ECG interpretation

On this page
🔍 The ECG Detective: Mastering Cardiac Electrical Mysteries
You'll learn to decode the heart's electrical language by mastering systematic ECG interpretation-from identifying rhythms and analyzing waveform morphology to measuring critical intervals, determining axis deviation, and recognizing ischemic patterns. This skill transforms squiggly lines into life-saving diagnoses, enabling you to detect arrhythmias, conduction blocks, and silent myocardial infarctions before they become catastrophic. We'll build your interpretation framework step-by-step, turning uncertainty into clinical confidence at the bedside.
📌 Remember: PQRST - Patrial depolarization, QRS ventricular depolarization, Repolarization (ST-T), Segments (isoelectric), Timing (intervals)
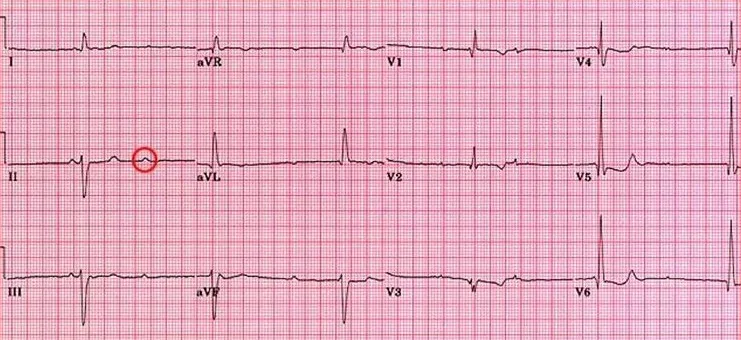
The systematic approach to ECG interpretation follows a structured hierarchy that prevents diagnostic errors. Rate analysis establishes the foundation - normal sinus rhythm maintains 60-100 bpm, while bradycardia <60 bpm and tachycardia >100 bpm trigger specific evaluation protocols. Rhythm assessment follows, distinguishing regular from irregular patterns with >10% variation defining irregularity.
- Primary ECG Components
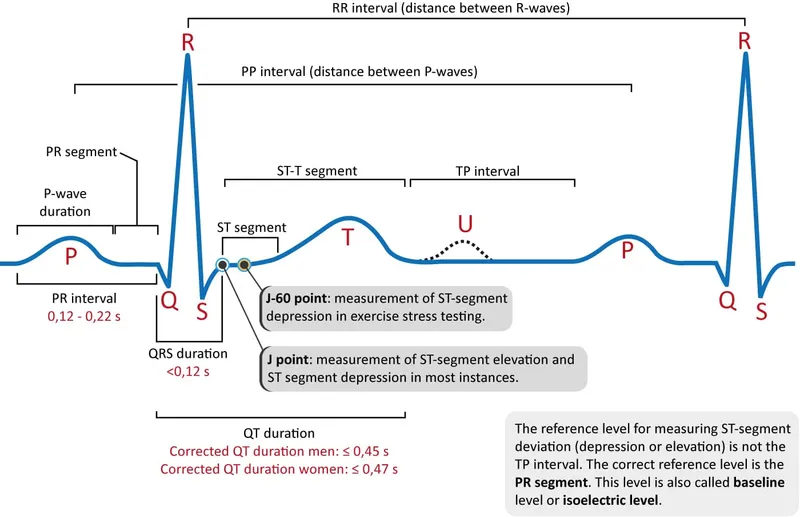
- P Wave: Atrial depolarization (<120ms duration, <2.5mm height)
- PR Interval: AV conduction time (120-200ms normal range)
- QRS Complex: Ventricular depolarization (<100ms width)
- Q waves: Initial negative deflection (<25% R wave height)
- R waves: Positive deflection (varies by lead)
- S waves: Negative deflection after R wave
- ST Segment: Early repolarization (isoelectric baseline)
- T Wave: Ventricular repolarization (upright in I, II, V3-V6)
⭐ Clinical Pearl: Lead II provides the clearest P wave morphology in 85% of patients, making it the gold standard for rhythm analysis and AV block assessment.
| Lead Group | Anatomical Territory | Primary Vessels | Normal R Wave Progression | Key Abnormalities |
|---|---|---|---|---|
| Inferior (II, III, aVF) | Inferior wall | RCA (85%), LCX (15%) | R wave ≥ S wave in III | Q waves >40ms |
| Lateral (I, aVL, V5-V6) | Lateral wall | LCX, LAD diagonal | R/S ratio >1 in V6 | Poor R progression |
| Anterior (V1-V4) | Anterior wall | LAD | R>S transition V3-V4 | Loss of R waves |
| Septal (V1-V2) | Interventricular septum | LAD septal perforators | Small R in V1 | Deep Q waves |
| Posterior | Posterior wall | RCA, LCX | Tall R in V1-V2 | R/S ratio >1 in V1 |
💡 Master This: Rate calculation mastery - Count R-R intervals in 6-second strips and multiply by 10, or use the 300/large squares method for regular rhythms. Irregular rhythms require full 10-second analysis for accuracy.
