ECG basics and lead placement US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ECG basics and lead placement. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ECG basics and lead placement US Medical PG Question 1: A 28-year-old male presents with sharp, stabbing chest pain that worsens when lying flat and improves when sitting forward. He reports a recent viral upper respiratory infection 2 weeks ago. On examination, a friction rub is heard on auscultation. His vital signs are stable.
An ECG is most likely to show which of the following findings in this patient?
- A. Diffuse, concave ST-segment elevations (Correct Answer)
- B. Peaked T waves and ST-segment elevations in leads V1-V6
- C. Sawtooth-appearance of P waves
- D. S waves in lead I, Q waves in lead III, and inverted T waves in lead III
- E. Alternating high and low amplitude QRS complexes
ECG basics and lead placement Explanation: ***Diffuse, concave ST-segment elevations***
- This is a hallmark ECG finding in **acute pericarditis**, along with **PR segment depression**, due to widespread inflammation of the epicardium.
- The chest pain described here (sharp, stabbing, worse when lying flat, improved by sitting forward) paired with a recent viral infection and a pericardial friction rub, is highly characteristic of **pericarditis**.
*Peaked T waves and ST-segment elevations in leads V1-V6*
- **Peaked T waves** are typically seen in early stages of hyperkalemia or myocardial ischemia, while **ST-segment elevations in specific leads (V1-V6)** are more indicative of an **ST-elevation myocardial infarction (STEMI)** involving the anterior wall.
- The diffuse nature of ST elevation in pericarditis, as opposed to regional changes, along with **PR depression**, differentiates it from STEMI.
*Sawtooth-appearance of P waves*
- A **sawtooth appearance of P waves** (often referred to as 'f waves') is characteristic of **atrial flutter**, a type of supraventricular tachycardia.
- This finding is unrelated to pericarditis, which primarily affects the pericardium and not the atrial electrical activity in this specific manner.
*S waves in lead I, Q waves in lead III, and inverted T waves in lead III*
- This pattern, known as the **S1Q3T3 pattern**, is a classic (though not always present) ECG finding suggestive of **acute pulmonary embolism**.
- While pulmonary embolism can cause chest pain, its presentation differs significantly from the positional relief and friction rub seen in pericarditis.
*Alternating high and low amplitude QRS complexes*
- This ECG finding, known as **electrical alternans**, is highly specific for a large **pericardial effusion** or **cardiac tamponade**, where the heart swings within the fluid-filled pericardial sac.
- Although pericarditis can lead to effusion, the presence of a friction rub and stable vital signs suggests acute pericarditis without significant tamponade at this stage, making diffuse ST elevation a more likely initial finding.
ECG basics and lead placement US Medical PG Question 2: A 58-year-old man comes to the emergency department for complaints of crushing chest pain for 4 hours. He was shoveling snow outside when the pain started. It is rated 7/10 and radiates to his left arm. An electrocardiogram (ECG) demonstrates ST-segment elevation in leads V2-4. He subsequently undergoes percutaneous coronary intervention (PCI) and is discharged with aspirin, clopidogrel, carvedilol, atorvastatin, and lisinopril. Five days later, the patient is brought to the emergency department by his wife with complaints of dizziness. He reports lightheadedness and palpitations for the past 2 hours but otherwise feels fine. His temperature is 99.7°F (37.6°C), blood pressure is 95/55 mmHg, pulse is 105/min, and respirations are 17/min. A pulmonary artery catheter is performed and demonstrates an increase in oxygen concentration at the pulmonary artery. What finding would you expect in this patient?
- A. Widespread ST-segment elevations
- B. Harsh, loud, holosystolic murmur at the lower left sternal border (Correct Answer)
- C. Pulseless electrical activity
- D. Drop of systolic blood pressure by 20 mmHg during inspiration
- E. Normal findings
ECG basics and lead placement Explanation: ***Harsh, loud, holosystolic murmur at the lower left sternal border***
- This patient's presentation, including recent **anterior STEMI**, dizziness, lightheadedness, palpitations, hypotension, tachycardia, and **increased oxygen saturation in the pulmonary artery** (oxygen "step-up" indicating a left-to-right shunt), is highly suggestive of **ventricular septal rupture (VSR)**.
- VSR is a **mechanical complication** of MI that typically occurs **3-7 days post-infarction** when the necrotic myocardium is weakest.
