QT interval and QTc calculation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for QT interval and QTc calculation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
QT interval and QTc calculation US Medical PG Question 1: A 21-year-old woman presents with palpitations and anxiety. She had a recent outpatient ECG that was suggestive of supraventricular tachycardia, but her previous physician failed to find any underlying disease. No other significant past medical history. Her vital signs include blood pressure 102/65 mm Hg, pulse 120/min, respiratory rate 17/min, and temperature 36.5℃ (97.7℉). Electrophysiological studies reveal an atrioventricular nodal reentrant tachycardia. The patient refuses an ablation procedure so it is decided to perform synchronized cardioversion with consequent ongoing management with verapamil. Which of the following ECG features should be monitored in this patient during treatment?
- A. Amplitude and direction of the T wave
- B. Length of QRS complex
- C. Length of QT interval
- D. Length of PR interval (Correct Answer)
- E. QRS complex amplitude
QT interval and QTc calculation Explanation: ***Length of PR interval***
- Verapamil is a **non-dihydropyridine calcium channel blocker** that primarily acts on the **AV node** to slow conduction.
- Monitoring the **PR interval** is crucial because excessive slowing of AV nodal conduction can lead to **AV block**, which is indicated by a prolonged PR interval.
*Amplitude and direction of the T wave*
- Changes in T-wave amplitude and direction are often associated with **myocardial ischemia** or **electrolyte imbalances**, which are not the primary concerns with verapamil.
- While verapamil can affect repolarization, the most direct and common adverse effect related to its mechanism of action on the AV node is not primarily reflected in T-wave changes.
*Length of QRS complex*
- The QRS complex duration primarily reflects **ventricular depolarization** and is typically affected by medications that alter conduction through the His-Purkinje system or within the ventricles, such as antiarrhythmics like **flecainide** or **amiodarone**.
- Verapamil's main action is on the AV node, so it generally does not significantly prolong the QRS complex unless there is pre-existing conduction system disease.
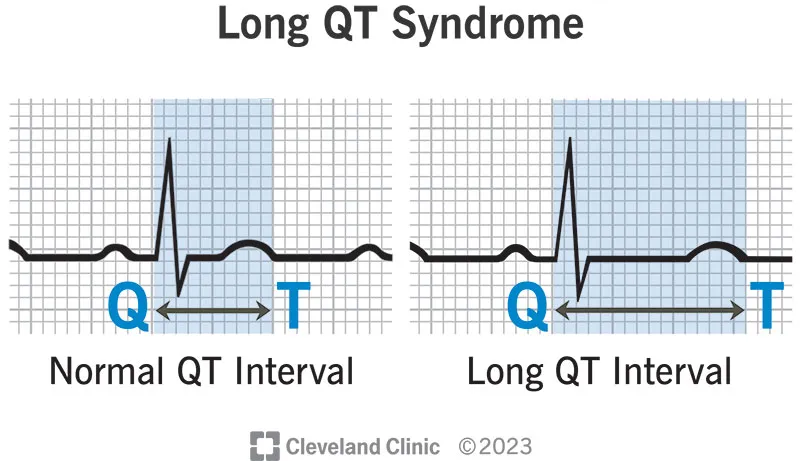
*Length of QT interval*
- The QT interval represents **ventricular repolarization**, and its prolongation can lead to **Torsades de Pointes**, a life-threatening arrhythmia.
- While many antiarrhythmics can prolong the QT interval, **verapamil is not known to significantly prolong the QT interval** and is generally considered safe in this regard.
*QRS complex amplitude*
- Changes in QRS amplitude can indicate conditions like **pericardial effusion**, **cardiomyopathy**, or changes in ventricular mass.
- These are generally not direct or common side effects of verapamil therapy, which primarily focuses on AV nodal conduction.
QT interval and QTc calculation US Medical PG Question 2: A 62-year-old man is brought to the emergency department because of syncope. He reports sudden onset of palpitations followed by loss of consciousness while carrying his groceries to his car. He is unable to recall any further details and does not have any chest pain or dizziness. He has a history of hypertension, type 2 diabetes mellitus, gastroparesis, and osteoarthritis of the knees. Medications include lisinopril, metformin, and ondansetron as needed for nausea. He also takes methadone daily for chronic pain. Apart from an abrasion on his forehead, he appears well. His temperature is 37.2 °C (98.9 F), heart rate is 104/min and regular, and blood pressure is 135/70 mm Hg. While he is in the emergency department, he loses consciousness again. Telemetry shows polymorphic ventricular tachycardia with cyclic alteration of the QRS axis that spontaneously resolves after 30 seconds. Results of a complete blood count, serum electrolyte concentrations, and serum thyroid studies show no abnormalities. Cardiac enzymes are within normal limits. Which of the following is the most likely underlying cause of this patient's syncope?
