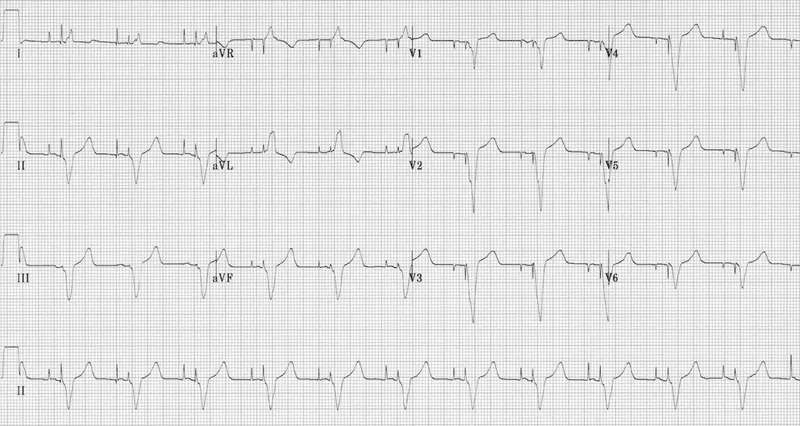
ST segment evaluation US Medical PG Question 3: A 71-year-old man presents to the emergency department with severe substernal chest pain. An initial EKG demonstrates ST elevation in leads V2, V3, V4, and V5 with reciprocal changes. The patient is started on aspirin and heparin and is transferred to the cardiac catheterization lab. The patient recovers over the next several days. On the floor, the patient complains of feeling very fatigued and feels too weak to ambulate even with the assistance of physical therapy. Chest radiography reveals an enlarged cardiac silhouette with signs of fluid bilaterally in the lung bases. His temperature is 98.4°F (36.9°C), blood pressure is 85/50 mmHg, pulse is 110/min, respirations are 13/min, and oxygen saturation is 97% on room air. Which of the following would be expected to be seen in this patient?
- A. Decreased systemic vascular resistance
- B. Increased venous oxygen content
- C. Increased ejection fraction
- D. Decreased tissue oxygen extraction
- E. Increased pulmonary capillary wedge pressure (Correct Answer)
ST segment evaluation Explanation: ***Increased pulmonary capillary wedge pressure***
- The patient's symptoms of **fatigue**, **weakness**, **hypotension**, **tachycardia**, and **pulmonary congestion** (enlarged cardiac silhouette, bilateral pleural effusions) after a significant myocardial infarction are highly suggestive of **cardiogenic shock**.
- In cardiogenic shock, the heart's pumping ability is severely compromised, leading to **increased end-diastolic filling pressures** in the left ventricle, which is reflected as an elevated **pulmonary capillary wedge pressure (PCWP)**.
*Decreased systemic vascular resistance*
- **Decreased systemic vascular resistance (SVR)** is a hallmark of **distributive shock**, such as septic shock, where widespread vasodilation occurs.
- In **cardiogenic shock**, the body typically tries to compensate for reduced cardiac output by **increasing SVR** to maintain blood pressure, although this compensation may be overwhelmed, leading to hypotension.
*Increased venous oxygen content*
- **Increased mixed venous oxygen saturation (SvO2)** or **venous oxygen content** is seen when tissues are not adequately extracting oxygen, either due to shunt physiology or when oxygen delivery far exceeds demand.
- In **cardiogenic shock**, tissue oxygen demand often exceeds delivery due to severely impaired cardiac output, leading to **increased oxygen extraction** by tissues and thus **decreased venous oxygen content**.
*Increased ejection fraction*
- The patient experienced a **large myocardial infarction (ST elevation in V2-V5)**, indicating substantial damage to the left ventricle.
- This damage would severely impair the heart's pumping function, leading to a **decreased ejection fraction**, which is characteristic of **cardiogenic shock**.
*Decreased tissue oxygen extraction*
- **Decreased tissue oxygen extraction** would imply that tissues are not properly utilizing the delivered oxygen, or that oxygen delivery is so high that tissues don't need to extract as much.
- In **cardiogenic shock**, cardiac output is severely reduced, leading to **inadequate oxygen delivery** to tissues, forcing them to **maximally extract oxygen** from the blood to meet metabolic demands.