- A **VSR** causes a **harsh, loud, holosystolic murmur** best heard at the **lower left sternal border** due to turbulent blood flow through the septal defect from the left ventricle to the right ventricle.
- The left-to-right shunt results in oxygenated blood from the left ventricle mixing with deoxygenated blood in the right ventricle, causing the characteristic oxygen saturation step-up detected by pulmonary artery catheterization.
*Widespread ST-segment elevations*
- Widespread ST-segment elevations are characteristic of **acute pericarditis**, which typically presents with **pleuritic chest pain** that improves when leaning forward and a **friction rub**, not the hemodynamic compromise described here.
- While **Dressler syndrome** (post-MI pericarditis) can occur weeks after MI, the acute hemodynamic instability, left-to-right shunt evidence, and 5-day timeframe point to VSR rather than pericarditis.
*Pulseless electrical activity*
- **Pulseless electrical activity (PEA)** indicates cardiac arrest with organized electrical activity but no mechanical cardiac output, resulting in an **unpalpable pulse**.
- The patient has a documented pulse of **105/min**, which directly contradicts PEA.
- A patient in PEA would be unconscious and unable to report symptoms for 2 hours.
*Drop of systolic blood pressure by 20 mmHg during inspiration*
- A drop in systolic blood pressure >10 mmHg during inspiration (**pulsus paradoxus**) is characteristic of **cardiac tamponade** or severe obstructive airway disease.
- While **free wall rupture** leading to tamponade is another mechanical complication post-MI, the **oxygen saturation step-up** in the pulmonary artery is pathognomonic for an **intracardiac shunt** (VSR), not tamponade.
- Tamponade would show equalization of diastolic pressures across all chambers, not increased PA oxygen saturation.
*Normal findings*
- The patient presents with clear evidence of hemodynamic compromise: **hypotension (95/55 mmHg)**, **tachycardia (105/min)**, dizziness, and lightheadedness.
- The **oxygen saturation step-up** in the pulmonary artery is an objective abnormal finding indicating an intracardiac left-to-right shunt.
- Therefore, normal findings are incompatible with this clinical presentation.
ECG basics and lead placement US Medical PG Question 3: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
ECG basics and lead placement Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
ECG basics and lead placement US Medical PG Question 4: A 72-year-old man comes to the physician because of a 2-month history of intermittent retrosternal chest pain and tightness on exertion. He has type 2 diabetes mellitus, osteoarthritis of the right hip, and hypertension. Current medications include insulin, ibuprofen, enalapril, and hydrochlorothiazide. Vital signs are within normal limits. His troponin level is within the reference range. An ECG at rest shows a right bundle branch block and infrequent premature ventricular contractions. The patient's symptoms are reproduced during adenosine stress testing. Repeat ECG during stress testing shows new ST depression of > 1 mm in leads V2, V3, and V4. Which of the following is the most important underlying mechanism of this patient's ECG changes?
- A. Diversion of blood flow from stenotic coronary arteries (Correct Answer)
- B. Transient atrioventricular nodal blockade
- C. Reduced left ventricular preload
- D. Ruptured cholesterol plaque within a coronary vessel
- E. Increased myocardial oxygen demand
ECG basics and lead placement Explanation: ***Diversion of blood flow from stenotic coronary arteries***
- The **adenosine stress test** induces **submaximal coronary vasodilation** in healthy vessels, diverting blood flow away from stenosed areas that are already maximally dilated, a phenomenon known as **coronary steal**.
- This **relative hypoperfusion** in areas supplied by stenotic arteries leads to myocardial ischemia, manifested as **new ST depression** on the ECG due to **subendocardial oxygen supply-demand mismatch**.
*Transient atrioventricular nodal blockade*
- While adenosine can cause transient AV nodal blockade, leading to AV blocks, this would manifest as specific changes in **PR interval** or **QRS drop-out**, not ST segment depression indicative of ischemia.
- The patient's symptoms and ECG changes point towards myocardial ischemia, not an AV conduction disturbance.
*Reduced left ventricular preload*
- Reduced preload can occur in certain cardiac conditions but is not the primary mechanism behind ST depression during an adenosine stress test.
- ECG changes due to reduced preload are usually nonspecific, such as **sinus tachycardia** or **low voltage**, and do not typically cause new ST depression in specific leads.
