QRS complex analysis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for QRS complex analysis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
QRS complex analysis US Medical PG Question 1: A previously healthy 19-year-old man is brought to the emergency department by his girlfriend after briefly losing consciousness. He passed out while moving furniture into her apartment. She said that he was unresponsive for a minute but regained consciousness and was not confused. The patient did not have any chest pain, palpitations, or difficulty breathing before or after the episode. He has had episodes of dizziness when exercising at the gym. His blood pressure is 125/75 mm Hg while supine and 120/70 mm Hg while standing. Pulse is 70/min while supine and 75/min while standing. On examination, there is a grade 3/6 systolic murmur at the left lower sternal border and a systolic murmur at the apex, both of which disappear with passive leg elevation. Which of the following is the most likely cause?
- A. Prolonged QT interval
- B. Hypertrophic cardiomyopathy (Correct Answer)
- C. Mitral valve stenosis
- D. Mitral valve prolapse
- E. Bicuspid aortic valve
QRS complex analysis Explanation: ***Hypertrophic cardiomyopathy***
- This patient's **syncope associated with exertion** (moving furniture) and episodes of **dizziness during exercise** are highly suggestive of hypertrophic cardiomyopathy (HCM).
- The presence of a **systolic murmur at the left sternal border and apex** that **decreases/disappears with passive leg elevation** indicates a dynamic left ventricular outflow tract (LVOT) obstruction that is sensitive to preload changes, a hallmark of HCM.
- Passive leg elevation **increases preload** → **increases LV volume** → **decreases LVOT obstruction** → **decreases murmur intensity**.
*Prolonged QT interval*
- While it can cause syncope, especially exertional, a prolonged QT interval generally **does not present with dynamic murmurs** that change with preload.
- ECG findings (not mentioned here) would be the primary diagnostic clue, not physical exam findings related to murmurs.
*Mitral valve stenosis*
- Mitral stenosis would typically present with a **diastolic murmur** (not systolic) and symptoms like dyspnea, fatigue, and possibly hemoptysis due to elevated left atrial pressure.
- The murmur of mitral stenosis would not characteristically change with passive leg elevation in the manner described.
*Mitral valve prolapse*
- Mitral valve prolapse often presents with a **mid-systolic click** followed by a systolic murmur, which typically **intensifies with standing** or maneuvers that decrease left ventricular volume.
- The murmur described here decreases with leg elevation (increased preload), which is the opposite behavior of a mitral prolapse murmur.
*Bicuspid aortic valve*
- A bicuspid aortic valve can cause an **aortic stenosis murmur** (a systolic ejection murmur heard best at the right upper sternal border) or regurgitation, but it generally **does not cause a dynamic murmur that changes with preload** in this characteristic fashion.
- Symptoms related to bicuspid aortic valve disease (like syncope) would more commonly be associated with significant stenosis, not with a murmur that is acutely sensitive to preload changes.
QRS complex analysis US Medical PG Question 2: A researcher measures action potential propagation velocity in various regions of the heart in a 42-year-old Caucasian female. Which of the following set of measurements corresponds to the velocities found in the atrial muscle, AV Node, Purkinje system, and ventricular muscle, respectively?
- A. 0.05 m/s, 1.1 m/s, 2.2 m/s, 3.3 m/s
- B. 2.2 m/s, 0.3 m/s, 0.05 m/s, 1.1 m/s
- C. 0.3 m/s, 2.2 m/s, 0.05 m/s, 1.1 m/s
- D. 0.5 m/s, 1.1 m/s, 2.2 m/s, 3 m/s
- E. 1.1 m/s, 0.05 m/s, 2.2 m/s, 0.3 m/s (Correct Answer)
QRS complex analysis Explanation: ***1.1 m/s, 0.05 m/s, 2.2 m/s, 0.3 m/s***
- This option correctly lists the approximate conduction velocities for the **atrial muscle (1.1 m/s)**, **AV node (0.05 m/s)**, **Purkinje system (2.2 m/s)**, and **ventricular muscle (0.3 m/s)**, respectively.
