Surfactant function and synthesis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surfactant function and synthesis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surfactant function and synthesis US Medical PG Question 1: During a clinical study examining the diffusion of gas between the alveolar compartment and the pulmonary capillary blood, men between the ages of 20 and 50 years are evaluated while they hold a sitting position. After inhaling a water-soluble gas that rapidly combines with hemoglobin, the concentration of the gas in the participant's exhaled air is measured and the diffusion capacity is calculated. Assuming that the concentration of the inhaled gas remains the same, which of the following is most likely to increase the flow of the gas across the alveolar membrane?
- A. Deep exhalation
- B. Entering a cold chamber
- C. Treadmill exercise (Correct Answer)
- D. Standing straight
- E. Assuming a hunched position
Surfactant function and synthesis Explanation: ***Correct: Treadmill exercise***
- **Treadmill exercise** increases cardiac output and pulmonary blood flow, which in turn recruits and distends more **pulmonary capillaries**. This increases the **surface area** available for gas exchange and reduces the diffusion distance, thereby enhancing the flow of gas across the alveolar membrane.
- Exercise also typically leads to deeper and more frequent breaths, increasing the **ventilation-perfusion matching** and overall efficiency of gas exchange.
- According to Fick's law of diffusion (Vgas = A/T × D × ΔP), increasing the surface area (A) directly increases gas flow.
*Incorrect: Deep exhalation*
- **Deep exhalation** would empty the lungs more completely, potentially leading to alveolar collapse in some regions and thus **decreasing the alveolar surface area** available for gas exchange.
- This would also reduce the **driving pressure** for gas diffusion by lowering the alveolar concentration of the inhaled gas.
*Incorrect: Entering a cold chamber*
- Exposure to a **cold chamber** can cause **bronchoconstriction** in some individuals, particularly those with reactive airways, which would increase airway resistance and potentially reduce alveolar ventilation.
- While metabolic rate may slightly increase in the cold, the primary effect on the lungs is unlikely to promote increased gas diffusion in a healthy individual.
*Incorrect: Standing straight*
- **Standing straight** is a normal physiological posture and does not significantly alter the **pulmonary capillary recruitment** or the alveolar surface area in a way that would dramatically increase gas flow compared to a seated position.
- There might be minor gravitational effects on blood flow distribution, but these are generally less impactful than dynamic changes like exercise.
*Incorrect: Assuming a hunched position*
- **Assuming a hunched position** can restrict chest wall expansion and diaphragm movement, leading to **reduced tidal volume** and overall alveolar ventilation.
- This posture, by reducing lung volumes and potentially compressing the lungs, would likely **decrease the effective surface area** for gas exchange and therefore reduce gas flow.
Surfactant function and synthesis US Medical PG Question 2: A 63-year-old man with alpha-1-antitrypsin deficiency is brought to the emergency department 1 hour after his daughter found him unresponsive. Despite appropriate care, the patient dies. At autopsy, examination of the lungs shows enlargement of the airspaces in the respiratory bronchioles and alveoli. Enzymatic activity of which of the following cells is the most likely cause of these findings?
- A. Alveolar macrophages (Correct Answer)
- B. Ciliated bronchiolar epithelial cells
- C. Elastic fibers in alveolar septa
- D. Type I pneumocytes
- E. Alveolar septal cells
Surfactant function and synthesis Explanation: ***Alveolar macrophages***
- In **alpha-1-antitrypsin deficiency**, alveolar macrophages (and neutrophils) release **elastase**, which is normally inhibited by alpha-1-antitrypsin.
- Unchecked elastase activity from alveolar macrophages leads to the **destruction of elastic fibers** in the alveolar walls, causing emphysema with characteristic **panacinar** distribution (worse in lower lobes).
- This results in enlargement of airspaces distal to terminal bronchioles.
*Ciliated bronchiolar epithelial cells*
- These cells are primarily involved in **mucociliary clearance** and do not produce proteolytic enzymes that degrade elastic tissue.
- Their dysfunction would lead to impaired mucus clearance and increased susceptibility to infections, but not emphysema.