- A. Prinzmetal angina
- B. Fast accessory conduction pathway
- C. Brugada syndrome
- D. Prolonged QT interval (Correct Answer)
- E. Hypomagnesemia
QT interval and QTc calculation Explanation: ***Prolonged QT interval***
- The patient experienced **polymorphic ventricular tachycardia** with cyclic alteration of the **QRS axis** (Torsades de Pointes), which is characteristic of a prolonged QT interval.
- **Methadone is known to prolong the QT interval**, and the patient's history of syncope preceded by palpitations is consistent with this arrhythmia.
*Prinzmetal angina*
- Prinzmetal angina involves **coronary artery spasm**, leading to **transient myocardial ischemia**, typically causing chest pain, not primarily syncope from polymorphic VT.
- While it can cause arrhythmias, the characteristic EKG finding would be **ST-segment elevation during pain**, which is not described.
*Fast accessory conduction pathway*
- A fast accessory pathway (e.g., in Wolfe-Parkinson-White syndrome) can lead to **AV reentrant tachycardia** or **pre-excitation** with atrial fibrillation, but not typically polymorphic VT with cyclic QRS alteration.
- The EKG would show a **delta wave** and a short PR interval, which is not mentioned.
*Brugada syndrome*
- Brugada syndrome is an inherited channelopathy **characterized by specific EKG patterns** (e.g., coved-type ST elevation in V1-V3) and an increased risk of sudden cardiac death due to ventricular arrhythmias.
- The patient's EKG findings of polymorphic VT with cyclic QRS alteration are not typical of Brugada syndrome-induced arrhythmia.
*Hypomagnesemia*
- While **hypomagnesemia can prolong the QT interval** and lead to Torsades de Pointes, the patient's **serum electrolyte concentrations were normal**, ruling out this direct cause.
- Magnesium levels would need to be critically low for such an effect, and this is typically detected on blood tests.
QT interval and QTc calculation US Medical PG Question 3: A 51-year-old woman with a history of paroxysmal atrial fibrillation comes to the physician for a follow-up visit. She feels well and wants to discuss pausing her only current medication, flecainide. Her pulse is 75/min and regular, blood pressure is 125/75 mm Hg. Physical examination shows no abnormalities. An ECG shows a PR interval of 180 ms, QRS time of 120 ms, and corrected QT interval of 440 ms. Which of the following ECG changes is most likely to be seen on cardiac stress testing in this patient?
- A. Decreased maximal heart rate
- B. Prolonged QRS complex (Correct Answer)
- C. Shortened PR interval
- D. False-positive ST-segment depression
- E. Prolonged QTc interval
QT interval and QTc calculation Explanation: ***Prolonged QRS complex***
- **Flecainide** is a class Ic antiarrhythmic that **blocks fast sodium channels** in myocardial cells, slowing conduction in the atria, ventricles, and His-Purkinje system.
- Its effects are **use-dependent**, meaning the drug binds more effectively to channels that are frequently activated (i.e., at higher heart rates), leading to a **further widening of the QRS complex** during exercise.
*Decreased maximal heart rate*
- While some class II antiarrhythmics (beta-blockers) can decrease maximal heart rate, **flecainide** primarily affects cardiac conduction and does not significantly impact heart rate response to stress.
- The ECG does not suggest sinus node dysfunction that would limit heart rate increase with activity.
*Shortened PR interval*
- Flecainide typically **prolongs the PR interval** by slowing conduction through the atrioventricular (AV) node.
- Exercise would likely exacerbate this effect rather than shorten the PR interval.
*False-positive ST-segment depression*
- While wide QRS complexes (as may occur with flecainide-induced conduction slowing) can cause abnormal ST-segment morphology, the **most prominent and characteristic effect** of flecainide during stress testing is **progressive QRS widening** due to use-dependent sodium channel blockade.
- False-positive ST changes are a nonspecific finding and not the hallmark ECG change expected with flecainide during exercise.