- The **AV node has the slowest conduction velocity (~0.05 m/s)**, which is crucial for delaying ventricular contraction and allowing complete ventricular filling.
- The **Purkinje system has the fastest conduction velocity (~2-4 m/s)**, ensuring rapid and coordinated ventricular depolarization.
- **Atrial muscle (~1 m/s)** and **ventricular muscle (~0.3-0.5 m/s)** have intermediate velocities.
*0.05 m/s, 1.1 m/s, 2.2 m/s, 3.3 m/s*
- This sequence is incorrect because it places the **AV node's velocity (0.05 m/s)** first (as atrial muscle) and significantly overestimates ventricular muscle velocity (3.3 m/s).
- Atrial muscle conducts faster than 0.05 m/s, and ventricular muscle velocity should be approximately 0.3-0.5 m/s, not 3.3 m/s.
*2.2 m/s, 0.3 m/s, 0.05 m/s, 1.1 m/s*
- This option incorrectly assigns the **highest velocity (2.2 m/s)** to atrial muscle, which is characteristic of the Purkinje system, and misplaces the **slowest velocity (0.05 m/s)** in the Purkinje system instead of the AV node.
- The values do not align with known physiological conduction speeds across cardiac tissues.
*0.3 m/s, 2.2 m/s, 0.05 m/s, 1.1 m/s*
- This sequence incorrectly places the **slowest velocity (0.05 m/s)** in the Purkinje system, which is known for the most rapid conduction, and assigns an unrealistically high velocity (2.2 m/s) to the AV node.
- The arrangement directly contradicts the physiological function and relative speeds within the cardiac conduction system.
*0.5 m/s, 1.1 m/s, 2.2 m/s, 3 m/s*
- This option underestimates the **atrial muscle velocity** (0.5 m/s instead of ~1 m/s) and significantly overestimates the **ventricular muscle velocity** (3 m/s instead of ~0.3-0.5 m/s).
- The provided values do not accurately represent the typical ranges of conduction velocities for each specified cardiac region.
QRS complex analysis US Medical PG Question 3: A 23-year-old man comes to the emergency department because of palpitations, dizziness, and substernal chest pain for three hours. The day prior, he was at a friend’s wedding, where he consumed seven glasses of wine. The patient appears diaphoretic. His pulse is 220/min and blood pressure is 120/84 mm Hg. Based on the patient's findings on electrocardiography, the physician diagnoses atrial fibrillation with rapid ventricular response and administers verapamil for rate control. Ten minutes later, the patient is unresponsive and loses consciousness. Despite resuscitative efforts, the patient dies. Histopathologic examination of the heart at autopsy shows an accessory atrioventricular conduction pathway. Electrocardiography prior to the onset of this patient's symptoms would most likely have shown which of the following findings?
- A. Epsilon wave following the QRS complex
- B. Prolongation of the QT interval
- C. Cyclic alteration of the QRS axis
- D. Slurred upstroke of the QRS complex (Correct Answer)
- E. Positive Sokolow-Lyon index
QRS complex analysis Explanation: ***Slurred upstroke of the QRS complex***
- The patient's presentation with **atrial fibrillation with rapid ventricular response** and subsequent collapse after verapamil administration—a calcium channel blocker—is classic for a pre-excitation syndrome like **Wolff-Parkinson-White (WPW) syndrome**.
- In WPW, an accessory pathway (bundle of Kent) bypasses the AV node, leading to a **short PR interval** and a **delta wave** (slurred upstroke of the QRS complex) on ECG during normal sinus rhythm.
*Epsilon wave following the QRS complex*
- An **epsilon wave** is characteristic of **arrhythmogenic right ventricular cardiomyopathy (ARVC)**, representing delayed depolarization of the right ventricle.