*Elastic fibers in alveolar septa*
- Elastic fibers are **extracellular matrix components**, not cells.
- While their destruction is the pathological mechanism of emphysema, they do not have enzymatic activity.
*Type I pneumocytes*
- **Type I pneumocytes** form the structural lining of the alveoli and are primarily involved in gas exchange.
- They do not produce elastase or other proteolytic enzymes responsible for tissue destruction in emphysema.
*Alveolar septal cells*
- This term broadly refers to structural cells including Type I and Type II pneumocytes.
- While these cells may be damaged secondarily in emphysema, they do not produce the elastase responsible for elastic fiber destruction.
Surfactant function and synthesis US Medical PG Question 3: An investigator is studying the clearance of respiratory particles in healthy non-smokers. An aerosol containing radio-labeled particles that are small enough to reach the alveoli is administered to the subjects via a non-rebreather mask. A gamma scanner is then used to evaluate the rate of particle clearance from the lungs. The primary mechanism of particle clearance most likely involves which of the following cell types?
- A. Goblet cells
- B. Macrophages (Correct Answer)
- C. Club cells
- D. Type I pneumocytes
- E. Neutrophils
Surfactant function and synthesis Explanation: ***Macrophages***
- **Alveolar macrophages** are the primary phagocytic cells in the alveoli responsible for clearing inhaled particles that reach this deepest part of the lung.
- They engulf and digest foreign substances, including pathogens and inert particles, protecting the delicate alveolar structures.
*Goblet cells*
- **Goblet cells** are found in the larger airways (trachea, bronchi), where they produce mucus to trap inhaled particles.
- They are not present in the alveoli, so they cannot clear particles that have reached this region.
*Club cells*
- **Club cells** (formerly Clara cells) are located in the bronchioles and secrete components of the surfactant-like material, but they do not primarily function in particle clearance.
- While they have some protective roles, they are not the main phagocytic cells for alveolar particles.
*Type I pneumocytes*
- **Type I pneumocytes** are flattened, thin cells that form the majority of the alveolar surface and are primarily involved in gas exchange.
- They are not phagocytic and do not play a direct role in clearing inhaled particles.
*Neutrophils*
- **Neutrophils** are acute inflammatory cells primarily involved in combating bacterial infections.
- While they can migrate to the lungs during inflammation, they are not the primary, routine phagocytic cells for clearing inhaled particles in healthy individuals.
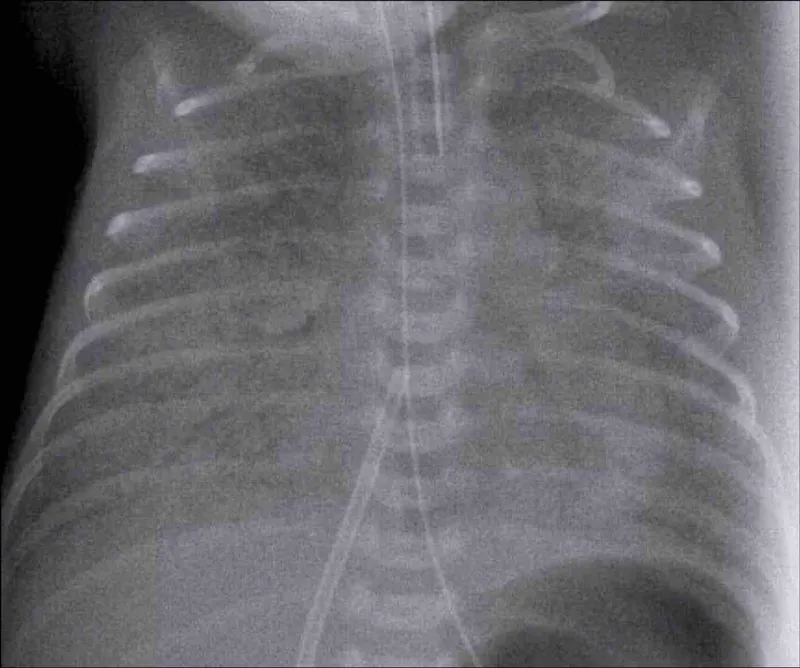
Surfactant function and synthesis US Medical PG Question 4: A baby is born after the 32nd gestational week by cesarean delivery. The mother suffered from gestational diabetes; however, she had no other pregnancy-related diseases and was otherwise healthy. The baby has a blood pressure of 100/58 mm Hg, heart rate of 104/min, and oxygen saturation of 88%. The child has tachypnea, subcostal and intercostal retractions, nasal flaring, and cyanosis. The cyanosis is responding well to initial administration of oxygen. The nasogastric tube was positioned without problems. Which of the following is the most likely diagnosis?
