Electrolyte effects on ECG US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Electrolyte effects on ECG. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Electrolyte effects on ECG US Medical PG Question 1: Four days after admission to the hospital for anorexia nervosa, a 20-year-old woman has new-onset palpitations and paresthesias in all four limbs. Prior to admission, she was found unconscious by her parents on the floor of a residential treatment center. The patient was started on a trial of nutritional rehabilitation upon arrival to the hospital. Her temperature is 36°C (96.8°F), pulse is 47/min, and blood pressure is 90/60 mmHg. She is 160 cm tall and weighs 35 kg; BMI is 14 kg/m2. The patient appears emaciated. Examination shows lower leg edema. A 2/6 holosystolic murmur is heard over the 5th intercostal space at the midclavicular line. An ECG shows intermittent supraventricular tachycardia and QTc prolongation. Serum studies show:
Day 2 Day 4
Potassium (mEq/L) 3.5 2.7
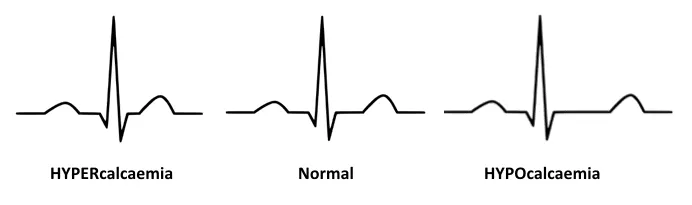
Calcium (mg/dL) 8.5 7.8
Magnesium (mEq/L) 1.2 0.5
Phosphorus (mg/dL) 3.6 1.5
Which of the following is the most likely underlying cause of this patient's condition?
- A. Uncompensated metabolic alkalosis
- B. Thiamine deficiency
- C. Euthyroid sick syndrome
- D. Rapid gastric emptying
- E. Increased insulin release (Correct Answer)
Electrolyte effects on ECG Explanation: ***Increased insulin release***
- **Refeeding syndrome** is triggered by a sudden increase in carbohydrate intake after a period of starvation, leading to an abrupt rise in **insulin secretion**.
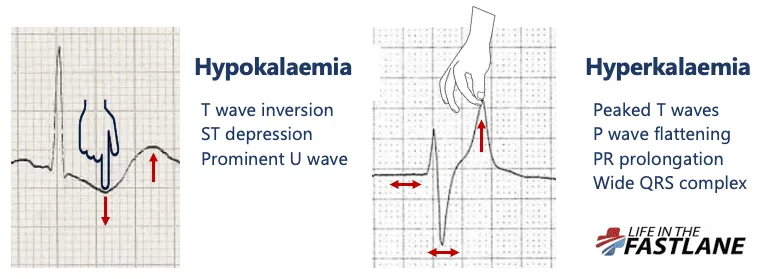
- Insulin shifts **potassium, phosphate, and magnesium** into cells, causing rapid and severe **hypokalemia, hypophosphatemia, and hypomagnesemia**, which manifest as cardiac arrhythmias, neurological symptoms (paresthesias), and muscle weakness.
*Uncompensated metabolic alkalosis*
- While metabolic alkalosis can occur in anorexia nervosa due to **vomiting**, it typically causes hypokalemia, not the widespread electrolyte derangements seen here.
- It does not directly explain the acute drop in **phosphate and magnesium** or the onset of refeeding syndrome symptoms.
*Thiamine deficiency*
- **Thiamine deficiency** can occur in malnourished patients and lead to Wernicke encephalopathy or Korsakoff syndrome, but it typically presents with ocular abnormalities, ataxia, and confusion, not primarily with the acute cardiac and electrolyte disturbances observed.
- While important for metabolism, it is not the **primary driver** of the acute electrolyte shifts characteristic of refeeding syndrome.
*Euthyroid sick syndrome*
- Characterized by **abnormal thyroid function tests** in a severely ill patient without primary thyroid disease, reflecting altered peripheral thyroid hormone metabolism.
- It does not directly cause the acute and severe **electrolyte abnormalities** (hypokalemia, hypophosphatemia, hypomagnesemia) or the specific clinical presentation of refeeding syndrome.
