Common arrhythmia recognition US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Common arrhythmia recognition. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
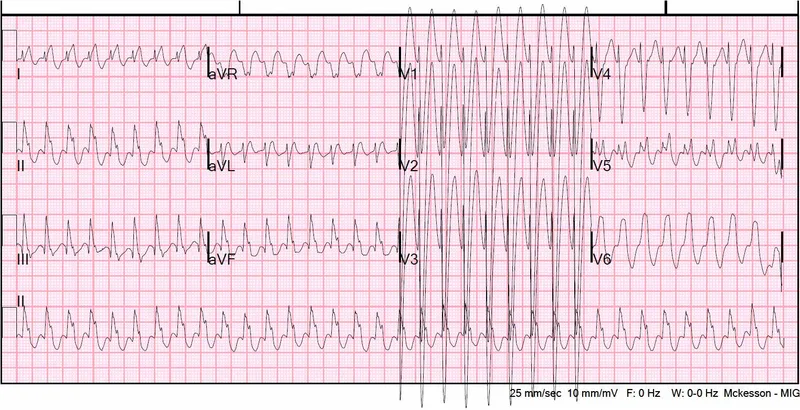
Common arrhythmia recognition US Medical PG Question 1: A 62-year-old man is brought to the emergency department because of syncope. He reports sudden onset of palpitations followed by loss of consciousness while carrying his groceries to his car. He is unable to recall any further details and does not have any chest pain or dizziness. He has a history of hypertension, type 2 diabetes mellitus, gastroparesis, and osteoarthritis of the knees. Medications include lisinopril, metformin, and ondansetron as needed for nausea. He also takes methadone daily for chronic pain. Apart from an abrasion on his forehead, he appears well. His temperature is 37.2 °C (98.9 F), heart rate is 104/min and regular, and blood pressure is 135/70 mm Hg. While he is in the emergency department, he loses consciousness again. Telemetry shows polymorphic ventricular tachycardia with cyclic alteration of the QRS axis that spontaneously resolves after 30 seconds. Results of a complete blood count, serum electrolyte concentrations, and serum thyroid studies show no abnormalities. Cardiac enzymes are within normal limits. Which of the following is the most likely underlying cause of this patient's syncope?
- A. Prinzmetal angina
- B. Fast accessory conduction pathway
- C. Brugada syndrome
- D. Prolonged QT interval (Correct Answer)
- E. Hypomagnesemia
Common arrhythmia recognition Explanation: ***Prolonged QT interval***
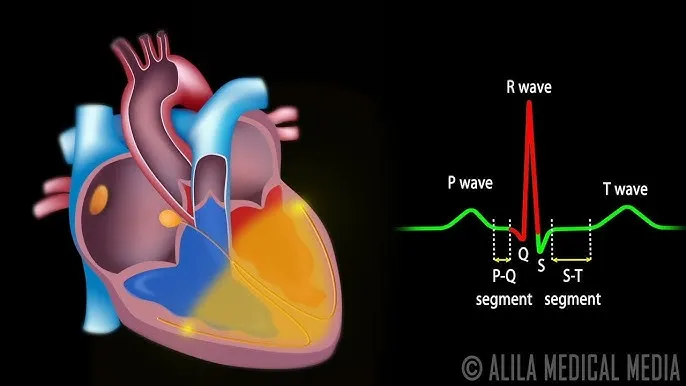
- The patient experienced **polymorphic ventricular tachycardia** with cyclic alteration of the **QRS axis** (Torsades de Pointes), which is characteristic of a prolonged QT interval.
- **Methadone is known to prolong the QT interval**, and the patient's history of syncope preceded by palpitations is consistent with this arrhythmia.
*Prinzmetal angina*
- Prinzmetal angina involves **coronary artery spasm**, leading to **transient myocardial ischemia**, typically causing chest pain, not primarily syncope from polymorphic VT.
- While it can cause arrhythmias, the characteristic EKG finding would be **ST-segment elevation during pain**, which is not described.