*Ruptured cholesterol plaque within a coronary vessel*
- A ruptured plaque with subsequent **thrombus formation** would lead to **acute coronary syndrome (ACS)**, characterized by persistent chest pain, **elevated troponins**, and potentially **ST elevation** or new **pathologic Q waves** if complete occlusion occurs.
- The patient's troponin level is normal, and his symptoms are intermittent and reproducible on stress testing, which is more consistent with **stable angina**.
*Increased myocardial oxygen demand*
- While increased myocardial oxygen demand is a component of angina pectoris, adenosine primarily causes **coronary vasodilation**, which can worsen ischemia in stenotic areas by diverting blood flow, rather than directly increasing myocardial oxygen demand itself.
- **Dobutamine stress testing** would be the test that primarily increases myocardial oxygen demand.
ECG basics and lead placement US Medical PG Question 5: A 50-year-old man presents the emergency department for intense chest pain, profuse sweating, and shortness of breath. The onset of these symptoms was 3 hours ago. The chest pain began after a heated discussion with a colleague at the community college where he is employed. Upon arrival, he is found conscious and responsive; the vital signs include a blood pressure of 130/80 mm Hg, a heart rate at 90/min, a respiratory rate at 20/min, and a body temperature of 36.4°C (97.5°F). His medical history is significant for hypertension diagnosed 7 years ago, which is well-controlled with a calcium channel blocker. The initial electrocardiogram (ECG) shows ST-segment depression in multiple consecutive leads, an elevated cardiac troponin T level, and normal kidney function. Which of the following would you expect to find in this patient?
- A. Subendocardial necrosis (Correct Answer)
- B. Transmural necrosis
- C. Incomplete occlusion of a coronary artery
- D. Coronary artery spasm
- E. Ventricular pseudoaneurysm
ECG basics and lead placement Explanation: ***Subendocardial necrosis***
- This patient's presentation with **ST-segment depression** and **elevated troponin T** indicates a **Non-ST-segment Elevation Myocardial Infarction (NSTEMI)**, which typically results from subendocardial ischemia and necrosis.
- Subendocardial tissue is most vulnerable to ischemia due to its high oxygen demand and distal location from the coronary arteries, making it the first region to suffer damage when oxygen supply is compromised.
*Transmural necrosis*
- **Transmural necrosis** is characteristic of a **ST-segment Elevation Myocardial Infarction (STEMI)**, which presents with persistent **ST-segment elevation** on ECG.
- This patient's ECG shows **ST-segment depression**, ruling out transmural involvement at the time of presentation.
*Incomplete occlusion of a coronary artery*
- While an NSTEMI usually involves an **incomplete occlusion** or **critical stenosis** of a coronary artery, the question asks what would be *found* in the patient's heart tissue, not the mechanism.
- The direct tissue consequence of incomplete occlusion leading to NSTEMI is **subendocardial necrosis**, which is a more specific answer about the pathological finding.
*Coronary artery spasm*
- Although **coronary artery spasm (Prinzmetal angina)** can cause chest pain and ECG changes, it typically presents with **transient ST-segment elevation** (not depression) and often resolves spontaneously.
- The elevated troponin T indicates myocardial necrosis, which is not typically a feature of uncomplicated coronary artery spasm, and the duration of symptoms (3 hours) suggests a more sustained event than a transient spasm.
*Ventricular pseudoaneurysm*
- A **ventricular pseudoaneurysm** is a **late complication of myocardial infarction**, typically occurring weeks to months after the acute event, due to rupture of the ventricular free wall contained by pericardium.
- Given the 3-hour symptom onset, it is highly unlikely to be present in the acute phase of myocardial infarction.
ECG basics and lead placement US Medical PG Question 6: A 55-year-old man comes to the emergency department because of left-sided chest pain and difficulty breathing for the past 30 minutes. His pulse is 88/min. He is pale and anxious. Serum studies show increased cardiac enzymes. An ECG shows ST-elevations in leads I, aVL, and V5-V6. A percutaneous coronary intervention is performed. In order to localize the site of the lesion, the catheter must pass through which of the following structures?