- A. Tracheoesophageal fistula
- B. Pneumonia
- C. Neonatal respiratory distress syndrome (NRDS) (Correct Answer)
- D. Sepsis
- E. Congenital heart anomaly with right-to-left shunt
Surfactant function and synthesis Explanation: ***Neonatal respiratory distress syndrome (NRDS)***
- The premature birth (32nd week), presence of **tachypnea**, **retractions**, **nasal flaring**, **cyanosis** responding to oxygen, and maternal **gestational diabetes** are all highly suggestive of NRDS.
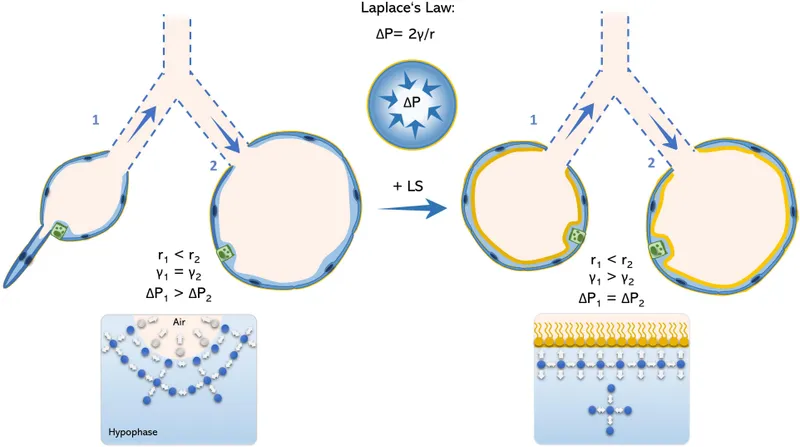
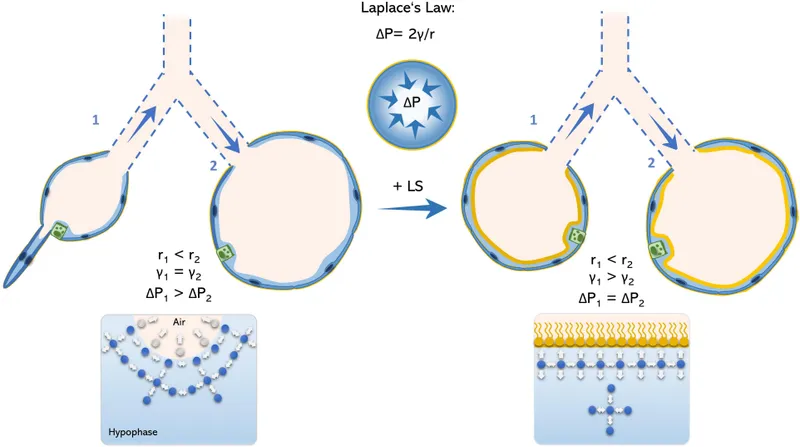
- Maternal gestational diabetes can delay fetal lung maturity, increasing the risk of **surfactant deficiency**, which is the primary cause of NRDS.
*Tracheoesophageal fistula*
- This condition typically presents with **choking**, **coughing**, and **regurgitation** during feeding, often with inability to pass a nasogastric tube into the stomach.
- The successful positioning of the **nasogastric tube** makes this diagnosis less likely.
*Pneumonia*
- While pneumonia can cause respiratory distress, the **early onset** in a premature infant with maternal gestational diabetes points more strongly towards **NRDS**.