*Fast accessory conduction pathway*
- A fast accessory pathway (e.g., in Wolfe-Parkinson-White syndrome) can lead to **AV reentrant tachycardia** or **pre-excitation** with atrial fibrillation, but not typically polymorphic VT with cyclic QRS alteration.
- The EKG would show a **delta wave** and a short PR interval, which is not mentioned.
*Brugada syndrome*
- Brugada syndrome is an inherited channelopathy **characterized by specific EKG patterns** (e.g., coved-type ST elevation in V1-V3) and an increased risk of sudden cardiac death due to ventricular arrhythmias.
- The patient's EKG findings of polymorphic VT with cyclic QRS alteration are not typical of Brugada syndrome-induced arrhythmia.
*Hypomagnesemia*
- While **hypomagnesemia can prolong the QT interval** and lead to Torsades de Pointes, the patient's **serum electrolyte concentrations were normal**, ruling out this direct cause.
- Magnesium levels would need to be critically low for such an effect, and this is typically detected on blood tests.
Common arrhythmia recognition US Medical PG Question 2: A 72-year-old man with congestive heart failure is brought to the emergency department because of chest pain, shortness of breath, dizziness, and palpitations for 30 minutes. An ECG shows a wide complex tachycardia with a P-wave rate of 105/min, an R-wave rate of 130/min, and no apparent relation between the two. Intravenous pharmacotherapy is initiated with a drug that prolongs the QRS and QT intervals. The patient was most likely treated with which of the following drugs?
- A. Carvedilol
- B. Verapamil
- C. Flecainide
- D. Quinidine (Correct Answer)
- E. Sotalol
Common arrhythmia recognition Explanation: **Quinidine**
- Quinidine is a **Class IA antiarrhythmic** that blocks fast sodium channels, prolonging both the **QRS complex** (due to slowed conduction) and the **QT interval** (due to prolonged repolarization).
- The ECG findings of **wide-complex tachycardia** and **AV dissociation** (P-wave rate different from R-wave rate without apparent relation) are consistent with ventricular tachycardia, which Class IA drugs can treat.
*Carvedilol*
- Carvedilol is a **beta-blocker** (Class II antiarrhythmic) that primarily slows heart rate and AV nodal conduction, generally **shortening the QT interval** or having no effect, and would not widen the QRS complex.
- Beta-blockers are typically contraindicated in **decompensated heart failure** and **wide-complex tachycardia** due to their negative inotropic effects and risk of worsening decompensation.
*Verapamil*
- Verapamil is a **non-dihydropyridine calcium channel blocker** (Class IV antiarrhythmic) that mainly slows AV nodal conduction. It would not cause QRS widening and can shorten the QT interval.
- Verapamil is generally contraindicated in **wide-complex tachycardias** of unknown origin as it can precipitate cardiovascular collapse if the arrhythmia is ventricular.
*Flecainide*
- Flecainide is a **Class IC antiarrhythmic** that primarily blocks fast sodium channels, causing significant **QRS widening** but has **minimal effect on the QT interval**, which is contrary to the case description.
- Class IC agents are also generally avoided in patients with **structural heart disease** like congestive heart failure due to increased mortality risk.
*Sotalol*
- Sotalol is a **Class III antiarrhythmic** (beta-blocker with potassium channel blockade) that primarily prolongs the **QT interval** by blocking potassium channels. While it prolongs the QT, it does **not significantly widen the QRS complex**.
- Its beta-blocking effects could exacerbate **decompensated heart failure** in this patient, similar to carvedilol.
Common arrhythmia recognition US Medical PG Question 3: A 65-year-old woman comes to the physician because of a 3-month history of intermittent palpitations and shortness of breath. Cardiopulmonary examination shows no other abnormalities. An ECG shows an absence of P waves, an oscillating baseline, and irregular RR intervals at a rate of approximately 95 beats per minute. The difference between atrial and ventricular rates in this patient is most likely due to which of the following?