*Prolonged QTc interval*
- Flecainide is generally known to **not significantly prolong the QT interval**; in some cases, it may even shorten it due to its effect on action potential duration.
- Other antiarrhythmics like Class III agents (e.g., amiodarone, sotalol) are more commonly associated with QTc prolongation.
QT interval and QTc calculation US Medical PG Question 4: A 51-year-old woman schedules an appointment with her physician with complaints of upper abdominal pain, nausea, and early satiety for the last 6 months. She has type 1 diabetes for the past 10 years and is on subcutaneous insulin therapy. She complains of occasional heartburn and lost 4.5 kg (10 lb) in the past 6 months without any changes in her diet. The medical history is significant for long QT syndrome. The vital signs include: pulse 74/min, respirations 18/min, temperature 37.7°C (99.9°F), and blood pressure 140/84 mm Hg. Abdominal examination is negative for organomegaly or a palpable mass, but there is a presence of succussion splash. She has slightly decreased vision in both her eyes and fundoscopy reveals diabetic changes in the retina. Esophagogastroduodenoscopy is performed, which is negative for obstruction, but a small ulcer is noted near the cardiac end of the stomach with some food particles. Which of the following drugs would be inappropriate in the management of this patient's condition?
- A. Bethanechol
- B. Domperidone
- C. Erythromycin
- D. Promethazine
- E. Cisapride (Correct Answer)
QT interval and QTc calculation Explanation: ***Cisapride***
- Cisapride is a **prokinetic agent** that was largely withdrawn due to its propensity to cause **QT prolongation** and life-threatening arrhythmias, which is critically contraindicated in patients with a history of **long QT syndrome**.
- The patient's history of **long QT syndrome** makes cisapride an inappropriate and dangerous choice for managing her diabetic gastroparesis.
*Bethanechol*
- Bethanechol is a **muscarinic agonist** that can increase gastric motility, but it is not typically first-line for gastroparesis due to potential systemic cholinergic side effects.
- While it aids in stomach emptying, its use must be weighed against its side-effect profile, though it doesn't directly interact with QT interval.
*Domperidone*
- Domperidone is a **dopamine D2 receptor antagonist** that acts as a prokinetic and antiemetic, primarily in the periphery, minimizing central nervous system side effects.
- While generally safer regarding QT prolongation than some other prokinetics, it can still prolong the QT interval in high doses or in susceptible individuals, but less severely than cisapride.
*Erythromycin*
- Erythromycin is a **macrolide antibiotic** that acts as a **motilin receptor agonist**, significantly increasing gastric emptying.
- It's a useful prokinetic for gastroparesis, although long-term use can be limited by antibiotic resistance and potential for **QT prolongation**, though less severe than cisapride.
*Promethazine*
- Promethazine is an **antihistamine** with antiemetic properties, often used for nausea and vomiting, but it is **not a prokinetic agent**.
- It would address the nausea symptomatically but would not improve gastric emptying in a patient with gastroparesis.
QT interval and QTc calculation US Medical PG Question 5: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
QT interval and QTc calculation Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
QT interval and QTc calculation US Medical PG Question 6: A 52-year-old man comes to the physician because of a 3-day history of intermittent chest tightness that worsens with exercise. He has chronic atrial fibrillation treated with a drug that prolongs the QT interval. During cardiac stress testing, an ECG shows progressive shortening of the QT interval as the heart rate increases. Which of the following drugs is this patient most likely taking?
- A. Lidocaine
- B. Flecainide
- C. Carvedilol
- D. Dofetilide (Correct Answer)
- E. Diltiazem
QT interval and QTc calculation Explanation: ***Dofetilide***
- **Dofetilide** is a **Class III antiarrhythmic** that blocks potassium channels (IKr) and **prolongs the QT interval**, making it the drug described in the stem.
- It is **FDA-approved for conversion and maintenance of sinus rhythm in atrial fibrillation**, matching this patient's treatment history.
- The QT shortening observed during stress testing is **normal physiologic behavior** seen with all drugs—the QT interval naturally decreases as heart rate increases (the corrected QT, or QTc, accounts for this).
- Dofetilide carries a significant **risk of torsades de pointes**, especially with QT prolongation, which is why the stem emphasizes QT monitoring.
*Lidocaine*
- **Lidocaine** is a **Class IB antiarrhythmic** that primarily shortens or has minimal effect on the QT interval.