*Rapid gastric emptying*
- While rapid gastric emptying can be a feature in some eating disorders, it directly leads to symptoms like **dumping syndrome** (abdominal pain, diarrhea).
- It does not explain the profound **intracellular shift of electrolytes** and the resulting cardiac and neurological symptoms seen in this case.
Electrolyte effects on ECG US Medical PG Question 2: An ECG from an 8-year-old male with neurosensory deafness and a family history of sudden cardiac arrest demonstrates QT-interval prolongation. Which of the following is this patient most at risk of developing?
- A. Hypertrophic cardiac myopathy
- B. Cardiac tamponade
- C. Essential hypertension
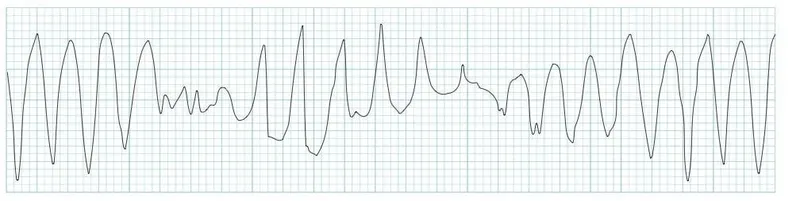
- D. Torsades de pointes (Correct Answer)
- E. First degree atrioventricular block
Electrolyte effects on ECG Explanation: ***Torsades de pointes***
- The combination of **neurosensory deafness**, **QT-interval prolongation**, and a family history of **sudden cardiac arrest** is highly suggestive of **Jervell and Lange-Nielsen syndrome**, a form of **long QT syndrome**.
- Patients with long QT syndrome are at significant risk for developing **polymorphic ventricular tachycardia** known as **Torsades de pointes**, which can degenerate into **ventricular fibrillation** and cause sudden cardiac death.
*Hypertrophic cardiac myopathy*
- This condition involves thickening of the **ventricular walls** and is associated with outflow tract obstruction, not primarily with QT prolongation.
- While it can cause sudden cardiac arrest, it typically presents with symptoms like **dyspnea, chest pain**, or syncope during exertion, and its ECG findings usually include **left ventricular hypertrophy** and **deep Q waves**.
*Cardiac tamponade*
- **Cardiac tamponade** results from the accumulation of fluid in the **pericardial sac**, compressing the heart and impairing its filling.
- This condition is not related to **QT prolongation** or **sensorineural deafness** and would present with signs of **hemodynamic instability**, such as **pulsus paradoxus** and muffled heart sounds.
*Essential hypertension*
- **Essential hypertension** is chronic high blood pressure with no identifiable secondary cause, commonly affecting adults.
- It is not associated with **congenital neurosensory deafness** or significant **QT-interval prolongation** in childhood.
*First degree atrioventricular block*
- **First-degree AV block** is characterized by a prolonged **PR interval** on ECG, indicating delayed conduction through the AV node.
- While it's an electrical abnormality, it is distinct from **QT prolongation** and is not typically associated with **neurosensory deafness** or the same risk of sudden cardiac arrest as long QT syndrome.
Electrolyte effects on ECG US Medical PG Question 3: A 53-year-old man with obesity and heart disease presents to your outpatient clinic with complaints of orthopnea, significant dyspnea on minimal exertion, nausea, vomiting, and diarrhea. He says that his old doctor gave him "some pills" that he takes in varying amounts every morning. Physical exam is significant for a severely displaced point of maximal impulse, bilateral rales in the lower lung fields, an S3 gallop, and hepatomegaly. You decide to perform an EKG (shown in figure A). Suddenly, his rhythm changes to ventricular tachycardia followed by ventricular fibrillation, and he syncopizes and expires despite resuscitative efforts. High levels of which medication are most likely responsible?