- A. Prolonged influx through voltage-gated Ca2+ channels in the bundle of His
- B. Transient activation of K+ current in Purkinje fibers
- C. Inhibition of the Na+/K+-ATPase pump in ventricular cells
- D. Limited speed of conduction through the left bundle branch
- E. Temporary inactivation of Na+ channels in the AV node (Correct Answer)
Common arrhythmia recognition Explanation: ***Temporary inactivation of Na+ channels in the AV node***
- The ECG findings are classic for **atrial fibrillation**, characterized by a rapid, irregular atrial rhythm (oscillating baseline with no P waves) and an irregularly irregular ventricular response.
- The **AV node's refractory period** and the number of sodium channels available for conduction dictate the rate at which atrial impulses can pass to the ventricles, preventing a dangerously fast ventricular rate.
*Prolonged influx through voltage-gated Ca2+ channels in the bundle of His*
- The **bundle of His** primarily conducts impulses rather than primarily regulating the rate difference between atria and ventricles through calcium channel kinetics.
- Prolonged calcium influx would generally **slow conduction** or decrease excitability, but it's not the primary mechanism explaining the ventricular rate control in atrial fibrillation.
*Transient activation of K+ current in Purkinje fibers*
- **Purkinje fibers** are involved in rapid ventricular depolarization, but their primary role is not to mediate the rate difference between atria and ventricles in atrial fibrillation.
- Activation of K+ current typically leads to **repolarization**, affecting action potential duration, not the overall filtering of atrial impulses.
*Inhibition of the Na+/K+-ATPase pump in ventricular cells*
- Inhibition of the **Na+/K+-ATPase pump** would lead to intracellular sodium accumulation and depolarization, potentially causing arrhythmias, not regulating the ventricular rate in atrial fibrillation.
- This is the mechanism of action for **digoxin**, which can slow AV nodal conduction but through a different primary pathway affecting the pump.
*Limited speed of conduction through the left bundle branch*
- While conduction system abnormalities can occur, a **limited speed of conduction** specifically in the left bundle branch would cause a wide QRS complex or bundle branch block, not the inherent rate-limiting seen in atrial fibrillation.
- The AV node is the primary regulator of ventricular response rate in atrial fibrillation due to its inherent physiological properties.
Common arrhythmia recognition US Medical PG Question 4: A 40-year-old woman comes to the physician for a 6-month history of recurrent episodes of chest pain, racing pulse, dizziness, and difficulty breathing. The episodes last up to several minutes. She also reports urinary urgency and two episodes of loss of consciousness followed by spontaneous recovery. There is no personal or family history of serious illness. She does not smoke or drink alcohol. Vitals signs are within normal limits. Cardiopulmonary examination shows no abnormalities. Holter monitoring is performed. ECG recordings during episodes of tachycardia show a QRS duration of 100 ms, regular RR-interval, and absent P waves. Which of the following is the most likely underlying cause of this patient's condition?
- A. AV node with slow and fast pathway (Correct Answer)
- B. Pre-excitation of the ventricles
- C. Mutations in genes that code for myocyte ion channels
- D. Macroreentrant rhythm in the right atria through cavotricuspid isthmus
- E. Fibrosis of the sinoatrial node and surrounding myocardium
Common arrhythmia recognition Explanation: ***AV node with slow and fast pathway***
- This describes **AV nodal reentrant tachycardia (AVNRT)**, a common cause of **paroxysmal supraventricular tachycardia (PSVT)**. The ECG findings of **narrow QRS (100 ms)**, regular RR-interval, and **absent P waves** (often hidden within the QRS complex) are characteristic of AVNRT.
- The patient's symptoms of recurrent chest pain, racing pulse, dizziness, and spontaneous recovery from loss of consciousness fit the episodic nature of **AVNRT**. The presence of two pathways (slow and fast) within the AV node facilitates the reentrant circuit.
*Pre-excitation of the ventricles*
- **Pre-excitation syndromes** (e.g., Wolff-Parkinson-White syndrome) involve an accessory pathway that bypasses the AV node, leading to a **delta wave** and **short PR interval** on the baseline ECG.