Understanding lead placement geometry transforms ECG interpretation from memorization to logical deduction. The frontal plane leads (I, II, III, aVR, aVL, aVF) view cardiac electrical activity from six different angles, while precordial leads (V1-V6) provide horizontal plane visualization from right ventricle to lateral wall.
⚠️ Warning: Lead misplacement occurs in 4% of routine ECGs, with limb lead reversal creating pseudo-infarction patterns that can trigger unnecessary interventions.
Connect these foundational principles through systematic waveform analysis to understand how electrical timing predicts mechanical function and clinical outcomes.
🔍 The ECG Detective: Mastering Cardiac Electrical Mysteries
⚡ Rhythm Recognition: The Cardiac Conductor's Score
Sinus rhythm analysis establishes the diagnostic foundation through systematic evaluation of P wave morphology and timing relationships. Normal sinus rhythm demonstrates upright P waves in leads I, II, aVF with consistent PR intervals of 120-200ms. P wave axis between 0-75 degrees confirms sinus node origin, while axis deviation >75 degrees suggests ectopic atrial pacemakers.
📌 Remember: ARREST - Atrial activity, Rate calculation, Regularity assessment, Ectopic beats, ST changes, Timing intervals
Atrial fibrillation recognition depends on identifying irregularly irregular rhythm patterns with absent P waves and fibrillatory waves at 350-600 bpm. The ventricular response typically ranges 100-180 bpm in untreated patients, while controlled AF maintains rates <100 bpm with rate-controlling medications.
- Atrial Arrhythmia Characteristics
- Atrial Fibrillation: Irregularly irregular, no P waves, f-waves 350-600/min
- Atrial Flutter: Regular sawtooth pattern, 300 bpm atrial rate, 2:1 or 4:1 block
- Type I: Counterclockwise, negative flutter waves in II, III, aVF
- Type II: Clockwise, positive flutter waves in inferior leads
- Multifocal Atrial Tachycardia: ≥3 P wave morphologies, rate >100 bpm
- Associated with COPD in 60% of cases
- Irregular P-P intervals with varying PR intervals

⭐ Clinical Pearl: Atrial flutter with 2:1 conduction produces ventricular rates of 150 bpm - a pathognomonic finding that should trigger immediate flutter wave analysis in leads II, III, and aVF.
Ventricular arrhythmia recognition requires distinguishing wide QRS tachycardias through morphology analysis and AV dissociation assessment. Ventricular tachycardia demonstrates QRS width >120ms, rate 150-250 bpm, and AV dissociation in 75% of cases. Capture beats and fusion beats provide pathognomonic evidence of VT when present.
| Arrhythmia Type | Rate Range | QRS Width | Key Features | Clinical Significance |
|---|---|---|---|---|
| Sinus Tachycardia | 100-180 bpm | <100ms | Gradual onset/offset | Physiologic response |
| SVT (AVNRT) | 150-250 bpm | <100ms | Abrupt onset/offset | Pseudo-R' in V1 |
| Atrial Flutter | 150 bpm (2:1) | <100ms | Sawtooth pattern | 300 bpm atrial rate |
| Ventricular Tachycardia | 150-250 bpm | >120ms | AV dissociation | Hemodynamic compromise |
| Torsades de Pointes | 200-300 bpm | >120ms | Twisting morphology | Long QT syndrome |
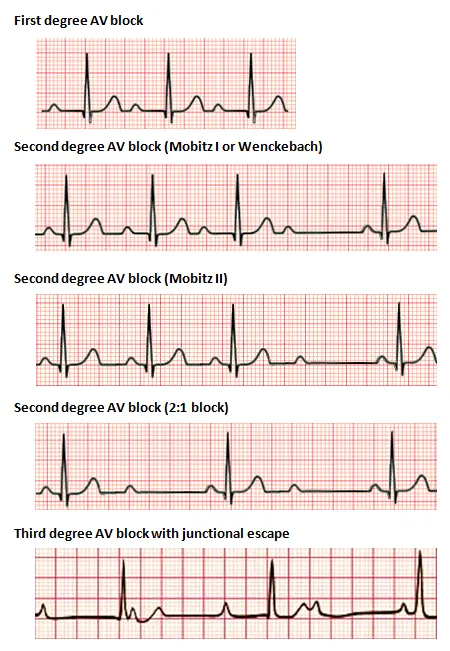
Bradyarrhythmia analysis focuses on conduction block patterns and escape rhythm identification. First-degree AV block shows PR prolongation >200ms with 1:1 conduction maintained. Second-degree blocks demonstrate intermittent conduction failure - Mobitz I with progressive PR prolongation, Mobitz II with fixed PR intervals and sudden conduction loss.
⚠️ Warning: Mobitz II second-degree AV block carries high risk of progression to complete heart block, requiring immediate pacemaker evaluation in symptomatic patients.