- A. Propranolol
- B. Amiodarone
- C. Lidocaine
- D. Verapamil
- E. Digoxin (Correct Answer)
Electrolyte effects on ECG Explanation: ***Digoxin***
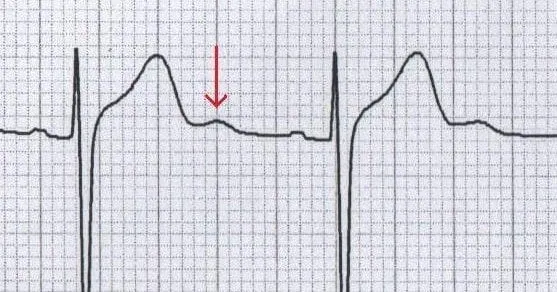
- The patient's presentation with **heart failure** symptoms (dyspnea, orthopnea, rales, S3 gallop, hepatomegaly) and erratic self-dosing of "some pills" strongly suggests **digoxin toxicity**.
- **Gastrointestinal symptoms** (nausea, vomiting, diarrhea) are common initial signs of digoxin toxicity, and the progression to **ventricular tachycardia** and **ventricular fibrillation** is consistent with severe digitalis-induced arrhythmia.
*Propranolol*
- This is a **beta-blocker** primarily used for hypertension, angina, and arrhythmias.
- While overdose can cause bradycardia, hypotension, and heart block, it typically does not lead to **ventricular tachycardia or fibrillation** as seen in this case.
*Amiodarone*
- This is a **Class III antiarrhythmic** medication with a long half-life, used for various tachyarrhythmias.
- Though it can cause many side effects, including proarrhythmia, it is less likely to present with the classic **GI symptoms** and rapid progression to fatal ventricular arrhythmias seen here, especially in the context of erratic self-dosing and underlying heart failure.
*Lidocaine*
- This is a **Class IB antiarrhythmic** primarily used for ventricular arrhythmias, especially post-myocardial infarction.
- Toxicity typically manifests as **neurological symptoms** (drowsiness, confusion, seizures) and sometimes hypotension or bradycardia, not the wide range of GI and lethal cardiac arrhythmias described.
*Verapamil*
- This is a **calcium channel blocker** used for hypertension, angina, and supraventricular tachycardias.
- Overdose primarily causes **bradycardia, hypotension, and atrioventricular block**, but it is generally not associated with the pronounced GI symptoms or directly triggering ventricular tachycardia/fibrillation like digoxin toxicity.
Electrolyte effects on ECG US Medical PG Question 4: An 8-year-old boy is brought to the emergency department by his parents because of vomiting, abdominal pain, and blurry vision for the past hour. The parents report that the boy developed these symptoms after he accidentally ingested 2 tablets of his grandfather’s heart failure medication. On physical examination, the child is drowsy, and his pulse is 120/min and irregular. Digoxin toxicity is suspected. A blood sample is immediately sent for analysis and shows a serum digoxin level of 4 ng/mL (therapeutic range: 0.8–2 ng/mL). Which of the following electrolyte abnormalities is most likely to be present in the boy?
- A. Hypermagnesemia
- B. Hypokalemia
- C. Hypercalcemia
- D. Hyperkalemia (Correct Answer)
- E. Hypocalcemia
Electrolyte effects on ECG Explanation: ***Hyperkalemia***
- **Digoxin** inhibits the **Na+/K+-ATPase pump**, leading to an increase in intracellular sodium and a decrease in intracellular potassium.
- The decreased function of the Na+/K+-ATPase pump results in reduced cellular uptake of potassium, causing **elevated extracellular potassium** levels.
*Hypermagnesemia*
- **Magnesium** is not directly affected by digoxin toxicity in a way that would lead to hypermagnesemia; in fact, hypomagnesemia can exacerbate digoxin toxicity.
- High magnesium levels are typically associated with renal failure or excessive intake of magnesium-containing antacids or laxatives.
*Hypokalemia*
- While hypokalemia can **predispose to digoxin toxicity** (by increasing digoxin binding to the Na+/K+-ATPase pump), acute digoxin overdose, as described here, often leads to **hyperkalemia** due to the direct inhibition of the pump's ability to drive potassium into cells.
- The classic association of hypokalemia with digoxin refers more to its role as a risk factor for toxicity, especially with diuretic use, rather than a direct consequence of acute overdose.