- While ARVC can cause arrhythmias, it is distinctly different from the pre-excitation syndrome described, which involves an accessory pathway.
*Prolongation of the QT interval*
- **Prolonged QT interval** is associated with an increased risk of **torsades de pointes**, a polymorphic ventricular tachycardia.
- This finding is typical of **long QT syndrome** and does not directly relate to an accessory atrioventricular conduction pathway.
*Cyclic alteration of the QRS axis*
- **Cyclic alteration of the QRS axis** or electrical alternans is seen in conditions causing swings in cardiac position, most notably **pericardial effusion with tamponade**.
- This ECG finding is unrelated to accessory pathways or the mechanisms of pre-excitation syndromes.
*Positive Sokolow-Lyon index*
- A **positive Sokolow-Lyon index** signifies **left ventricular hypertrophy (LVH)**, characterized by large QRS voltages (e.g., SV1 + RV5/V6 ≥ 35 mm).
- While LVH can be associated with various cardiac conditions, it is not a direct ECG manifestation of an accessory atrioventricular conduction pathway.
QRS complex analysis US Medical PG Question 4: A 48-year-old female comes into the ER with chest pain. An electrocardiogram (EKG) shows a heart beat of this individual in Image A. The QRS complex best correlates with what part of the action potential of the ventricular myocyte shown in Image B?
- A. Phase 1, which is primarily characterized by potassium and chloride efflux
- B. Phase 0, which is primarily characterized by potassium efflux
- C. Phase 3, which is primarily characterized by potassium efflux
- D. Phase 1, which is primarily characterized by calcium efflux
- E. Phase 0, which is primarily characterized by sodium influx (Correct Answer)
QRS complex analysis Explanation: ***Phase 0, which is primarily characterized by sodium influx***
- The **QRS complex** on an EKG represents ventricular depolarization, which is the electrical event linked to **Phase 0** of the ventricular myocyte action potential.
- **Phase 0** is characterized by the rapid influx of **sodium ions** through fast voltage-gated sodium channels, leading to a quick rise in membrane potential.
*Phase 1, which is primarily characterized by potassium and chloride efflux*
- **Phase 1** represents initial repolarization, which immediately follows depolarization and is a very brief phase, not the primary event represented by the extensive QRS complex.
- This phase is characterized by the inactivation of sodium channels and the efflux of **potassium** and **chloride ions**, leading to a slight drop in membrane potential.
*Phase 0, which is primarily characterized by potassium efflux*
- **Phase 0** is indeed ventricular depolarization, but it is primarily characterized by **sodium influx**, not potassium efflux.
- **Potassium efflux** is primarily associated with repolarization phases (Phase 1, 2, and 3), not the initial depolarization (Phase 0).
*Phase 3, which is primarily characterized by potassium efflux*
- **Phase 3** represents the rapid repolarization of the ventricular myocyte, which corresponds to the **T wave** on the EKG, not the QRS complex.
- This phase is primarily driven by the efflux of **potassium ions** through various potassium channels, bringing the membrane potential back to its resting state.
*Phase 1, which is primarily characterized by calcium efflux*
- **Phase 1** is the initial repolarization, but it is characterized by **potassium and chloride efflux**, not calcium efflux.
- **Calcium influx** is characteristic of Phase 2 (the plateau phase), which occurs after the QRS complex and contributes to the ST segment.