Connect rhythm recognition mastery through systematic waveform morphology analysis to understand how specific patterns predict hemodynamic consequences and guide therapeutic interventions.
⚡ Rhythm Recognition: The Cardiac Conductor's Score
📐 Waveform Morphology: Decoding Electrical Architecture
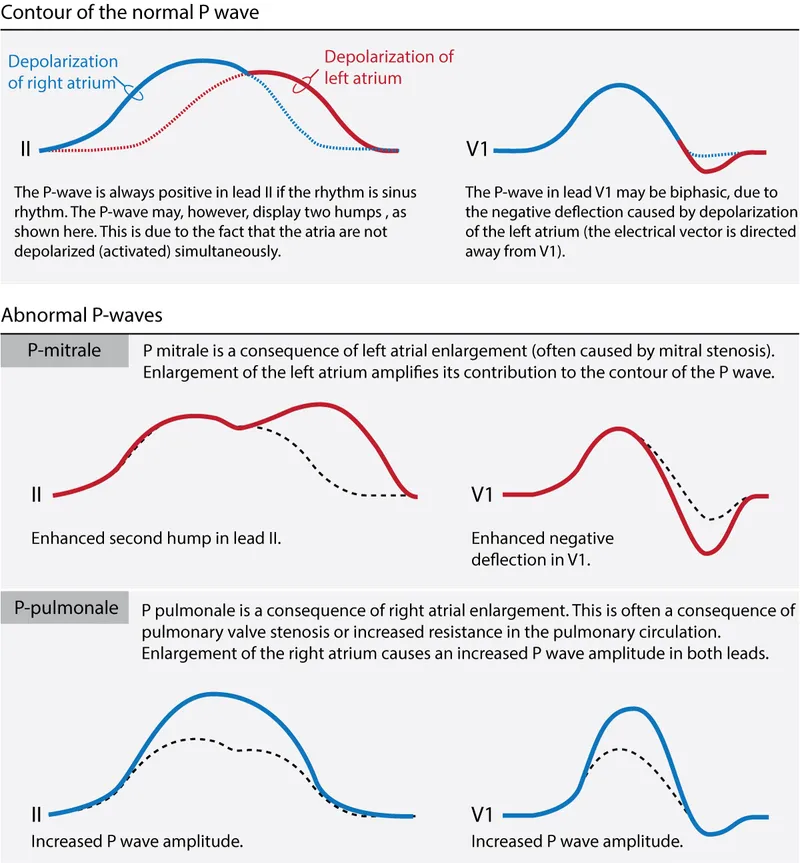
P wave morphology analysis provides crucial insights into atrial pathology and conduction disorders. Normal P waves demonstrate duration <120ms and amplitude <2.5mm in limb leads, with biphasic morphology in V1 reflecting sequential atrial activation. Right atrial enlargement produces tall, peaked P waves >2.5mm in leads II, III, aVF, while left atrial enlargement creates broad, notched P waves with terminal negative component in V1.
📌 Remember: MACHO - Mitral (LAE = notched), Amplitude (RAE = tall), Chronology (duration), Height (voltage), Orientation (axis)
- P Wave Abnormality Patterns
- Right Atrial Enlargement (P pulmonale)
- Height >2.5mm in leads II, III, aVF
- Peaked, symmetric morphology
- Associated with pulmonary hypertension in 70% of cases
- Left Atrial Enlargement (P mitrale)
- Duration >120ms with notched appearance
- Terminal negative component in V1 >40ms
- P wave area in V1 negative component >1 small square
- Biatrial Enlargement
- Tall AND broad P waves meeting both criteria
- Biphasic P in V1 with prominent positive and negative components
- Right Atrial Enlargement (P pulmonale)
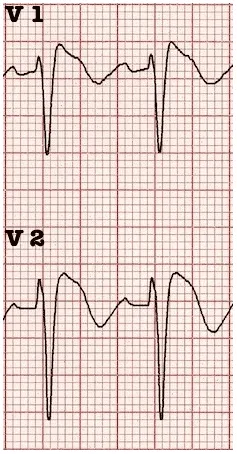
QRS complex analysis reveals ventricular pathology through systematic evaluation of width, amplitude, and morphological patterns. Normal QRS duration <100ms indicates intact intraventricular conduction, while prolongation >120ms suggests bundle branch blocks or ventricular hypertrophy. QRS amplitude varies significantly by lead position and patient factors.
⭐ Clinical Pearl: QRS width >120ms with LBBB morphology indicates significant left ventricular dysfunction in 85% of cases, often requiring echocardiographic evaluation and heart failure management.