- A. Left coronary artery → left circumflex artery (Correct Answer)
- B. Right coronary artery → posterior descending artery
- C. Left coronary artery → left anterior descending artery
- D. Right coronary artery → right marginal artery
- E. Left coronary artery → posterior descending artery
ECG basics and lead placement Explanation: ***Left coronary artery → left circumflex artery***
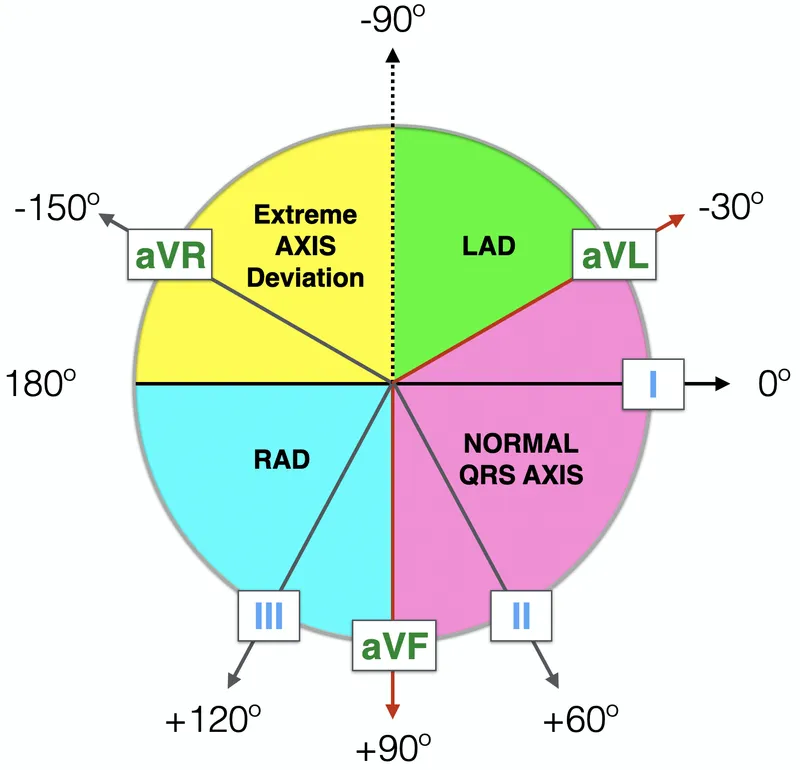
- **ST-elevations** in leads I, aVL, and V5-V6 are indicative of a **lateral myocardial infarction**.
- The **left circumflex artery** primarily supplies the lateral wall of the left ventricle.
*Right coronary artery → posterior descending artery*
- The **posterior descending artery** (PDA) typically supplies the inferior wall and posterior interventricular septum.
- An occlusion here would cause **ST-elevations** in leads II, III, and aVF, which is not seen in this case.
*Left coronary artery → left anterior descending artery*
- The **left anterior descending** (LAD) artery supplies the anterior wall and apex of the left ventricle.
- Occlusion of the LAD would typically cause **ST-elevations** in leads V1-V4, indicating an anterior MI.
*Right coronary artery → right marginal artery*
- The **right marginal artery** is a branch of the right coronary artery and supplies part of the right ventricle.
- Occlusion here would primarily affect the **right ventricle**, and is not typically associated with the given ECG changes.
*Left coronary artery → posterior descending artery*
- While the **posterior descending artery** can sometimes originate from the left circumflex artery (**left dominant circulation**), it primarily supplies the inferior wall.
- The observed ECG changes in leads I, aVL, and V5-V6 are characteristic of a **lateral wall infarct**, which is supplied by the left circumflex artery.
ECG basics and lead placement US Medical PG Question 7: An abnormal wave is noted on a routine ECG. The wave in question represents which of the following electrical events in the cardiac cycle?