QRS complex analysis US Medical PG Question 5: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
QRS complex analysis Explanation: ***Normal duration defined as less than 120 milliseconds***
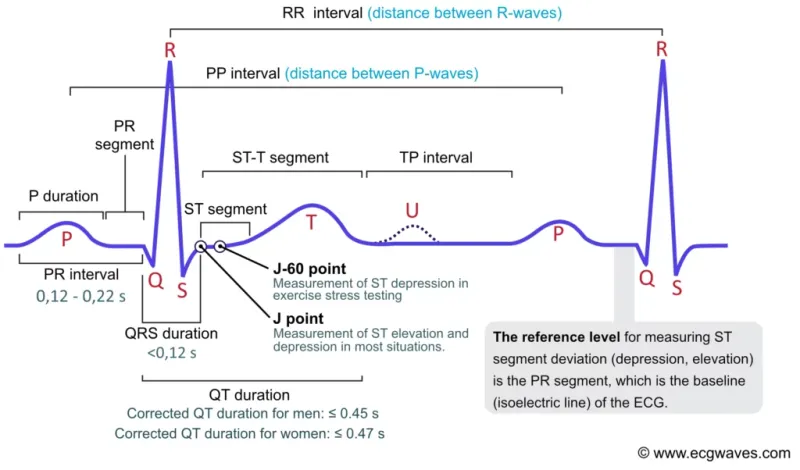
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
QRS complex analysis US Medical PG Question 6: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
QRS complex analysis Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
QRS complex analysis US Medical PG Question 7: A 41-year-old woman presents to the emergency room with chest pain. She has had progressive substernal chest pain accompanied by weakness and mild shortness of breath for the past 2 hours. Her past medical history is notable for poorly controlled systemic lupus erythematosus (SLE), Sjogren syndrome, and interstitial lung disease. She was hospitalized last year with pericarditis presumed to be from SLE. Her temperature is 98.6°F (37°C), blood pressure is 106/56 mmHg, pulse is 132/min, and respirations are 26/min. On exam, the skin overlying the internal jugular vein fills at 9 cm above the sternal angle and distant heart sounds are appreciated. There is no friction rub. She is given 1000cc of intravenous fluids with no appreciable change in her blood pressure. An electrocardiogram in this patient would most likely reveal which of the following findings?
- A. Polymorphic P waves
- B. ST elevations in leads II, III, and aVF
- C. Peaked T waves
- D. Wide QRS complexes with no P waves
- E. Electrical alternans (Correct Answer)
QRS complex analysis Explanation: ***Electrical alternans***
- The patient's symptoms (chest pain, shortness of breath, **hypotension**, **tachycardia**, **elevated JVP**, and **distant heart sounds**) in the context of a history of **pericarditis** and **SLE** are highly suggestive of **cardiac tamponade.**
- **Electrical alternans**, characterized by alternating QRS complex heights due to the swinging motion of the heart in a large pericardial effusion, is a classic EKG finding for cardiac tamponade.
- This finding reflects the mechanical swinging of the heart within the pericardial fluid, causing beat-to-beat variation in QRS amplitude.
*Polymorphic P waves*
- **Polymorphic P waves** (multifocal atrial tachycardia) occur when there are at least three different P wave morphologies on the EKG, indicating multiple ectopic atrial foci.
- This is typically seen in patients with severe lung disease or other conditions causing increased atrial stretch, but it is not a direct consequence or typical finding of cardiac tamponade.
*ST elevations in leads II, III, and aVF*
- **ST elevations in leads II, III, and aVF** indicate an **inferior myocardial infarction**, which is caused by coronary artery occlusion.
- While chest pain is present, the patient's other signs (elevated JVP, distant heart sounds, hypotension not responding to fluids, history of pericarditis/SLE) point away from an acute MI and strongly towards cardiac tamponade.
*Peaked T waves*
- **Peaked T waves** are characteristic of **hyperkalemia**, a condition of excessively high potassium levels in the blood.
- While hyperkalemia can cause cardiac symptoms, it does not typically present with the specific hemodynamic compromise and physical exam findings (elevated JVP, distant heart sounds) described, which are classic for cardiac tamponade.
*Wide QRS complexes with no P waves*
- **Wide QRS complexes with no P waves** are characteristic of a **ventricular arrhythmia**, such as ventricular tachycardia or idioventricular rhythm.
- While the patient is hypotensive and tachycardic, the presenting symptoms and physical exam findings are not directly indicative of a primary ventricular arrhythmia, but rather suggest an extracardiac compression of the heart due to tamponade.