Bundle branch block recognition depends on identifying specific morphological patterns in key leads. Right bundle branch block demonstrates RSR' pattern in V1 with wide S waves in leads I and V6. Left bundle branch block shows broad, notched R waves in I, aVL, V5-V6 with QS or rS pattern in V1.
| Block Type | V1 Morphology | I/aVL/V6 Pattern | QRS Width | Clinical Associations |
|---|---|---|---|---|
| RBBB | RSR', rSR' | Wide S waves | >120ms | RV strain, PE |
| LBBB | QS, rS | Broad, notched R | >120ms | LV dysfunction |
| LAFB | Normal | qR pattern | <120ms | Left axis deviation |
| LPFB | Normal | rS pattern | <120ms | Right axis deviation |
| Bifascicular | RBBB + fascicular | Combined patterns | >120ms | High-grade block risk |
💡 Master This: Wellens' syndrome shows biphasic or deeply inverted T waves in V2-V3 indicating critical LAD stenosis requiring urgent catheterization - present in 14-18% of unstable angina cases.
ST segment evaluation provides critical information about myocardial injury and ischemia. Normal ST segments remain isoelectric with <1mm deviation from baseline. ST elevation >1mm in ≥2 contiguous leads indicates acute injury, while ST depression >0.5mm suggests ischemia or reciprocal changes.
- ST Segment Abnormality Patterns
- ST Elevation (Injury Pattern)
- >1mm elevation in limb leads
- >2mm elevation in precordial leads
- Convex upward morphology indicates acute MI
- ST Depression (Ischemia Pattern)
- Horizontal or downsloping >0.5mm
- Upsloping depression >1.5mm at J-point
- Reciprocal changes in opposite leads
- ST Segment Mimics
- Early repolarization: J-point elevation with upward concavity
- Pericarditis: Diffuse elevation with PR depression
- ST Elevation (Injury Pattern)
⚠️ Warning: Posterior MI presents as tall R waves in V1-V2 with ST depression - easily missed without posterior lead assessment (V7-V9).
Connect morphological pattern recognition through systematic interval measurement to understand how timing abnormalities predict conduction disorders and arrhythmic risks.
📐 Waveform Morphology: Decoding Electrical Architecture
⏱️ Interval Analysis: Timing the Cardiac Symphony

PR interval assessment evaluates atrioventricular conduction through systematic measurement from P wave onset to QRS beginning. Normal PR intervals range 120-200ms, with age-related variations - children 120-160ms, adults 120-200ms, elderly up to 220ms. PR prolongation >200ms indicates first-degree AV block, while PR shortening <120ms suggests preexcitation syndromes.
📌 Remember: PACED - PR interval (120-200ms), AV blocks (1°, 2°, 3°), Conduction delays, Escape rhythms, Delta waves (WPW)
- PR Interval Abnormality Classification
- First-Degree AV Block
- PR >200ms with 1:1 conduction maintained
- Progressive lengthening may indicate developing higher-grade block
- Associated with digitalis toxicity in 15% of cases
- Short PR Syndrome
- PR <120ms with normal QRS morphology
- Lown-Ganong-Levine syndrome - enhanced AV conduction
- Preexcitation variants without delta waves
- Variable PR Intervals
- Mobitz I (Wenckebach) - progressive lengthening then dropped beat
- Mobitz II - fixed PR with sudden conduction failure
- First-Degree AV Block
QRS duration analysis reveals intraventricular conduction status and ventricular activation patterns. Normal QRS width <100ms indicates intact His-Purkinje conduction, while prolongation 100-120ms suggests incomplete blocks or ventricular hypertrophy. QRS >120ms defines complete bundle branch blocks requiring morphological analysis.
⭐ Clinical Pearl: QRS widening >130ms in LBBB indicates severe left ventricular dysfunction and potential CRT candidacy - present in cardiac resynchronization therapy evaluation protocols.
QT interval measurement assesses ventricular repolarization duration and arrhythmic risk. QT interval extends from QRS onset to T wave end, requiring rate correction using Bazett's formula: QTc = QT/√RR. Normal QTc values are <440ms in men and <460ms in women, with prolongation indicating increased torsades risk.
| QT Parameter | Normal Range | Borderline | Prolonged | Clinical Risk |
|---|---|---|---|---|
| QTc (Men) | <440ms | 440-470ms | >470ms | Torsades risk >500ms |
| QTc (Women) | <460ms | 460-480ms | >480ms | 2x higher baseline |
| QT Dispersion | <50ms | 50-80ms | >80ms | Sudden death risk |
| T-peak to T-end | <100ms | 100-120ms | >120ms | Arrhythmic substrate |
💡 Master This: QTc >500ms increases torsades risk 5-fold, requiring immediate medication review and electrolyte correction - hypokalemia <3.5mEq/L and hypomagnesemia <1.8mg/dL are correctable triggers.
RR interval variability provides insights into autonomic function and arrhythmic patterns. Heart rate variability analysis reveals parasympathetic and sympathetic balance, with reduced variability indicating increased mortality risk in post-MI patients. RR interval irregularity >10% defines irregular rhythms requiring rhythm-specific evaluation.