- Pneumonia would typically have signs of **infection** such as fever, though early neonatal pneumonia can be atypical.
*Sepsis*
- Sepsis can cause respiratory distress, but it's usually accompanied by other signs of systemic infection, such as **fever or hypothermia**, **lethargy**, and poor feeding and often signs of **circulatory compromise**.
- The clinical picture provided primarily points towards a respiratory rather than a systemic infectious cause primarily.
*Congenital heart anomaly with right-to-left shunt*
- While this can cause **cyanosis** and respiratory distress, the prompt response to oxygen management makes a significant right-to-left shunt less likely.
- A significant right-to-left shunt would typically cause **cyanosis** that is refractory to oxygen administration.
Surfactant function and synthesis US Medical PG Question 5: A P2G1 diabetic woman is at risk of delivering at 29 weeks gestation. Her obstetrician counsels her that there is a risk the baby could have significant pulmonary distress after it is born. However, she states she will give the mother corticosteroids, which will help prevent this from occurring. Additionally, the obstetrician states she will perform a test on the amniotic fluid which will indicate the likelihood of the infant being affected by this syndrome. Which of the following ratios would be most predictive of the infant having pulmonary distress?
- A. lecithin:phosphatidylserine < 1.5
- B. lecithin:sphingomyelin < 1.5 (Correct Answer)
- C. lecithin:sphingomyelin > 1.5
- D. lecithin:phosphatidylserine > 3.0
- E. lecithin:sphingomyelin > 3.0
Surfactant function and synthesis Explanation: ***lecithin:sphingomyelin < 1.5***
- A lecithin:sphingomyelin (L:S) ratio less than 2:1 (or 1.5 in some clinical contexts) indicates **fetal lung immaturity** and a **high risk for respiratory distress syndrome (RDS)**.
- The **lecithin level increases** significantly in the amniotic fluid during the third trimester as fetal lungs mature, while **sphingomyelin levels remain relatively constant**.
*lecithin:phosphatidylserine < 1.5*
- While **phosphatidylserine** is a component of surfactant, the **Lecithin:Sphingomyelin (L:S) ratio** is the established and most commonly used marker for fetal lung maturity.
- There is **no widely recognized or clinically validated threshold** for a lecithin:phosphatidylserine ratio in predicting respiratory distress syndrome.
*lecithin:sphingomyelin > 1.5*
- An L:S ratio **greater than 2:1 (or 1.5, in some labs)** generally indicates **fetal lung maturity** and a low risk for respiratory distress syndrome.
- Therefore, this ratio would suggest a **lower likelihood of pulmonary distress**, which contradicts the aim of identifying risk.
*lecithin:phosphatidylserine > 3.0*
- As with an L:S ratio, a higher ratio would generally indicate **lung maturity**, not increased risk for pulmonary distress.
- There is **no clinical standard for lecithin:phosphatidylserine ratio** to assess lung maturity for preventing RDS.
*lecithin:sphingomyelin > 3.0*
- An L:S ratio of **greater than 2:1 (or 3.0 in certain clinical scenarios)** is a strong indicator of **fetal lung maturity**, meaning the risk of respiratory distress syndrome is low.
- The question asks for a ratio that would be **predictive of pulmonary distress**, whereas this ratio indicates the opposite.
Surfactant function and synthesis US Medical PG Question 6: A 55-year-old man with recurrent pneumonia comes to the physician for a follow-up examination one week after hospitalization for pneumonia. He feels well but still has a productive cough. He has smoked 1 pack of cigarettes daily for 5 years. His temperature is 36.9°C (98.4°F) and respirations are 20/min. Cardiopulmonary examination shows coarse crackles at the right lung base. Microscopic examination of a biopsy specimen of the right lower lung parenchyma shows proliferation of clustered, cuboidal, foamy-appearing cells. These cells are responsible for which of the following functions?