ST segment evaluation US Medical PG Question 4: A 61-year-old man is brought to the emergency department by ambulance because of severe retrosternal chest pain and shortness of breath for 30 minutes. Paramedics report that an ECG recorded en route to the hospital showed ST-segment elevation in I, aVL, and the precordial leads. On arrival, the patient is unresponsive to painful stimuli. Examination shows neither respiration nor pulse. Despite appropriate lifesaving measures, he dies 10 minutes later. Which of the following is the most likely cause of death in this patient?
- A. Left ventricular failure
- B. Cardiac free wall rupture
- C. Ventricular fibrillation (Correct Answer)
- D. Ventricular aneurysm
- E. Hemorrhagic stroke
ST segment evaluation Explanation: ***Ventricular fibrillation***
- The rapid onset of symptoms, severe chest pain, ST-segment elevation myocardial infarction (STEMI) involving extensive leads (I, aVL, and precordial), and sudden cardiac arrest without pulse or respiration strongly indicate a **malignant arrhythmia**, specifically ventricular fibrillation.
- In a STEMI, **ischemia** can rapidly trigger electrical instability in the myocardium, leading to disorganized electrical activity and immediate hemodynamic collapse.
*Left ventricular failure*
- While a large anterior STEMI could lead to **left ventricular failure**, the patient's immediate collapse and absence of respiration and pulse suggest sudden electrical rather than mechanical failure.
- **Left ventricular failure** typically manifests with progressive symptoms like severe dyspnea, pulmonary edema, and cardiogenic shock, which often allows for some period of clinical deterioration before death.
*Cardiac free wall rupture*
- **Cardiac free wall rupture** is a mechanical complication of MI that usually occurs several days post-infarction, though it can rarely occur acutely.
- It typically presents with **sudden severe chest pain**, hypotension, and rapid death due to **cardiac tamponade**, but the immediate timeline and ECG findings of extensive STEMI followed by sudden arrest are more consistent with an electrical event.
*Ventricular aneurysm*
- A **ventricular aneurysm** is a late complication of an MI, developing weeks to months after the event.
- It presents with symptoms like **heart failure**, arrhythmias, or mural thrombus formation, not as an acute cause of death within minutes of symptom onset.
*Hemorrhagic stroke*
- A **hemorrhagic stroke** would present with sudden neurological deficits, such as severe headache, altered consciousness, and focal neurological signs.
- While it can cause sudden death, the prominent chest pain and the ECG findings of widespread ST-segment elevation are indicative of a primary cardiac event.
ST segment evaluation US Medical PG Question 5: A 50-year-old man presents the emergency department for intense chest pain, profuse sweating, and shortness of breath. The onset of these symptoms was 3 hours ago. The chest pain began after a heated discussion with a colleague at the community college where he is employed. Upon arrival, he is found conscious and responsive; the vital signs include a blood pressure of 130/80 mm Hg, a heart rate at 90/min, a respiratory rate at 20/min, and a body temperature of 36.4°C (97.5°F). His medical history is significant for hypertension diagnosed 7 years ago, which is well-controlled with a calcium channel blocker. The initial electrocardiogram (ECG) shows ST-segment depression in multiple consecutive leads, an elevated cardiac troponin T level, and normal kidney function. Which of the following would you expect to find in this patient?
- A. Subendocardial necrosis (Correct Answer)
- B. Transmural necrosis
- C. Incomplete occlusion of a coronary artery
- D. Coronary artery spasm
- E. Ventricular pseudoaneurysm
ST segment evaluation Explanation: ***Subendocardial necrosis***
- This patient's presentation with **ST-segment depression** and **elevated troponin T** indicates a **Non-ST-segment Elevation Myocardial Infarction (NSTEMI)**, which typically results from subendocardial ischemia and necrosis.
- Subendocardial tissue is most vulnerable to ischemia due to its high oxygen demand and distal location from the coronary arteries, making it the first region to suffer damage when oxygen supply is compromised.
*Transmural necrosis*
- **Transmural necrosis** is characteristic of a **ST-segment Elevation Myocardial Infarction (STEMI)**, which presents with persistent **ST-segment elevation** on ECG.
- This patient's ECG shows **ST-segment depression**, ruling out transmural involvement at the time of presentation.
*Incomplete occlusion of a coronary artery*
- While an NSTEMI usually involves an **incomplete occlusion** or **critical stenosis** of a coronary artery, the question asks what would be *found* in the patient's heart tissue, not the mechanism.