QRS complex analysis US Medical PG Question 8: A 17-year-old girl suddenly grabs her chest and collapses to the ground while playing volleyball at school. The teacher rushes to evaluate the situation and finds that the girl has no pulse and is not breathing. He starts chest compressions. An automated external defibrillator (AED) is brought to the scene within 3 minutes and a shock is delivered. The girl regains consciousness and regular sinus rhythm. She is rushed to the emergency department. The vital signs include: blood pressure 122/77 mm Hg and pulse 65/min. The pulse is regular. An electrocardiogram (ECG) shows a shortened PR interval, a wide QRS complex, a delta wave, and an inverted T wave. Which of the following is the most likely pathology in the conduction system of this patient’s heart?
- A. Impulse generation by tissue in atrioventricular node
- B. Accessory pathway from atria to ventricles (Correct Answer)
- C. Automatic discharge of irregular impulses in the atria
- D. Wandering atrial pacemaker
- E. Blockage in conduction pathway
QRS complex analysis Explanation: ***Accessory pathway from atria to ventricles***
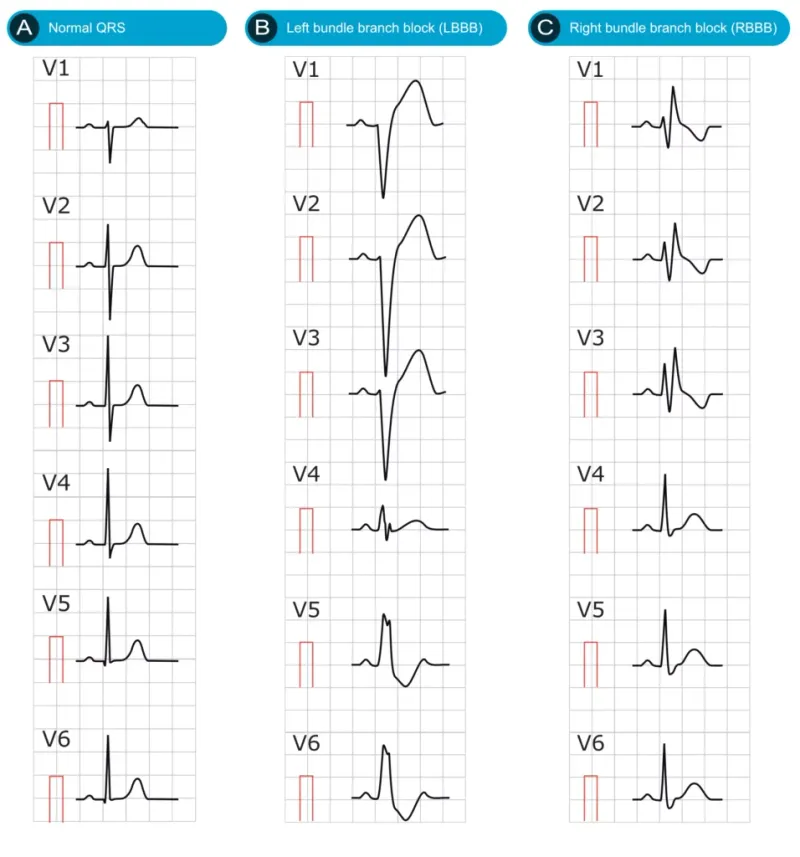
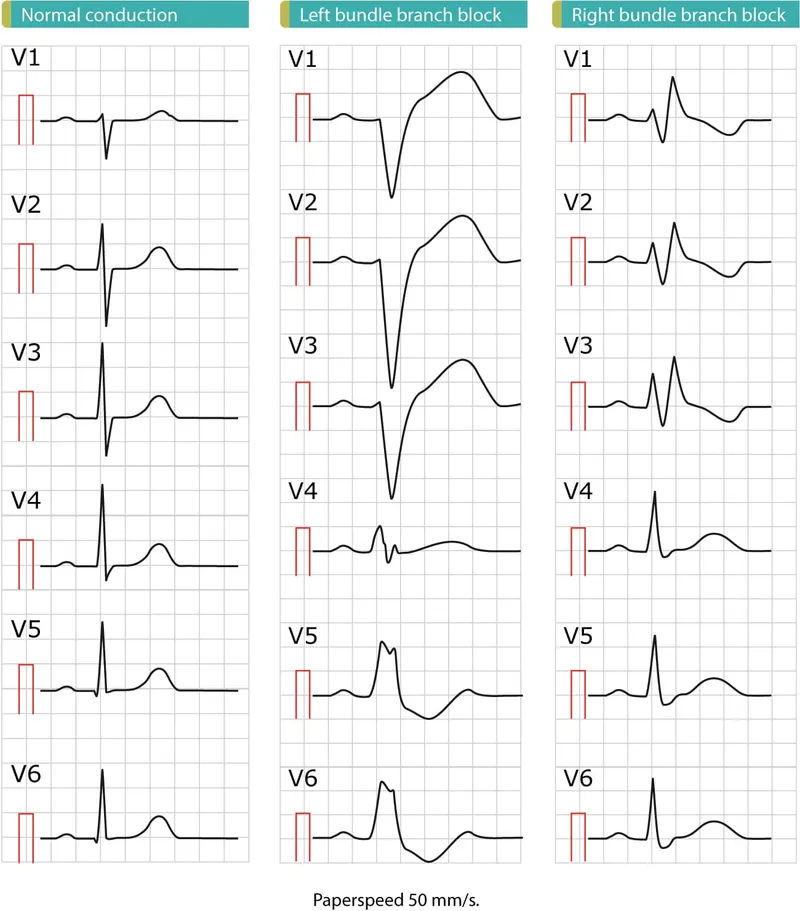
- The ECG findings of a **shortened PR interval**, **delta wave**, and **wide QRS complex** are characteristic of **Wolff-Parkinson-White (WPW) syndrome**, which involves an **accessory pathway** (Bundle of Kent) bypassing the AV node.
- This accessory pathway allows for pre-excitation of the ventricles, predisposing patients to **tachyarrhythmias** like the one experienced by the patient (sudden cardiac arrest).