- It is used for **ventricular arrhythmias** (especially in acute MI), **not for atrial fibrillation**.
- Does not match the described QT-prolonging treatment.
*Flecainide*
- **Flecainide** is a **Class IC antiarrhythmic** that primarily slows conduction by blocking sodium channels.
- It **does not significantly prolong the QT interval**—it may widen the QRS complex but doesn't affect ventricular repolarization substantially.
- While it can be used for atrial fibrillation, it doesn't match the QT-prolonging drug described.
*Carvedilol*
- **Carvedilol** is a **non-selective beta-blocker** with alpha-1 blocking properties used for rate control in atrial fibrillation and heart failure.
- Beta-blockers **do not prolong the QT interval**; they may slightly shorten it or have no effect.
- Does not match the stem description.
*Diltiazem*
- **Diltiazem** is a **non-dihydropyridine calcium channel blocker** used for rate control in atrial fibrillation.
- It **does not prolong the QT interval**—calcium channel blockers affect AV nodal conduction but not ventricular repolarization.
- Does not match the drug described in the stem.
QT interval and QTc calculation US Medical PG Question 7: A 68-year-old man comes to the physician because of fatigue and muscle cramps for the past 4 weeks. He has also noticed several episodes of tingling in both hands. He has not had fever or nausea. He has had a chronic cough for 10 years. He has chronic bronchitis, hypertension, and osteoarthritis of both knees. His father died from lung cancer. Current medications include salbutamol, ibuprofen, and ramipril. He has smoked 1 pack of cigarettes daily for 45 years. He is 175 cm (5 ft 9 in) tall and weighs 68 kg (163 lb); BMI is 22 kg/m2. His temperature is 36.7°C (98°F), pulse is 60/min, and blood pressure is 115/76 mm Hg. While measuring the patient's blood pressure, the physician observes carpopedal spasm. Cardiopulmonary examination shows no abnormalities. His hematocrit is 41%, leukocyte count is 5,800/mm3, and platelet count is 195,000/mm3. Serum alkaline phosphatase activity is 55 U/L. An ECG shows sinus rhythm with a prolonged QT interval. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Multiple endocrine neoplasia
- B. Ectopic hormone production
- C. Medication side effect
- D. Destruction of parathyroid glands
- E. Vitamin D deficiency (Correct Answer)
QT interval and QTc calculation Explanation: ***Vitamin D deficiency***
- The patient's symptoms of **fatigue**, **muscle cramps**, **paresthesias** (tingling in hands), and **carpopedal spasm** (Trousseau's sign) are classic manifestations of **hypocalcemia**.
- The **prolonged QT interval** on ECG further confirms hypocalcemia.
- **Vitamin D deficiency** is the most common cause of hypocalcemia in elderly patients, especially those with:
- **Chronic disease** (chronic bronchitis)
- **Limited sun exposure** (likely given chronic illness)
- **Poor nutrition** or malabsorption
- **Normal alkaline phosphatase** (55 U/L) helps rule out severe bone disease
- This is the most likely diagnosis given the clinical presentation and demographic factors.
*Multiple endocrine neoplasia*
- **MEN syndromes** (MEN1, MEN2a) typically cause **primary hyperparathyroidism** with **hypercalcemia**, not hypocalcemia.
- There is no evidence of other endocrine tumors or family history to suggest MEN.
*Ectopic hormone production*
- **Ectopic PTHrP production** (e.g., from squamous cell lung carcinoma) causes **hypercalcemia**, not hypocalcemia.
- While the patient has smoking history and chronic cough, his presentation is clearly hypocalcemia.
*Medication side effect*
- The patient's current medications (**salbutamol**, **ibuprofen**, **ramipril**) are not commonly associated with symptomatic hypocalcemia.
- None of these medications typically cause carpopedal spasm or prolonged QT interval from calcium disturbances.
*Destruction of parathyroid glands*
- **Hypoparathyroidism** from parathyroid destruction (surgical, autoimmune, or infiltrative) would cause hypocalcemia.
- However, there is **no history** of neck surgery, radiation, or autoimmune disease.
- Without such history, this is less likely than vitamin D deficiency in an elderly patient with chronic disease.