- RR Interval Pattern Analysis
- Regular Rhythms
- RR variation <10% indicates consistent conduction
- Sinus arrhythmia shows respiratory variation in young patients
- Fixed RR intervals suggest electronic pacing
- Irregular Patterns
- Irregularly irregular - atrial fibrillation pattern
- Regularly irregular - second-degree AV block patterns
- Occasionally irregular - premature beats or escape rhythms
- Regular Rhythms
⚠️ Warning: Sudden RR interval changes >20% during continuous monitoring may indicate developing AV block or ischemic conduction changes requiring immediate evaluation.
Rate-dependent interval changes reveal dynamic conduction properties and autonomic influences. PR interval shortening with increased heart rate reflects enhanced AV conduction, while QT interval shortening maintains constant repolarization time. Aberrant conduction occurs when cycle length changes exceed refractory period recovery.
Connect interval timing mastery through systematic axis determination to understand how electrical vector changes predict anatomical and pathological cardiac alterations.
⏱️ Interval Analysis: Timing the Cardiac Symphony
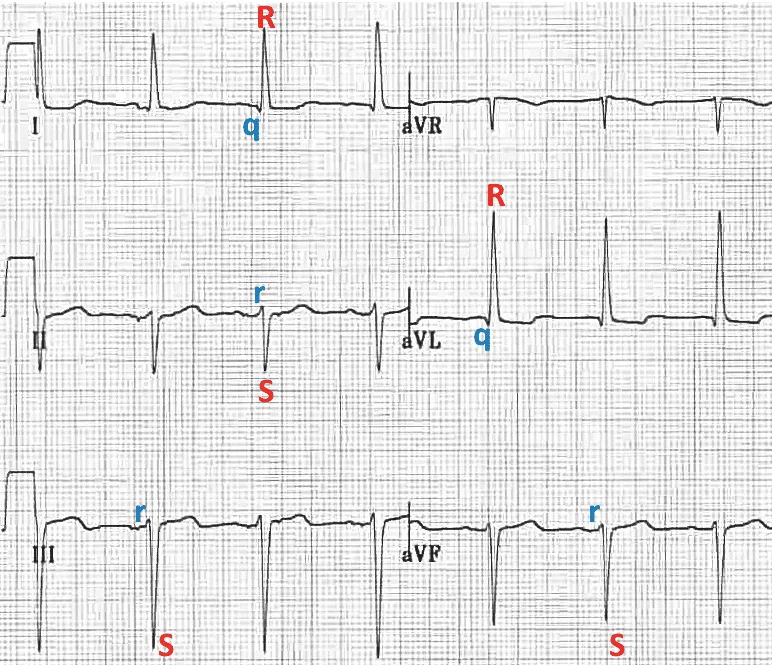
🧭 Axis Determination: The Heart's Electrical Compass
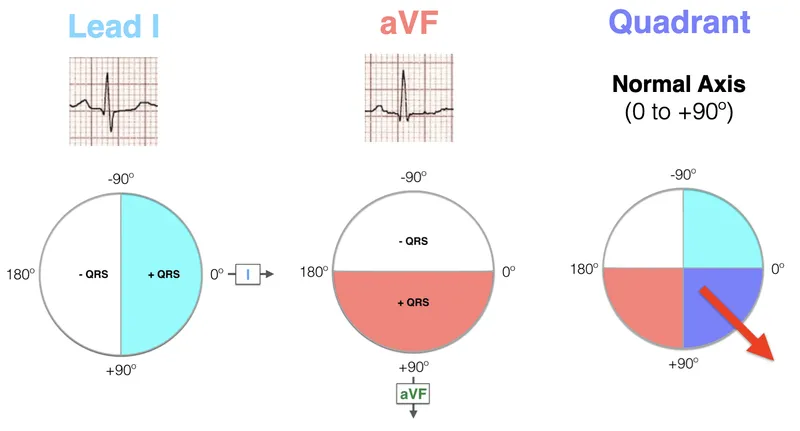
Normal cardiac axis ranges from -30° to +90°, reflecting normal left ventricular dominance and physiological conduction patterns. Left axis deviation (LAD) occurs with axis <-30°, while right axis deviation (RAD) presents with axis >+90°. Extreme axis deviation beyond ±120° indicates significant pathology requiring immediate evaluation.
📌 Remember: LEAD - Left axis deviation (<-30°), Extreme deviation (±120°), Axis normal (-30° to +90°), Dextrocardia (negative in I)
Quadrant method provides rapid axis estimation using leads I and aVF as perpendicular references. Positive deflections in both leads indicate normal axis (0° to +90°), while specific combinations identify axis quadrants with high accuracy. This two-lead approach enables bedside axis determination within 30-degree ranges.