*Impulse generation by tissue in atrioventricular node*
- This describes a **junctional rhythm**, which would present with a **normal or long PR interval** and a **narrow QRS complex**, contrasting with the given ECG findings.
- A junctional rhythm typically results in a slower heart rate and is not generally associated with sudden cardiac arrest in healthy individuals.
*Automatic discharge of irregular impulses in the atria*
- This typically refers to **atrial fibrillation** or multifocal atrial tachycardia, which would show an **irregularly irregular rhythm** or multiple P-wave morphologies, not the specific PR and QRS abnormalities seen.
- While atrial fibrillation can occur with WPW, the primary pathology described by the ECG findings is the accessory pathway itself.
*Wandering atrial pacemaker*
- A **wandering atrial pacemaker** is characterized by varying P-wave morphology and PR intervals as the pacemaker shifts between different atrial sites, but it generally maintains a normal QRS duration.
- It is typically a benign arrhythmia and does not cause the pre-excitation or the risk of sudden cardiac death seen in this patient.
*Blockage in conduction pathway*
- A **blockage in the conduction pathway** (e.g., AV block) would result in a **prolonged PR interval** or dropped QRS complexes, which is the opposite of the shortened PR interval observed.
- While heart block can cause syncope, it wouldn't explain the pre-excitation pattern (delta wave, wide QRS) seen in the ECG.