- A. Period between ventricular depolarization and repolarization
- B. Atrial repolarization
- C. Ventricular repolarization (Correct Answer)
- D. Ventricular depolarization
- E. Atrial depolarization
ECG basics and lead placement Explanation: ***Ventricular repolarization***
- The **T wave** represents ventricular repolarization, which is the electrical recovery phase of the ventricles after contraction
- T wave abnormalities are among the most common ECG findings and include **T wave inversions** (myocardial ischemia, ventricular hypertrophy), **peaked T waves** (hyperkalemia), **flattened T waves** (hypokalemia, ischemia), and **biphasic T waves**
- The T wave corresponds to **phase 3** of the ventricular action potential when potassium channels open and the membrane repolarizes
*Period between ventricular depolarization and repolarization*
- This describes the **ST segment**, which represents the period when ventricles are completely depolarized before repolarization begins
- The **QT interval** encompasses both ventricular depolarization and repolarization (QRS + ST segment + T wave)
- These are intervals or segments, not waves
*Atrial repolarization*
- Atrial repolarization occurs during ventricular depolarization and is represented by the **Ta wave**
- This wave is typically **not visible** on standard ECG because it is **masked by the much larger QRS complex** and has very low amplitude
- It cannot be identified as a distinct wave on routine ECGs
*Ventricular depolarization*
- The **QRS complex** represents ventricular depolarization, the electrical activation that triggers ventricular contraction
- Normal QRS duration is **0.06-0.10 seconds** (3 small boxes or less)
- QRS abnormalities include bundle branch blocks, ventricular hypertrophy patterns, and pre-excitation
*Atrial depolarization*
- The **P wave** represents atrial depolarization, the electrical activation that triggers atrial contraction
- Normal P wave characteristics: **upright in leads I, II, aVF**; duration less than 0.12 seconds; amplitude less than 2.5 mm
- P wave abnormalities include left atrial enlargement (broad, notched P waves) and right atrial enlargement (tall, peaked P waves)
ECG basics and lead placement US Medical PG Question 8: A researcher is studying how electrical activity propagates across the heart. In order to do this, he decides to measure the rate at which an action potential moves within various groups of cardiac muscle tissue. In particular, he isolates fibers from areas of the heart with the following characteristics:
A) Dysfunction leads to fixed PR intervals prior to a dropped beat
B) Dysfunction leads to increasing PR intervals prior to a dropped beat
C) Dysfunction leads to tachycardia with a dramatically widened QRS complex
D) Dysfunction leads to tachycardia with a sawtooth pattern on electrocardiogram
Which of the following is the proper order of these tissues from fastest action potential propagation to slowest action potential propagation.
- A. B > D > C > A
- B. D > C > A > B
- C. B > C > D > A
- D. A > D > C > B (Correct Answer)
- E. A > C > D > B
ECG basics and lead placement Explanation: ***A > D > C > B***
* **Purkinje fibers (A)** have the fastest conduction velocity in the heart to ensure rapid and synchronous ventricular depolarization. The description of "fixed PR intervals prior to a dropped beat" in **Mobitz type II second-degree AV block** indicates an issue with conduction distal to the AV node, often in the His-Purkinje system, while still maintaining typical conduction through the atria and AV node for conducted beats.
* **Atrial muscle (D)** has a faster conduction velocity than the AV node but slower than Purkinje fibers. The "sawtooth pattern on electrocardiogram" unequivocally points to **atrial flutter**, which is characterized by rapid, regular depolarization of the atria.
* **Ventricular muscle (C)** has a conduction velocity slower than Purkinje fibers but faster than the AV node. "Tachycardia with a dramatically widened QRS complex" is characteristic of **ventricular tachycardia (VT)**, which arises from abnormal electrical activity within the ventricles.
* **AV node (B)** has the slowest conduction velocity in the heart, which allows for proper ventricular filling. "Increasing PR intervals prior to a dropped beat" describes **Mobitz type I second-degree AV block (Wenckebach phenomenon)**, which is due to progressive prolongation of conduction delay within the AV node itself.
*B > D > C > A*
* This order incorrectly places the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest, which is contrary to the known conduction velocities in the heart.
* The AV node is critical for delaying the impulse, making it the slowest, while Purkinje fibers are designed for rapid spread, making them the fastest.
*D > C > A > B*
* This option incorrectly places **atrial muscle (D)** as faster than **Purkinje fibers (A)**. Purkinje fibers have the fastest conduction velocity in the heart, considerably faster than atrial muscle.
*B > C > D > A*
* This arrangement incorrectly lists the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest. The AV node is the slowest for its physiological role of delaying ventricular contraction, while Purkinje fibers are optimized for rapid conduction.
*A > C > D > B*
* While placing **Purkinje fibers (A)** as the fastest and the **AV node (B)** as the slowest is correct, this order incorrectly places **ventricular muscle (C)** as faster than **atrial muscle (D)**. Atrial muscle generally conducts faster than ventricular muscle in normal physiology.