- While they can cause SVT, the ECG during tachycardia would typically show a **wide QRS complex** if the accessory pathway is part of the reentrant circuit (antidromic), or a narrow QRS with a visible P wave if orthodromic and the accessory pathway is used for retrograde conduction, which doesn't fully align with the absent P waves and typically *normal* QRS during tachycardia as described.
*Mutations in genes that code for myocyte ion channels*
- This refers to **channelopathies** (e.g., long QT syndrome, Brugada syndrome), which predispose to **ventricular arrhythmias** like **polymorphic ventricular tachycardia** and **ventricular fibrillation**.
- These conditions typically cause **wide QRS tachycardias** and have distinct ECG patterns (e.g., prolonged QT interval, Brugada pattern) not described here. The narrow QRS and regular rhythm point away from primary ventricular channelopathies as the cause of this specific tachycardia.
*Macroreentrant rhythm in the right atria through cavotricuspid isthmus*
- This describes **atrial flutter**, which typically presents with characteristic **"sawtooth" F waves** on ECG, representing atrial activity.
- While atrial flutter can cause recurrent episodes of rapid heart rate, the ECG description of **absent P waves** and a **narrow QRS complex** without F waves makes atrial flutter less likely.
*Fibrosis of the sinoatrial node and surrounding myocardium*
- **Sinoatrial node dysfunction (sick sinus syndrome)** can lead to bradycardia, sinus pauses, or alternating bradycardia and tachycardia (tachy-brady syndrome).
- It does not primarily cause the described paroxysmal narrow-complex tachycardia with absent P waves. The patient's symptoms are more consistent with an abrupt-onset, regular supraventricular tachycardia.
Common arrhythmia recognition US Medical PG Question 5: A 42-year-old Caucasian woman is enrolled in a randomized controlled trial to study cardiac function in the setting of several different drugs. She is started on verapamil and instructed to exercise at 50% of her VO2 max while several cardiac parameters are being measured. During this experiment, which of the following represents the relative conduction speed through the heart from fastest to slowest?
- A. Purkinje fibers > ventricles > atria > AV node
- B. Purkinje fibers > atria > ventricles > AV node (Correct Answer)
- C. Atria > Purkinje fibers > ventricles > AV node
- D. AV node > ventricles > atria > Purkinje fibers
- E. Purkinje fibers > AV node > ventricles > atria
Common arrhythmia recognition Explanation: ***Purkinje fibers > atria > ventricles > AV node***
- The **Purkinje fibers** have the fastest conduction velocity, ensuring rapid and synchronous ventricular depolarization.
- The **atria** conduct impulses faster than the ventricles, but slower than the Purkinje fibers, allowing for atrial contraction before ventricular systole.
*Purkinje fibers > ventricles > atria > AV node*
- This option correctly identifies the **Purkinje fibers** and **AV node** at the fastest and slowest ends, respectively, but incorrectly orders the atria and ventricles.
- While Purkinje fibers are fastest, cardiac muscle cells (atria then ventricles) conduct slower than Purkinje fibers.
*Atria > Purkinje fibers > ventricles > AV node*
- This option incorrectly places the **atria** as having the fastest conduction speed, which is not true as Purkinje fibers are significantly faster.
- It also misorders the Purkinje fibers relative to the atria in terms of speed.
*AV node > ventricles > atria > Purkinje fibers*
- This option is incorrect as it places the **AV node** as the fastest conductor and the **Purkinje fibers** as the slowest, which is the exact opposite of their actual conduction speeds.
- The AV node is known for its slow conduction to allow for ventricular filling.
*Purkinje fibers > AV node > ventricles > atria*
- This option incorrectly places the **AV node** as the second fastest conductor, and the ventricles as slower than the atria.
- The AV node is specifically designed to slow the impulse to allow for proper ventricular filling.