*Hypercalcemia*
- **Calcium** levels are not directly altered to hypercalcemia by digoxin toxicity.
- Digoxin's mechanism involves increasing intracellular calcium by promoting calcium influx and inhibiting its efflux via the Na+/Ca2+ exchanger, but this typically does not manifest as measurable serum hypercalcemia.
*Hypocalcemia*
- Digoxin toxicity does not directly cause hypocalcemia.
- Digoxin actually leads to **increased intracellular calcium**, which is responsible for its positive inotropic effect, but this change is primarily intracellular and does not result in systemic hypocalcemia.
Electrolyte effects on ECG US Medical PG Question 5: A 58-year-old African-American man with a history of congestive heart failure presents to the emergency room with headache, frequent vomiting, diarrhea, anorexia, and heart palpitations. He is taking a drug that binds the sodium-potassium pump in myocytes. EKG reveals ventricular dysrhythmia. Which of the following is likely also present in the patient?
- A. Angioedema
- B. Changes in color vision (Correct Answer)
- C. Bronchoconstriction
- D. Cough
- E. Decreased PR interval
Electrolyte effects on ECG Explanation: ***Changes in color vision***
- The patient's symptoms (headache, vomiting, diarrhea, anorexia, heart palpitations, ventricular dysrhythmia) and the medication (**cardiac glycoside, like digoxin**) that binds the **sodium-potassium pump** are classic signs of **digoxin toxicity**.
- **Yellow-green vision**, known as xanthopsia, is a highly characteristic and specific visual disturbance associated with digoxin toxicity, often described as seeing halos around lights.
*Angioedema*
- **Angioedema** is an adverse effect commonly associated with **ACE inhibitors** due to their impact on bradykinin metabolism, which is not the drug class described.
- This symptom is unrelated to the mechanism of a sodium-potassium pump inhibitor or cardiac glycoside toxicity.
*Bronchoconstriction*
- **Bronchoconstriction** is a common side effect of **beta-blockers**, especially in patients with reactive airway disease, but not directly linked to cardiac glycosides.
- There is no direct mechanism by which a drug binding the sodium-potassium pump would cause airway narrowing.
*Cough*
- A persistent, dry **cough** is a well-known side effect of **ACE inhibitors**, which increase bradykinin levels.
- This symptom is not characteristic of digoxin toxicity or the action of a sodium-potassium pump inhibitor.
*Decreased PR interval*
- **Digoxin** typically works by **slowing AV nodal conduction**, which would lengthen, not decrease, the **PR interval** (if it were to change significantly due to toxicity, it would be prolongation or AV block).
- A decreased PR interval can be seen in conditions like **Wolff-Parkinson-White syndrome**, or a rapid heart rate.
Electrolyte effects on ECG US Medical PG Question 6: A 32-year-old woman is hospitalized after developing an allergic reaction to the contrast medium used for a cerebral angiography. The study was initially ordered as part of the diagnostic approach of a suspected case of pseudotumor cerebri. Her medical history is unremarkable. On physical examination she has stable vital signs, a diffuse maculopapular rash over her neck and chest, and a mild fever. She is started on hydrocortisone and monitored for the next 8 hours. After the monitoring period, a laboratory test shows significant azotemia. The patient complains of generalized weakness and palpitations. Tall-peaked T waves are observed on ECG. Which of the following explains this clinical manifestation?
- A. Anemia
- B. Platelet dysfunction
- C. Uremic pericarditis
- D. Metabolic acidosis
- E. Hyperkalemia (Correct Answer)
Electrolyte effects on ECG Explanation: ***Hyperkalemia***
- The combination of **significant azotemia** (indicating acute kidney injury), **generalized weakness**, and **peaked T waves on ECG** are classic signs of hyperkalemia.
- The allergic reaction and subsequent treatment may have exacerbated kidney dysfunction, leading to impaired potassium excretion and subsequent elevated serum potassium levels.
*Anemia*
- While anemia can cause weakness and palpitations, it does not typically manifest with **peaked T waves** on ECG or directly explain the presence of **azotemia**.