- The direct tissue consequence of incomplete occlusion leading to NSTEMI is **subendocardial necrosis**, which is a more specific answer about the pathological finding.
*Coronary artery spasm*
- Although **coronary artery spasm (Prinzmetal angina)** can cause chest pain and ECG changes, it typically presents with **transient ST-segment elevation** (not depression) and often resolves spontaneously.
- The elevated troponin T indicates myocardial necrosis, which is not typically a feature of uncomplicated coronary artery spasm, and the duration of symptoms (3 hours) suggests a more sustained event than a transient spasm.
*Ventricular pseudoaneurysm*
- A **ventricular pseudoaneurysm** is a **late complication of myocardial infarction**, typically occurring weeks to months after the acute event, due to rupture of the ventricular free wall contained by pericardium.
- Given the 3-hour symptom onset, it is highly unlikely to be present in the acute phase of myocardial infarction.
ST segment evaluation US Medical PG Question 6: A 55-year-old man comes to the emergency department because of left-sided chest pain and difficulty breathing for the past 30 minutes. His pulse is 88/min. He is pale and anxious. Serum studies show increased cardiac enzymes. An ECG shows ST-elevations in leads I, aVL, and V5-V6. A percutaneous coronary intervention is performed. In order to localize the site of the lesion, the catheter must pass through which of the following structures?
- A. Left coronary artery → left circumflex artery (Correct Answer)
- B. Right coronary artery → posterior descending artery
- C. Left coronary artery → left anterior descending artery
- D. Right coronary artery → right marginal artery
- E. Left coronary artery → posterior descending artery
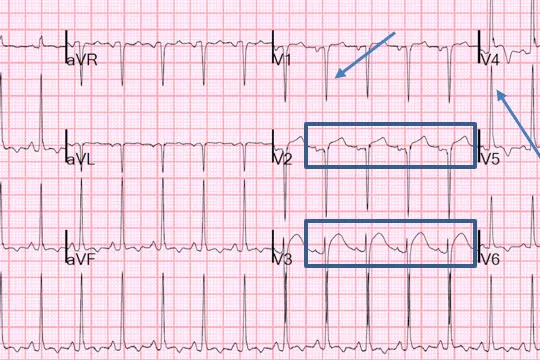
ST segment evaluation Explanation: ***Left coronary artery → left circumflex artery***
- **ST-elevations** in leads I, aVL, and V5-V6 are indicative of a **lateral myocardial infarction**.
- The **left circumflex artery** primarily supplies the lateral wall of the left ventricle.
*Right coronary artery → posterior descending artery*
- The **posterior descending artery** (PDA) typically supplies the inferior wall and posterior interventricular septum.
- An occlusion here would cause **ST-elevations** in leads II, III, and aVF, which is not seen in this case.
*Left coronary artery → left anterior descending artery*
- The **left anterior descending** (LAD) artery supplies the anterior wall and apex of the left ventricle.
- Occlusion of the LAD would typically cause **ST-elevations** in leads V1-V4, indicating an anterior MI.
*Right coronary artery → right marginal artery*
- The **right marginal artery** is a branch of the right coronary artery and supplies part of the right ventricle.
- Occlusion here would primarily affect the **right ventricle**, and is not typically associated with the given ECG changes.
*Left coronary artery → posterior descending artery*
- While the **posterior descending artery** can sometimes originate from the left circumflex artery (**left dominant circulation**), it primarily supplies the inferior wall.
- The observed ECG changes in leads I, aVL, and V5-V6 are characteristic of a **lateral wall infarct**, which is supplied by the left circumflex artery.