Common arrhythmia recognition US Medical PG Question 6: A researcher is studying how electrical activity propagates across the heart. In order to do this, he decides to measure the rate at which an action potential moves within various groups of cardiac muscle tissue. In particular, he isolates fibers from areas of the heart with the following characteristics:
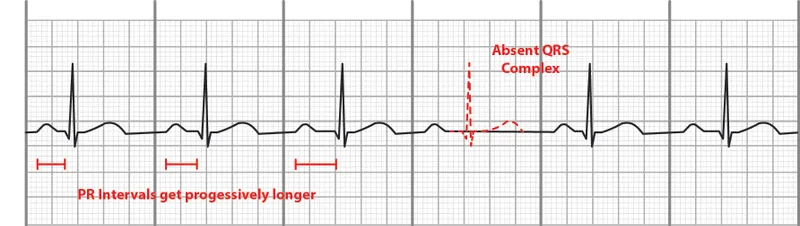
A) Dysfunction leads to fixed PR intervals prior to a dropped beat
B) Dysfunction leads to increasing PR intervals prior to a dropped beat
C) Dysfunction leads to tachycardia with a dramatically widened QRS complex
D) Dysfunction leads to tachycardia with a sawtooth pattern on electrocardiogram
Which of the following is the proper order of these tissues from fastest action potential propagation to slowest action potential propagation.
- A. B > D > C > A
- B. D > C > A > B
- C. B > C > D > A
- D. A > D > C > B (Correct Answer)
- E. A > C > D > B
Common arrhythmia recognition Explanation: ***A > D > C > B***
* **Purkinje fibers (A)** have the fastest conduction velocity in the heart to ensure rapid and synchronous ventricular depolarization. The description of "fixed PR intervals prior to a dropped beat" in **Mobitz type II second-degree AV block** indicates an issue with conduction distal to the AV node, often in the His-Purkinje system, while still maintaining typical conduction through the atria and AV node for conducted beats.
* **Atrial muscle (D)** has a faster conduction velocity than the AV node but slower than Purkinje fibers. The "sawtooth pattern on electrocardiogram" unequivocally points to **atrial flutter**, which is characterized by rapid, regular depolarization of the atria.
* **Ventricular muscle (C)** has a conduction velocity slower than Purkinje fibers but faster than the AV node. "Tachycardia with a dramatically widened QRS complex" is characteristic of **ventricular tachycardia (VT)**, which arises from abnormal electrical activity within the ventricles.
* **AV node (B)** has the slowest conduction velocity in the heart, which allows for proper ventricular filling. "Increasing PR intervals prior to a dropped beat" describes **Mobitz type I second-degree AV block (Wenckebach phenomenon)**, which is due to progressive prolongation of conduction delay within the AV node itself.
*B > D > C > A*
* This order incorrectly places the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest, which is contrary to the known conduction velocities in the heart.
* The AV node is critical for delaying the impulse, making it the slowest, while Purkinje fibers are designed for rapid spread, making them the fastest.
*D > C > A > B*
* This option incorrectly places **atrial muscle (D)** as faster than **Purkinje fibers (A)**. Purkinje fibers have the fastest conduction velocity in the heart, considerably faster than atrial muscle.
*B > C > D > A*
* This arrangement incorrectly lists the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest. The AV node is the slowest for its physiological role of delaying ventricular contraction, while Purkinje fibers are optimized for rapid conduction.
*A > C > D > B*
* While placing **Purkinje fibers (A)** as the fastest and the **AV node (B)** as the slowest is correct, this order incorrectly places **ventricular muscle (C)** as faster than **atrial muscle (D)**. Atrial muscle generally conducts faster than ventricular muscle in normal physiology.
Common arrhythmia recognition US Medical PG Question 7: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Common arrhythmia recognition Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Common arrhythmia recognition US Medical PG Question 8: A 33-year-old man is evaluated by paramedics after being found unconscious outside of his home. He has no palpable pulses. Physical examination shows erythematous marks in a fern-leaf pattern on his lower extremities. An ECG shows ventricular fibrillation. Which of the following is the most likely cause of this patient's findings?