- Axis Deviation Clinical Correlations
- Left Axis Deviation (-30° to -90°)
- Left anterior fascicular block - most common cause
- Left ventricular hypertrophy with conduction delay
- Inferior myocardial infarction with Q waves
- Mechanical shifts - pregnancy, obesity, ascites
- Right Axis Deviation (+90° to +180°)
- Right ventricular hypertrophy - pulmonary disease
- Left posterior fascicular block - rare isolated finding
- Lateral myocardial infarction with conduction loss
- Pulmonary embolism - acute RV strain
- Left Axis Deviation (-30° to -90°)
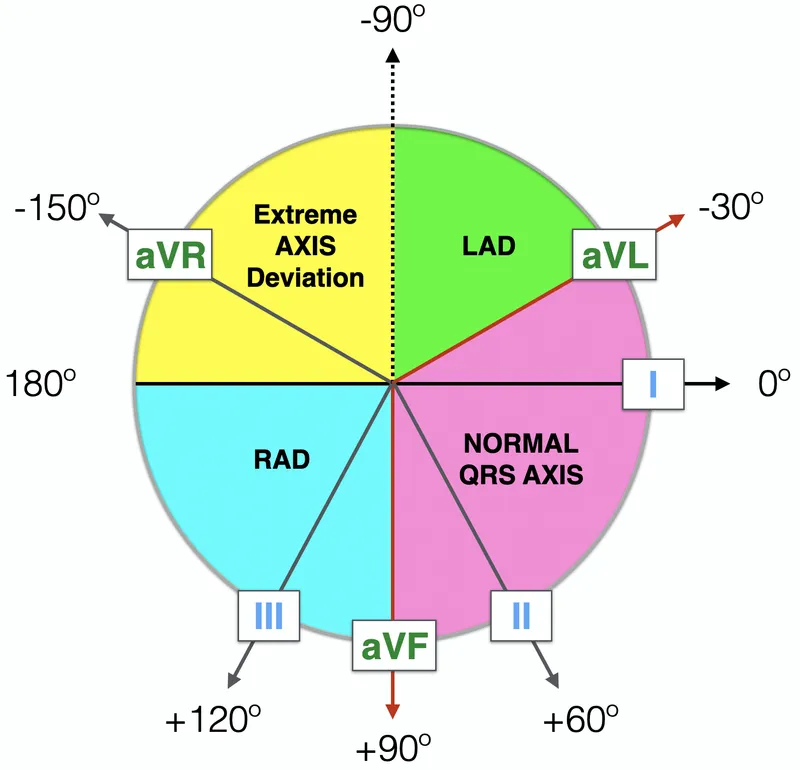
Isoelectric lead method provides precise axis calculation by identifying the lead with equal positive and negative deflections. The cardiac axis lies perpendicular to the isoelectric lead, enabling exact degree measurement using the hexaxial reference system. This method achieves ±15-degree accuracy for detailed axis analysis.
⭐ Clinical Pearl: Lead aVR positivity indicates extreme axis deviation or lead misplacement - normally shows negative QRS deflection in >95% of patients with normal cardiac position.
Age-related axis variations reflect developmental cardiac changes and physiological adaptations. Newborns demonstrate right axis deviation (+90° to +180°) due to right ventricular dominance, gradually shifting leftward to adult patterns by age 8-16 years. Elderly patients may show progressive leftward shift with conduction system aging.
| Age Group | Normal Axis Range | Common Deviations | Clinical Significance |
|---|---|---|---|
| Newborn | +90° to +180° | RVH physiologic | Normal RV dominance |
| Child (1-8y) | +30° to +120° | Gradual leftward shift | LV growth pattern |
| Adult | -30° to +90° | LAD with age | Conduction changes |
| Elderly (>65y) | -30° to +75° | Progressive LAD | Fibrosis effects |
💡 Master This: Bifascicular block (RBBB + LAFB or LPFB) carries 10-15% risk of progression to complete heart block, requiring pacemaker consideration in symptomatic patients with syncope or presyncope.
Axis shifts during acute events provide dynamic diagnostic information about evolving cardiac pathology. Acute right heart strain from pulmonary embolism causes sudden RAD with S1Q3T3 pattern, while acute inferior MI may produce LAD through conduction system involvement. Serial axis monitoring reveals progression or resolution of underlying conditions.
- Dynamic Axis Change Patterns
- Acute Pulmonary Embolism
- Sudden RAD development with S1Q3T3 pattern
- Right heart strain pattern in V1-V3
- Axis shift >30° from baseline in massive PE
- Acute Myocardial Infarction
- Inferior MI - LAD development with fascicular involvement
- Lateral MI - RAD with lateral conduction loss
- Anterior MI - axis preservation unless extensive
- Acute Pulmonary Embolism
⚠️ Warning: Extreme axis deviation with QRS widening suggests severe conduction disease or ventricular arrhythmia - requires immediate rhythm analysis and hemodynamic assessment.
Connect axis determination expertise through comprehensive ischemia pattern recognition to understand how electrical vector changes predict coronary territories and guide therapeutic interventions.