- A. Mucus secretion
- B. Cytokine release
- C. Lecithin production (Correct Answer)
- D. Toxin degradation
- E. Gas diffusion
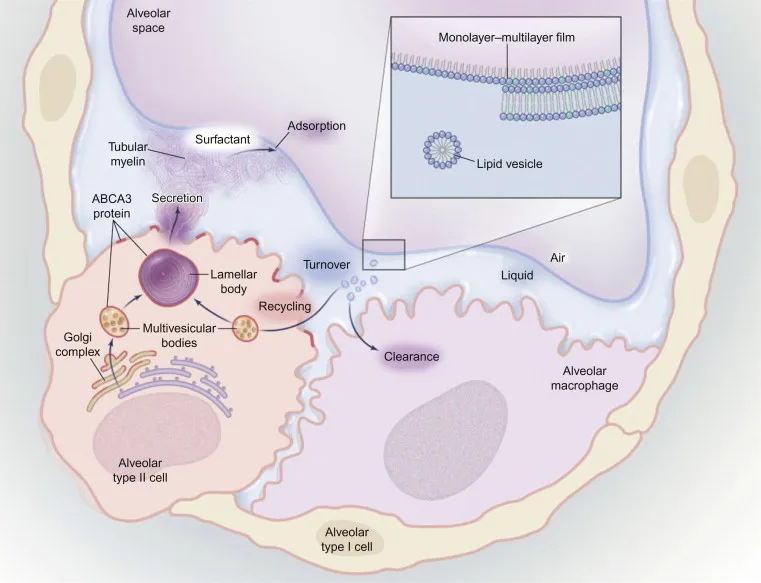
Surfactant function and synthesis Explanation: ***Lecithin production***
- The description of **clustered, cuboidal, foamy-appearing cells** in the lung parenchyma strongly suggests **Type II pneumocytes**.
- **Type II pneumocytes** are primarily responsible for producing and secreting **pulmonary surfactant**, which is rich in **lecithin (phosphatidylcholine)**, to reduce surface tension in the alveoli.
*Mucus secretion*
- **Goblet cells** and **submucosal glands** in the airways are responsible for mucus secretion, not the alveolar cells described.
- Mucus functions to trap particles and pathogens, preventing them from reaching the alveoli.
*Cytokine release*
- While various lung cells, including macrophages and epithelial cells, can release cytokines in response to inflammation or infection, it is not the primary defining function of Type II pneumocytes.
- **Cytokine release** is a broad immune response, not specific to the unique morphology and function described.
*Toxin degradation*
- The liver and kidneys are the primary organs for **toxin degradation** and excretion, though some detoxification can occur in the lungs.
- This function is not characteristic of **Type II pneumocytes**, which are focused on surfactant production and alveolar repair.
*Gas diffusion*
- **Gas diffusion** primarily occurs across the **Type I pneumocytes** (squamous alveolar cells) and the capillary endothelial cells due to their thinness and large surface area.
- **Type II pneumocytes** are thicker and less involved in direct gas exchange.
Surfactant function and synthesis US Medical PG Question 7: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
Surfactant function and synthesis Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Surfactant function and synthesis US Medical PG Question 8: A 68-year-old man with both severe COPD (emphysema) and newly diagnosed idiopathic pulmonary fibrosis presents with worsening dyspnea. His pressure-volume curve shows a complex pattern with features of both diseases. Static compliance measured at mid-lung volumes is 120 mL/cm H2O. His pulmonologist must decide on optimal management. Synthesizing the pathophysiology of both conditions, what represents the most significant clinical challenge in managing his combined disease?
- A. Pulmonary rehabilitation cannot address the opposing mechanical derangements
- B. The increased compliance from emphysema completely negates decreased compliance from fibrosis
- C. The opposing effects on compliance create a pseudonormal total respiratory compliance masking disease severity (Correct Answer)
- D. Emphysema treatment with bronchodilators will worsen fibrosis progression
- E. Oxygen therapy beneficial for COPD will accelerate fibrotic changes
Surfactant function and synthesis Explanation: ***The opposing effects on compliance create a pseudonormal total respiratory compliance masking disease severity***
- In **Combined Pulmonary Fibrosis and Emphysema (CPFE)**, the **increased lung compliance** from upper-lobe emphysema is offset by the **decreased compliance** from lower-lobe fibrosis.