- A. Infective endocarditis
- B. Lightning strike (Correct Answer)
- C. Opioid overdose
- D. Hypothermia
- E. Cholesterol emboli
Common arrhythmia recognition Explanation: ***Lightning strike***
- The **fern-leaf pattern** on the skin, known as **Lichtenberg figures**, is pathognomonic for a lightning strike.
- **Ventricular fibrillation** is a common and often fatal cardiac arrhythmia caused by the massive electrical discharge from lightning.
*Infective endocarditis*
- While it can cause cardiac arrhythmias or collapse due to **embolism**, it does not produce **Lichtenberg figures**.
- Typical signs include **fever**, **murmurs**, and **Osler's nodes** or **Janeway lesions**, which are not mentioned here.
*Opioid overdose*
- Leads to **respiratory depression**, **miosis (pinpoint pupils)**, and potentially **bradycardia**, but not ventricular fibrillation or fern-leaf skin patterns.
- The patient would typically present with a **depressed level of consciousness** but usually has palpable pulses initially.
*Hypothermia*
- Can cause cardiac arrhythmias, including **ventricular fibrillation** in severe cases, but would not produce **Lichtenberg figures**.
- The patient's skin would typically be **cold to the touch**, and there might be **J-waves** on the ECG.
*Cholesterol emboli*
- Typically results in widespread **ischemic symptoms** in various organs and can cause skin manifestations like **livedo reticularis** or **"trash foot"**.
- It does not cause **ventricular fibrillation** or the characteristic **fern-leaf pattern** seen in lightning strike victims.
Common arrhythmia recognition US Medical PG Question 9: Cardiac muscle serves many necessary functions, leading to a specific structure that serves these functions. The structure highlighted is an important histology component of cardiac muscle. What would be the outcome if this structure diffusely failed to function?
- A. Failure of potassium channels to appropriately open to repolarize the cell
- B. Failure of propagation of the action potential from the conduction system (Correct Answer)
- C. Ineffective excitation-contraction coupling due to insufficient calcium ions
- D. Inappropriate formation of cardiac valve leaflets
- E. Outflow tract obstruction
Common arrhythmia recognition Explanation: ***Failure of propagation of the action potential from the conduction system***
- The highlighted structure, the **intercalated disc**, contains **gap junctions** which are crucial for the rapid, synchronized spread of **action potentials** between cardiac muscle cells.
- A diffuse failure of these structures would prevent the coordinated electrical activation of the myocardium, leading to a failure of impulse propagation and **compromised cardiac contraction**.
*Failure of potassium channels to appropriately open to repolarize the cell*
- This scenario describes a problem with **ion channel function** within individual cardiomyocytes, affecting their repolarization phase.
- While critical for a single cell's electrical activity, it does not directly relate to the primary function of **intercalated discs** in *propagating* action potentials across multiple cells.
*Ineffective excitation-contraction coupling due to insufficient calcium ions*
- This outcome would result from issues with **calcium handling** mechanisms, such as problems with the **sarcoplasmic reticulum** or **calcium channels**, which are internal to the cardiomyocyte.
- It is distinct from the role of **intercalated discs** in facilitating intercellular communication and electrical spread.
*Inappropriate formation of cardiac valve leaflets*
- The formation of cardiac valve leaflets is an intricate process during **embryological development** involving specific signaling pathways and cell migration.
- This structural defect is not directly related to the function of **intercalated discs** in mature cardiac muscle, which are involved in electrical and mechanical coupling.
*Outflow tract obstruction*
- **Outflow tract obstruction** is a congenital or acquired structural defect affecting the major arteries leaving the heart (e.g., aortic or pulmonary stenosis).
- This is a macroscopic structural anomaly that is not caused by a primary failure of **intercalated disc** function.
Common arrhythmia recognition US Medical PG Question 10: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Common arrhythmia recognition Explanation: ***Glossopharyngeal***
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
More Common arrhythmia recognition US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.