🧭 Axis Determination: The Heart's Electrical Compass
🚨 Ischemia Recognition: The Silent Cardiac Alarm
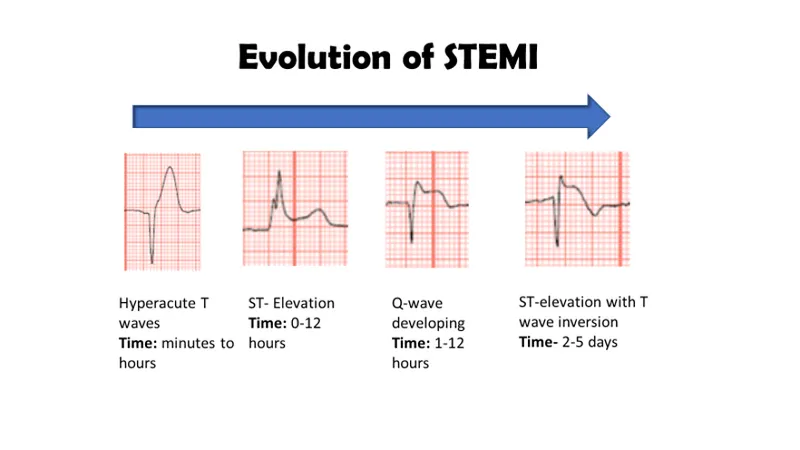
STEMI recognition requires identifying ST elevation ≥1mm in ≥2 contiguous leads with appropriate clinical context. Anterior STEMI affects leads V1-V6 with LAD territory involvement, while inferior STEMI presents in leads II, III, aVF indicating RCA occlusion in 85% of cases. Time to reperfusion <90 minutes reduces mortality by 25% compared to delayed intervention.
📌 Remember: STEMI - ST elevation ≥1mm, Two contiguous leads, Emergent reperfusion, Myocardial territory, Immediate catheterization
Hyperacute T wave recognition identifies earliest ischemic changes preceding ST elevation by 15-30 minutes. These tall, peaked, symmetric T waves appear disproportionately large relative to QRS amplitude and indicate acute coronary occlusion requiring immediate intervention. Hyperacute changes occur in 60-80% of acute occlusions before classic ST elevation.
- Coronary Territory Localization
- Anterior Wall (LAD Territory)
- V1-V6 - Extensive anterior with septal and lateral involvement
- V2-V4 - Anterior wall isolated
- V1-V2 - Septal involvement with septal perforator occlusion
- Inferior Wall (RCA Territory 85%)
- II, III, aVF - Inferior wall with RCA or dominant LCX
- Reciprocal depression in aVL confirms inferior injury
- V7-V9 - Posterior extension assessment
- Lateral Wall (LCX Territory)
- I, aVL, V5-V6 - Lateral wall circumflex distribution
- High lateral - I, aVL isolated
- Low lateral - V5-V6 predominant
- Anterior Wall (LAD Territory)

NSTEMI and unstable angina present with ST depression, T wave inversion, or dynamic changes without persistent ST elevation. Horizontal or downsloping ST depression ≥0.5mm indicates significant ischemia, while upsloping depression ≥1.5mm at J-point +80ms suggests ischemic burden. Troponin elevation distinguishes NSTEMI from unstable angina.
⭐ Clinical Pearl: Wellens' syndrome shows biphasic or deeply inverted T waves in V2-V3 indicating critical LAD stenosis - present in 14-18% of unstable angina cases requiring urgent catheterization.
Posterior MI recognition challenges traditional 12-lead analysis since posterior wall lacks direct lead representation. Tall R waves in V1-V2 with R/S ratio >1 suggest posterior injury, while ST depression in V1-V3 represents reciprocal changes. Posterior leads V7-V9 confirm diagnosis with ST elevation ≥0.5mm.
| MI Location | Primary Leads | Reciprocal Changes | Culprit Vessel | Key Features |
|---|---|---|---|---|
| Anterior | V2-V4 | II, III, aVF | LAD | Q waves V2-V4 |
| Extensive Anterior | V1-V6, I, aVL | II, III, aVF | Proximal LAD | Poor R progression |
| Inferior | II, III, aVF | I, aVL | RCA (85%) | Q waves inferior |
| Posterior | V7-V9 | V1-V3 | RCA/LCX | Tall R in V1-V2 |
| Lateral | I, aVL, V5-V6 | III, aVF | LCX | Q waves lateral |
💡 Master This: ST elevation resolution >50% within 60-90 minutes of reperfusion indicates successful recanalization - persistent ST elevation suggests failed reperfusion requiring rescue intervention.
Ischemic mimics create diagnostic challenges requiring systematic differentiation. Early repolarization shows J-point elevation with upward concavity and notching, while pericarditis demonstrates diffuse ST elevation with PR depression. Left ventricular aneurysm produces persistent ST elevation in chronic infarct territories.