ECG basics and lead placement US Medical PG Question 9: A 65-year-old woman comes to the physician because of a 3-month history of intermittent palpitations and shortness of breath. Cardiopulmonary examination shows no other abnormalities. An ECG shows an absence of P waves, an oscillating baseline, and irregular RR intervals at a rate of approximately 95 beats per minute. The difference between atrial and ventricular rates in this patient is most likely due to which of the following?
- A. Prolonged influx through voltage-gated Ca2+ channels in the bundle of His
- B. Transient activation of K+ current in Purkinje fibers
- C. Inhibition of the Na+/K+-ATPase pump in ventricular cells
- D. Limited speed of conduction through the left bundle branch
- E. Temporary inactivation of Na+ channels in the AV node (Correct Answer)
ECG basics and lead placement Explanation: ***Temporary inactivation of Na+ channels in the AV node***
- The ECG findings are classic for **atrial fibrillation**, characterized by a rapid, irregular atrial rhythm (oscillating baseline with no P waves) and an irregularly irregular ventricular response.
- The **AV node's refractory period** and the number of sodium channels available for conduction dictate the rate at which atrial impulses can pass to the ventricles, preventing a dangerously fast ventricular rate.
*Prolonged influx through voltage-gated Ca2+ channels in the bundle of His*
- The **bundle of His** primarily conducts impulses rather than primarily regulating the rate difference between atria and ventricles through calcium channel kinetics.
- Prolonged calcium influx would generally **slow conduction** or decrease excitability, but it's not the primary mechanism explaining the ventricular rate control in atrial fibrillation.
*Transient activation of K+ current in Purkinje fibers*
- **Purkinje fibers** are involved in rapid ventricular depolarization, but their primary role is not to mediate the rate difference between atria and ventricles in atrial fibrillation.
- Activation of K+ current typically leads to **repolarization**, affecting action potential duration, not the overall filtering of atrial impulses.
*Inhibition of the Na+/K+-ATPase pump in ventricular cells*
- Inhibition of the **Na+/K+-ATPase pump** would lead to intracellular sodium accumulation and depolarization, potentially causing arrhythmias, not regulating the ventricular rate in atrial fibrillation.
- This is the mechanism of action for **digoxin**, which can slow AV nodal conduction but through a different primary pathway affecting the pump.
*Limited speed of conduction through the left bundle branch*
- While conduction system abnormalities can occur, a **limited speed of conduction** specifically in the left bundle branch would cause a wide QRS complex or bundle branch block, not the inherent rate-limiting seen in atrial fibrillation.
- The AV node is the primary regulator of ventricular response rate in atrial fibrillation due to its inherent physiological properties.
ECG basics and lead placement US Medical PG Question 10: An investigator develops a new drug that decreases the number of voltage-gated potassium channels in cardiac muscle cell membranes. Which of the following is the most likely effect of this drug on the myocardial action potential?
- A. Delayed repolarization (Correct Answer)
- B. Delayed depolarization
- C. Accelerated repolarization
- D. Decreased resting membrane potential
- E. Accelerated depolarization
ECG basics and lead placement Explanation: ***Delayed repolarization***
- **Voltage-gated potassium channels** are primarily responsible for the efflux of potassium ions during the **repolarization phase** (phase 3) of the cardiac action potential.
- A decrease in the number of these channels would reduce potassium efflux, thus slowing down the repolarization process and prolonging the **action potential duration**.
*Delayed depolarization*
- **Depolarization** (phase 0) of the cardiac action potential is primarily mediated by the rapid influx of **sodium ions** through voltage-gated sodium channels.
- Changes in potassium channels do not directly affect the speed of depolarization.
*Accelerated repolarization*
- Accelerated repolarization would occur if there were an *increase* in the number or activity of **potassium channels**, leading to a faster efflux of potassium ions.
- A *decrease* in these channels would have the opposite effect.
*Decreased resting membrane potential*
- The **resting membrane potential** is primarily maintained by the **leak potassium channels** and the **Na+/K+ ATPase pump**, not directly by voltage-gated potassium channels involved in repolarization.
- A decrease in voltage-gated potassium channels would not significantly alter the resting membrane potential.
*Accelerated depolarization*
- Accelerated depolarization would result from an *increase* in the speed or magnitude of **sodium influx** during phase 0.
- A reduction in potassium channels has no direct impact on the rate of sodium channel activation or current.
More ECG basics and lead placement US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.