ST segment evaluation US Medical PG Question 7: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
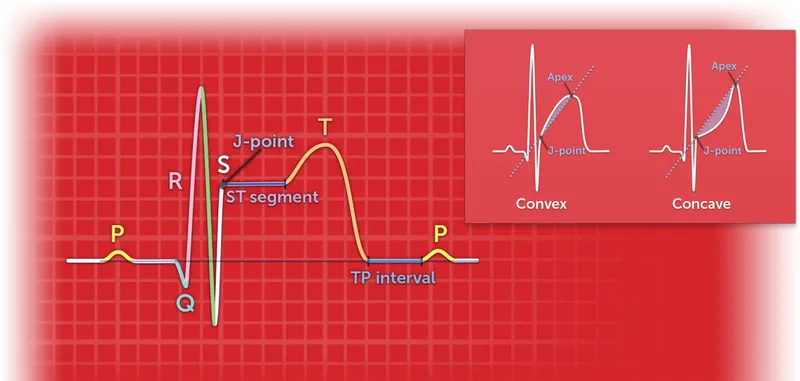
ST segment evaluation Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
ST segment evaluation US Medical PG Question 8: In the coronary steal phenomenon, vessel dilation is paradoxically harmful because blood is diverted from ischemic areas of the myocardium. Which of the following is responsible for the coronary steal phenomenon?
- A. Venodilation
- B. Microvessel dilation (Correct Answer)
- C. Dilation of the large coronary arteries
- D. Systemic arterial dilation
- E. Volume loss of fluid in the periphery
ST segment evaluation Explanation: ***Microvessel dilation***
- The coronary steal phenomenon occurs when **vasodilators** are administered, causing dilation of **healthy coronary microvessels** and a decrease in resistance.
- This preferentially diverts blood flow away from already **ischemic areas** with maximally dilated intrinsic microvessels, worsening myocardial ischemia.
*Venodilation*
- **Venodilation** primarily reduces **preload** by increasing venous capacitance, not by directly altering coronary microcirculatory blood flow distribution in a way that causes "steal."
- While some vasodilators have venodilatory effects, this specific effect is not the mechanism behind coronary steal.
*Dilation of the large coronary arteries*
- Dilation of large coronary arteries alone doesn't cause the "steal" but rather improves overall blood flow. The critical issue is the differential response of **collateral** and **non-collateral microvessels**.
- **Stenoses** in large coronary arteries are the underlying pathology, but the steal phenomenon itself results from changes in **downstream microvascular resistance**.
*Systemic arterial dilation*
- **Systemic arterial dilation** primarily reduces afterload and can lower blood pressure, but it does not specifically explain the redistribution of coronary blood flow to the detriment of ischemic zones within the myocardium.
- The key to coronary steal is the **heterogeneity of response** at the microvascular level within the coronary circulation.
*Volume loss of fluid in the periphery*
- **Volume loss** in the periphery would influence overall circulatory dynamics and cardiac output but is not directly responsible for the **localized myocardial blood flow redistribution** characteristic of the coronary steal phenomenon.
- Coronary steal is a physiological process related to **vasoreactivity** and not hypovolemia.
ST segment evaluation US Medical PG Question 9: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
ST segment evaluation Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
ST segment evaluation US Medical PG Question 10: An investigator develops a new drug that decreases the number of voltage-gated potassium channels in cardiac muscle cell membranes. Which of the following is the most likely effect of this drug on the myocardial action potential?
- A. Delayed repolarization (Correct Answer)
- B. Delayed depolarization
- C. Accelerated repolarization
- D. Decreased resting membrane potential
- E. Accelerated depolarization
ST segment evaluation Explanation: ***Delayed repolarization***
- **Voltage-gated potassium channels** are primarily responsible for the efflux of potassium ions during the **repolarization phase** (phase 3) of the cardiac action potential.
- A decrease in the number of these channels would reduce potassium efflux, thus slowing down the repolarization process and prolonging the **action potential duration**.
*Delayed depolarization*
- **Depolarization** (phase 0) of the cardiac action potential is primarily mediated by the rapid influx of **sodium ions** through voltage-gated sodium channels.
- Changes in potassium channels do not directly affect the speed of depolarization.
*Accelerated repolarization*
- Accelerated repolarization would occur if there were an *increase* in the number or activity of **potassium channels**, leading to a faster efflux of potassium ions.
- A *decrease* in these channels would have the opposite effect.
*Decreased resting membrane potential*
- The **resting membrane potential** is primarily maintained by the **leak potassium channels** and the **Na+/K+ ATPase pump**, not directly by voltage-gated potassium channels involved in repolarization.
- A decrease in voltage-gated potassium channels would not significantly alter the resting membrane potential.
*Accelerated depolarization*
- Accelerated depolarization would result from an *increase* in the speed or magnitude of **sodium influx** during phase 0.
- A reduction in potassium channels has no direct impact on the rate of sodium channel activation or current.
More ST segment evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.