- Anemia is common in chronic kidney disease but is not the primary cause of acute symptoms and ECG changes described here.
*Platelet dysfunction*
- Uremia can lead to **platelet dysfunction**, causing bleeding tendencies, but it does not account for the **generalized weakness**, **azotemia**, or the characteristic **peaked T waves** on ECG.
- Platelet dysfunction is typically associated with bruising or prolonged bleeding, not the cardiovascular and neurological symptoms observed.
*Uremic pericarditis*
- **Uremic pericarditis** can cause chest pain, a friction rub, and sometimes palpitations, but it does not directly explain the **peaked T waves** or generalized weakness in the context of acute azotemia.
- The primary symptoms of pericarditis are often related to inflammation of the pericardium rather than electrolyte imbalances.
*Metabolic acidosis*
- **Metabolic acidosis** is common in acute kidney injury and can contribute to weakness and dyspnea, but it does not directly cause **peaked T waves** on ECG.
- While clinically important, acidosis itself doesn't explain the specific ECG findings, which are more indicative of hyperkalemia.
Electrolyte effects on ECG US Medical PG Question 7: A 42-year-old man comes to the emergency department because of tingling in his hands and legs and palpitations for 1 week. He has also had severe cramping in his hands, feet, and abdomen during this period. Three months ago, he was hospitalized for acute pancreatitis. He discharged himself against medical advice at that time. There is no family history of illness. He does not smoke. He drinks 2–3 beers and a pint of vodka daily. He has a history of using intravenous heroin. He has not had a stable job for a year. He is only oriented to place and person. His temperature is 37.1°C (98.8°F), pulse is 90/min, and blood pressure is 110/96 mm Hg. There is a carpopedal spasm while measuring his blood pressure. Cardiopulmonary examination shows no abnormalities. Deep tendon reflexes are 4+ bilaterally. Neurologic examination shows no focal findings. Which of the following is the most appropriate pharmacotherapy?
- A. Magnesium sulfate (Correct Answer)
- B. Lorazepam
- C. Sodium bicarbonate
- D. Fomepizole
- E. Vitamin B1 (thiamine)
Electrolyte effects on ECG Explanation: ***Magnesium sulfate***
- The patient exhibits symptoms like **tingling**, **palpitations**, **severe cramping** (hands, feet, abdomen), **carpopedal spasm** (Trousseau's sign), and **hyperreflexia (4+)**, which are classic signs of **hypocalcemia** or **hypomagnesemia**.
- Given his history of **alcohol abuse**, **intravenous drug use**, and recent **pancreatitis**, **hypomagnesemia** is a likely diagnosis, often leading to secondary hypocalcemia. **Magnesium sulfate** is the appropriate treatment.
*Lorazepam*
- Lorazepam is a **benzodiazepine** used to treat seizures, anxiety, and alcohol withdrawal.
- While the patient has a history of alcohol use, his current symptoms are more indicative of electrolyte imbalance (hypomagnesemia/hypocalcemia) rather than acute alcohol withdrawal or seizures.
*Sodium bicarbonate*
- **Sodium bicarbonate** is used to treat metabolic acidosis or certain poisonings.
- There is no indication of acidosis in the given clinical presentation; the symptoms are primarily related to neuromuscular irritability.
*Fomepizole*
- **Fomepizole** is an antidote used in cases of **methanol** or **ethylene glycol poisoning**.
- The patient's presentation does not suggest ingestion of these toxic alcohols.
*Vitamin B1 (thiamine)*
- **Thiamine** is crucial for preventing and treating **Wernicke-Korsakoff syndrome** in patients with chronic alcohol abuse.
- While appropriate for patients with alcohol abuse, it does not directly address the acute neuromuscular irritability and tetany symptoms (tingling, carpopedal spasm, hyperreflexia) observed in this patient.