QT interval and QTc calculation US Medical PG Question 8: A 17-year-old girl suddenly grabs her chest and collapses to the ground while playing volleyball at school. The teacher rushes to evaluate the situation and finds that the girl has no pulse and is not breathing. He starts chest compressions. An automated external defibrillator (AED) is brought to the scene within 3 minutes and a shock is delivered. The girl regains consciousness and regular sinus rhythm. She is rushed to the emergency department. The vital signs include: blood pressure 122/77 mm Hg and pulse 65/min. The pulse is regular. An electrocardiogram (ECG) shows a shortened PR interval, a wide QRS complex, a delta wave, and an inverted T wave. Which of the following is the most likely pathology in the conduction system of this patient’s heart?
- A. Impulse generation by tissue in atrioventricular node
- B. Accessory pathway from atria to ventricles (Correct Answer)
- C. Automatic discharge of irregular impulses in the atria
- D. Wandering atrial pacemaker
- E. Blockage in conduction pathway
QT interval and QTc calculation Explanation: ***Accessory pathway from atria to ventricles***
- The ECG findings of a **shortened PR interval**, **delta wave**, and **wide QRS complex** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, which involves an **accessory pathway** (Bundle of Kent) bypassing the AV node.
- This accessory pathway allows for pre-excitation of the ventricles, predisposing patients to **tachyarrhythmias** like the one experienced by the patient (sudden cardiac arrest).
*Impulse generation by tissue in atrioventricular node*
- This describes a **junctional rhythm**, which would present with a **normal or long PR interval** and a **narrow QRS complex**, contrasting with the given ECG findings.
- A junctional rhythm typically results in a slower heart rate and is not generally associated with sudden cardiac arrest in healthy individuals.
*Automatic discharge of irregular impulses in the atria*
- This typically refers to **atrial fibrillation** or multifocal atrial tachycardia, which would show an **irregularly irregular rhythm** or multiple P-wave morphologies, not the specific PR and QRS abnormalities seen.
- While atrial fibrillation can occur with WPW, the primary pathology described by the ECG findings is the accessory pathway itself.
*Wandering atrial pacemaker*
- A **wandering atrial pacemaker** is characterized by varying P-wave morphology and PR intervals as the pacemaker shifts between different atrial sites, but it generally maintains a normal QRS duration.
- It is typically a benign arrhythmia and does not cause the pre-excitation or the risk of sudden cardiac death seen in this patient.
*Blockage in conduction pathway*
- A **blockage in the conduction pathway** (e.g., AV block) would result in a **prolonged PR interval** or dropped QRS complexes, which is the opposite of the shortened PR interval observed.
- While heart block can cause syncope, it wouldn't explain the pre-excitation pattern (delta wave, wide QRS) seen in the ECG.
QT interval and QTc calculation US Medical PG Question 9: An investigator develops a new drug that decreases the number of voltage-gated potassium channels in cardiac muscle cell membranes. Which of the following is the most likely effect of this drug on the myocardial action potential?
- A. Delayed repolarization (Correct Answer)
- B. Delayed depolarization
- C. Accelerated repolarization
- D. Decreased resting membrane potential
- E. Accelerated depolarization
QT interval and QTc calculation Explanation: ***Delayed repolarization***
- **Voltage-gated potassium channels** are primarily responsible for the efflux of potassium ions during the **repolarization phase** (phase 3) of the cardiac action potential.
- A decrease in the number of these channels would reduce potassium efflux, thus slowing down the repolarization process and prolonging the **action potential duration**.
*Delayed depolarization*
- **Depolarization** (phase 0) of the cardiac action potential is primarily mediated by the rapid influx of **sodium ions** through voltage-gated sodium channels.
- Changes in potassium channels do not directly affect the speed of depolarization.
*Accelerated repolarization*
- Accelerated repolarization would occur if there were an *increase* in the number or activity of **potassium channels**, leading to a faster efflux of potassium ions.
- A *decrease* in these channels would have the opposite effect.
*Decreased resting membrane potential*
- The **resting membrane potential** is primarily maintained by the **leak potassium channels** and the **Na+/K+ ATPase pump**, not directly by voltage-gated potassium channels involved in repolarization.
- A decrease in voltage-gated potassium channels would not significantly alter the resting membrane potential.
*Accelerated depolarization*
- Accelerated depolarization would result from an *increase* in the speed or magnitude of **sodium influx** during phase 0.
- A reduction in potassium channels has no direct impact on the rate of sodium channel activation or current.
More QT interval and QTc calculation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.