- ST Elevation Differential Diagnosis
- Early Repolarization
- J-point elevation with upward concavity
- Notching or slurring at QRS-ST junction
- Stable pattern without evolutionary changes
- Pericarditis
- Diffuse ST elevation in multiple territories
- PR depression in limb leads
- Spodick's sign - downsloping TP segment
- Left Ventricular Aneurysm
- Persistent ST elevation in old infarct territory
- Q waves with poor R wave progression
- No acute symptoms or troponin elevation
- Early Repolarization
⚠️ Warning: Posterior MI accounts for 15-20% of inferior MIs but lacks representation in standard 12-lead ECGs - always obtain V7-V9 in inferior STEMI patients.
Connect ischemia recognition mastery through advanced integration concepts to understand how electrical changes predict mechanical dysfunction and guide comprehensive cardiac care strategies.
🚨 Ischemia Recognition: The Silent Cardiac Alarm
🎯 ECG Mastery Arsenal: Your Clinical Command Center
Rapid ECG interpretation protocol follows the systematic RAMI approach: Rate, Axis, Morphology, Intervals. This standardized sequence prevents diagnostic errors and ensures comprehensive evaluation within 60-90 seconds. Expert interpreters achieve 95% diagnostic accuracy using structured protocols versus 78% accuracy with random approaches.
📌 Remember: RAMI-ST - Rate (60-100), Axis (-30° to +90°), Morphology (P-QRS-T), Intervals (PR, QRS, QT), ST segments, T waves
- Essential ECG Arsenal - Critical Values
- Rate Thresholds
- Bradycardia <60 bpm - symptomatic <50 bpm
- Tachycardia >100 bpm - hemodynamic compromise >150 bpm
- Ventricular rates >250 bpm - VT/VF territory
- Interval Boundaries
- PR: 120-200ms - 1st degree block >200ms
- QRS: <100ms normal - BBB >120ms
- QTc: <440ms (M), <460ms (F) - torsades risk >500ms
- Axis Landmarks
- Normal: -30° to +90° - LAD <-30°, RAD >+90°
- Extreme deviation: ±120° - pathological significance
- Rate Thresholds
| Clinical Scenario | Key ECG Findings | Immediate Actions | Time Targets |
|---|---|---|---|
| STEMI | ST elevation ≥1mm, ≥2 leads | Activate cath lab | Door-to-balloon <90min |
| Complete Heart Block | AV dissociation, escape <40 | Transcutaneous pacing | Pacemaker <24hrs |
| Atrial Fibrillation RVR | Irregular, rate >150 | Rate control, anticoagulation | Rate <100 in 24hrs |
| Torsades de Pointes | Polymorphic VT, long QT | Magnesium 2g IV | Immediate cardioversion |
| Hyperkalemia | Peaked T, wide QRS | Calcium, insulin/glucose | K+ <5.5 in 1hr |
Pattern recognition drills accelerate diagnostic expertise through systematic exposure to high-yield scenarios. Bundle branch blocks appear in 15% of hospitalized patients, while atrial fibrillation affects 33% of patients >80 years. Mastering common patterns enables rapid triage and appropriate interventions.
💡 Master This: Serial ECG comparison reveals dynamic changes - new Q waves, evolving ST segments, and T wave inversions indicate active processes requiring immediate intervention versus chronic findings.
High-yield diagnostic combinations predict specific pathologies with high accuracy. S1Q3T3 pattern suggests pulmonary embolism in appropriate clinical context, while electrical alternans indicates pericardial tamponade. Osborn waves (J waves) appear in hypothermia <32°C and hypercalcemia.
- Pathognomonic ECG Patterns
- Brugada Syndrome
- Type 1: Coved ST elevation ≥2mm in V1-V2
- Type 2: Saddleback pattern with ST elevation ≥1mm
- Sudden death risk - ICD consideration
- Arrhythmogenic RV Cardiomyopathy
- Epsilon waves in V1-V3
- T wave inversion V1-V3 beyond age 14
- QRS prolongation >110ms in V1-V3
- Hypertrophic Cardiomyopathy
- Deep Q waves in lateral leads
- Giant T wave inversion in apical variant
- Left ventricular hypertrophy with strain
- Brugada Syndrome
⚠️ Warning: New LBBB in acute chest pain carries equivalent risk to STEMI - activate catheterization laboratory for emergent revascularization within 90 minutes.
Quality assurance protocols ensure diagnostic accuracy through systematic verification. Lead placement confirmation, artifact recognition, and technical quality assessment prevent misinterpretation. Computer interpretation achieves 85% accuracy but requires physician overread for clinical correlation.
Connect this comprehensive ECG mastery framework to advanced cardiac care protocols, enabling rapid diagnosis, appropriate triage, and optimal therapeutic interventions across the full spectrum of cardiovascular emergencies and chronic conditions.
🎯 ECG Mastery Arsenal: Your Clinical Command Center
Practice Questions: ECG interpretation
Test your understanding with these related questions
An ECG from an 8-year-old male with neurosensory deafness and a family history of sudden cardiac arrest demonstrates QT-interval prolongation. Which of the following is this patient most at risk of developing?