Electrolyte effects on ECG US Medical PG Question 8: A 67-year-old man with a history of chronic alcoholism presents to the emergency department after a suicide attempt. The patient was found in his apartment by his grandson with wrist lacerations. He was rushed to the emergency department and was resuscitated en route. The patient has a past medical history of ischemic heart disease and depression. His pulse is barely palpable and he is not responding to questions coherently. His temperature is 98.2°F (36.8°C), blood pressure is 107/48 mmHg, pulse is 160/min, respirations are 14/min, and oxygen saturation is 99% on room air. After fluid resuscitation and wound care, his blood pressure improves to 127/55 mmHg. On physical exam, the patient complains of numbness surrounding his mouth and pain in the location of the lacerations of his wrists. Which of the following best describes the laboratory findings in this patient?
- A. Hyperkalemia
- B. Increased free iron
- C. No lab abnormalities
- D. Hypomagnesemia (Correct Answer)
- E. Hypocalcemia
Electrolyte effects on ECG Explanation: ***Hypomagnesemia***
- **Chronic alcoholism** is a significant risk factor for hypomagnesemia due to decreased dietary intake, increased renal excretion, and gastrointestinal losses.
- Clinical signs such as **numbness around the mouth** (circumoral paresthesia), **tachycardia**, and **agitation/confusion** can be manifestations of severe hypomagnesemia, which can also predispose to arrhythmias.
*Hyperkalemia*
- While electrolyte imbalances are common in alcoholism, **hyperkalemia** is less typical in this acute presentation unless associated with other complications like **renal failure** or certain medications.
- The patient's symptoms (numbness, tachycardia) are not classic for hyperkalemia; hyperkalemia often presents with **muscle weakness** or **cardiac arrhythmias** (peaked T waves, widened QRS).
*Increased free iron*
- **Increased free iron** is typically associated with conditions like **hemochromatosis** or acute iron poisoning, neither of which is suggested by the patient's history or symptoms.
- Chronic alcoholism can lead to iron overload in some cases, but this is usually chronic and does not manifest acutely with these neurological or cardiac symptoms.
*No lab abnormalities*
- Given the patient's history of **chronic alcoholism**, presentation with **tachycardia**, altered mental status, and circumoral paresthesia, it is highly unlikely that there would be no laboratory abnormalities.
- Alcoholism frequently leads to significant **electrolyte disturbances** and nutritional deficiencies, making "no lab abnormalities" an improbable finding.
*Hypocalcemia*
- While **hypocalcemia** can cause circumoral paresthesia, it is often secondary to **hypomagnesemia** in alcoholic patients.
- **Hypocalcemia** also typically presents with stronger signs of neuromuscular irritability like **tetany**, **Chvostek's sign**, or **Trousseau's sign**, which are not explicitly mentioned.
Electrolyte effects on ECG US Medical PG Question 9: A 65-year-old woman comes to the physician because of a 3-month history of intermittent palpitations and shortness of breath. Cardiopulmonary examination shows no other abnormalities. An ECG shows an absence of P waves, an oscillating baseline, and irregular RR intervals at a rate of approximately 95 beats per minute. The difference between atrial and ventricular rates in this patient is most likely due to which of the following?
- A. Prolonged influx through voltage-gated Ca2+ channels in the bundle of His
- B. Transient activation of K+ current in Purkinje fibers
- C. Inhibition of the Na+/K+-ATPase pump in ventricular cells
- D. Limited speed of conduction through the left bundle branch
- E. Temporary inactivation of Na+ channels in the AV node (Correct Answer)
Electrolyte effects on ECG Explanation: ***Temporary inactivation of Na+ channels in the AV node***
- The ECG findings are classic for **atrial fibrillation**, characterized by a rapid, irregular atrial rhythm (oscillating baseline with no P waves) and an irregularly irregular ventricular response.
- The **AV node's refractory period** and the number of sodium channels available for conduction dictate the rate at which atrial impulses can pass to the ventricles, preventing a dangerously fast ventricular rate.
*Prolonged influx through voltage-gated Ca2+ channels in the bundle of His*
- The **bundle of His** primarily conducts impulses rather than primarily regulating the rate difference between atria and ventricles through calcium channel kinetics.
- Prolonged calcium influx would generally **slow conduction** or decrease excitability, but it's not the primary mechanism explaining the ventricular rate control in atrial fibrillation.