QRS complex analysis US Medical PG Question 9: A 44-year-old man comes to the emergency department because of persistent palpitations for the past 2 hours. The day before, he was at a wedding, where he drank several glasses of wine and 9–10 vodka cocktails. He has never had similar symptoms before. He is a manager at a software company and has recently had a lot of work-related stress. He is otherwise healthy and takes no medications. His temperature is 36.5°C (97.7°F), pulse is 90/min and irregularly irregular, respirations are 13/min, and his blood pressure is 128/60 mm Hg. Physical examination shows no other abnormalities. An ECG is performed; no P-waves can be identified. Echocardiography shows no valvular abnormalities and normal ventricular function. One hour later, a repeat ECG shows normal P waves followed by narrow QRS complexes. He is still experiencing occasional palpitations. Which of the following is the most appropriate next step in management?
- A. Electrical cardioversion
- B. Defibrillation
- C. Adenosine injection
- D. Observation (Correct Answer)
- E. Catheter ablation
QRS complex analysis Explanation: ***Observation***
- The patient experienced **paroxysmal atrial fibrillation (AF)** likely triggered by **binge alcohol consumption** (holiday heart syndrome), which has already spontaneously converted to normal sinus rhythm.
- Given his hemodynamic stability, normal ventricular function, and the transient nature of this isolated episode, **close observation** for recurrence is the most appropriate initial step.
*Electrical cardioversion*
- This is primarily used for **hemodynamically unstable AF** or for persistent AF that fails to convert spontaneously.
- The patient is currently **hemodynamically stable** and has already converted to normal sinus rhythm, making cardioversion unnecessary.
*Defibrillation*
- **Defibrillation** is used for life-threatening arrhythmias like **ventricular fibrillation** or **pulseless ventricular tachycardia**.
- It is not indicated for stable atrial fibrillation, and the patient has already converted to sinus rhythm.
*Adenosine injection*
- **Adenosine** is used to terminate **supraventricular tachycardias (SVTs)** by blocking the AV node.
- It is generally **ineffective for atrial fibrillation** and not indicated here as the patient is already in normal sinus rhythm.
*Catheter ablation*
- **Catheter ablation** is a definitive treatment for recurrent symptomatic AF or other arrhythmias that are refractory to medical management.
- This patient has experienced a **first-time episode** that spontaneously resolved, making ablation an overly aggressive and premature intervention.
QRS complex analysis US Medical PG Question 10: An investigator develops a new drug that decreases the number of voltage-gated potassium channels in cardiac muscle cell membranes. Which of the following is the most likely effect of this drug on the myocardial action potential?
- A. Delayed repolarization (Correct Answer)
- B. Delayed depolarization
- C. Accelerated repolarization
- D. Decreased resting membrane potential
- E. Accelerated depolarization
QRS complex analysis Explanation: ***Delayed repolarization***
- **Voltage-gated potassium channels** are primarily responsible for the efflux of potassium ions during the **repolarization phase** (phase 3) of the cardiac action potential.
- A decrease in the number of these channels would reduce potassium efflux, thus slowing down the repolarization process and prolonging the **action potential duration**.
*Delayed depolarization*
- **Depolarization** (phase 0) of the cardiac action potential is primarily mediated by the rapid influx of **sodium ions** through voltage-gated sodium channels.
- Changes in potassium channels do not directly affect the speed of depolarization.
*Accelerated repolarization*
- Accelerated repolarization would occur if there were an *increase* in the number or activity of **potassium channels**, leading to a faster efflux of potassium ions.
- A *decrease* in these channels would have the opposite effect.
*Decreased resting membrane potential*
- The **resting membrane potential** is primarily maintained by the **leak potassium channels** and the **Na+/K+ ATPase pump**, not directly by voltage-gated potassium channels involved in repolarization.
- A decrease in voltage-gated potassium channels would not significantly alter the resting membrane potential.
*Accelerated depolarization*
- Accelerated depolarization would result from an *increase* in the speed or magnitude of **sodium influx** during phase 0.
- A reduction in potassium channels has no direct impact on the rate of sodium channel activation or current.
More QRS complex analysis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.