*Transient activation of K+ current in Purkinje fibers*
- **Purkinje fibers** are involved in rapid ventricular depolarization, but their primary role is not to mediate the rate difference between atria and ventricles in atrial fibrillation.
- Activation of K+ current typically leads to **repolarization**, affecting action potential duration, not the overall filtering of atrial impulses.
*Inhibition of the Na+/K+-ATPase pump in ventricular cells*
- Inhibition of the **Na+/K+-ATPase pump** would lead to intracellular sodium accumulation and depolarization, potentially causing arrhythmias, not regulating the ventricular rate in atrial fibrillation.
- This is the mechanism of action for **digoxin**, which can slow AV nodal conduction but through a different primary pathway affecting the pump.
*Limited speed of conduction through the left bundle branch*
- While conduction system abnormalities can occur, a **limited speed of conduction** specifically in the left bundle branch would cause a wide QRS complex or bundle branch block, not the inherent rate-limiting seen in atrial fibrillation.
- The AV node is the primary regulator of ventricular response rate in atrial fibrillation due to its inherent physiological properties.
Electrolyte effects on ECG US Medical PG Question 10: A researcher is studying how electrical activity propagates across the heart. In order to do this, he decides to measure the rate at which an action potential moves within various groups of cardiac muscle tissue. In particular, he isolates fibers from areas of the heart with the following characteristics:
A) Dysfunction leads to fixed PR intervals prior to a dropped beat
B) Dysfunction leads to increasing PR intervals prior to a dropped beat
C) Dysfunction leads to tachycardia with a dramatically widened QRS complex
D) Dysfunction leads to tachycardia with a sawtooth pattern on electrocardiogram
Which of the following is the proper order of these tissues from fastest action potential propagation to slowest action potential propagation.
- A. B > D > C > A
- B. D > C > A > B
- C. B > C > D > A
- D. A > D > C > B (Correct Answer)
- E. A > C > D > B
Electrolyte effects on ECG Explanation: ***A > D > C > B***
* **Purkinje fibers (A)** have the fastest conduction velocity in the heart to ensure rapid and synchronous ventricular depolarization. The description of "fixed PR intervals prior to a dropped beat" in **Mobitz type II second-degree AV block** indicates an issue with conduction distal to the AV node, often in the His-Purkinje system, while still maintaining typical conduction through the atria and AV node for conducted beats.
* **Atrial muscle (D)** has a faster conduction velocity than the AV node but slower than Purkinje fibers. The "sawtooth pattern on electrocardiogram" unequivocally points to **atrial flutter**, which is characterized by rapid, regular depolarization of the atria.
* **Ventricular muscle (C)** has a conduction velocity slower than Purkinje fibers but faster than the AV node. "Tachycardia with a dramatically widened QRS complex" is characteristic of **ventricular tachycardia (VT)**, which arises from abnormal electrical activity within the ventricles.
* **AV node (B)** has the slowest conduction velocity in the heart, which allows for proper ventricular filling. "Increasing PR intervals prior to a dropped beat" describes **Mobitz type I second-degree AV block (Wenckebach phenomenon)**, which is due to progressive prolongation of conduction delay within the AV node itself.
*B > D > C > A*
* This order incorrectly places the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest, which is contrary to the known conduction velocities in the heart.
* The AV node is critical for delaying the impulse, making it the slowest, while Purkinje fibers are designed for rapid spread, making them the fastest.
*D > C > A > B*
* This option incorrectly places **atrial muscle (D)** as faster than **Purkinje fibers (A)**. Purkinje fibers have the fastest conduction velocity in the heart, considerably faster than atrial muscle.
*B > C > D > A*
* This arrangement incorrectly lists the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest. The AV node is the slowest for its physiological role of delaying ventricular contraction, while Purkinje fibers are optimized for rapid conduction.
*A > C > D > B*
* While placing **Purkinje fibers (A)** as the fastest and the **AV node (B)** as the slowest is correct, this order incorrectly places **ventricular muscle (C)** as faster than **atrial muscle (D)**. Atrial muscle generally conducts faster than ventricular muscle in normal physiology.
More Electrolyte effects on ECG US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.