- This results in a **pseudonormalization** of lung volumes (like FVC and TLC) and compliance measurements, which can lead to a significant **underestimation of disease severity** during clinical assessment.
*Pulmonary rehabilitation cannot address the opposing mechanical derangements*
- While mechanical derangements are complex, **pulmonary rehabilitation** remains a cornerstone of management to improve functional capacity and reduce dyspnea in both conditions.
- The challenge is not that rehabilitation is ineffective, but rather the **physiological monitoring** and objective assessment of progress are hampered by masked lung volumes.
*The increased compliance from emphysema completely negates decreased compliance from fibrosis*
- The two forces do not perfectly negate each other; rather, they coexist to produce a **paradoxical physiological profile** where static measurements appear mid-range while gas exchange is severely impaired.
- Patients often exhibit a **disproportionate reduction in DLCO** (diffusion capacity) despite relatively preserved lung volumes, indicating the negation is only superficial and numerical.
*Emphysema treatment with bronchodilators will worsen fibrosis progression*
- There is no clinical evidence suggesting that **bronchodilators** (beta-agonists or anticholinergics) used for COPD/emphysema accelerate the **pathological scarring** seen in idiopathic pulmonary fibrosis.
- Bronchodilators primarily target **airway smooth muscle** and do not interfere with the fibroblastic pathways driving interstitial lung disease.
*Oxygen therapy beneficial for COPD will accelerate fibrotic changes*
- **Long-term oxygen therapy (LTOT)** is used to treat chronic hypoxemia in both COPD and fibrosis and does not cause or accelerate **lung remodeling** or fibrosis.
- While high concentrations of inspired oxygen (FiO2) can cause **oxidative stress**, the flow rates used for clinical management do not contribute to the progression of pulmonary fibrosis.
Surfactant function and synthesis US Medical PG Question 9: A 42-year-old woman with systemic sclerosis develops both pulmonary fibrosis and chest wall restriction from skin thickening. Her measured total respiratory system compliance is 30 mL/cm H2O. Testing with complete paralysis and positive pressure ventilation shows isolated lung compliance of 50 mL/cm H2O. She is being considered for immunosuppressive therapy versus supportive care. Evaluate which intervention would provide the greatest improvement in her respiratory mechanics.
- A. Supportive care only, as both components contribute equally and irreversibly
- B. Combined therapy targeting lung disease with chest wall mobilization (Correct Answer)
- C. Aggressive immunosuppression targeting both lung and skin disease
- D. Lung-directed therapy only, as it contributes more to total compliance reduction
- E. Chest wall-directed physical therapy, as it is the primary limiting factor
Surfactant function and synthesis Explanation: ***Combined therapy targeting lung disease with chest wall mobilization*** - The total respiratory compliance (Ct) is calculated using the formula **1/Ct = 1/Clung + 1/Cchest wall**; here, 1/30 = 1/50 + 1/Ccw, which calculates the **chest wall compliance** as 75 mL/cm H2O. - Both the lungs (50 mL/cm H2O) and chest wall (75 mL/cm H2O) are significantly below the **normal value of ~200 mL/cm H2O**, meaning both require intervention for meaningful improvement. *Supportive care only, as both components contribute equally and irreversibly* - While both contribute, they are not strictly equal (50 vs 75), and **systemic sclerosis**-associated lung/skin disease may respond to modern therapeutic interventions. - Labeling these as **irreversible** ignores potential benefits from immunosuppression in the active inflammatory stages of **interstitial lung disease**. *Aggressive immunosuppression targeting both lung and skin disease* - While immunosuppression addresses the underlying **pathophysiology**, it may not provide immediate mechanical relief for fixed **chest wall restriction**. - Effective management often requires adding **physical therapy** and mobilization to address the extrinsic mechanical constraint caused by **scleroderma skin thickening**. *Lung-directed therapy only, as it contributes more to total compliance reduction* - Although lung compliance (50) is lower than chest wall compliance (75), ignoring the **chest wall component** neglects a significant portion of the patient's **work of breathing**. - Solely treating the lung disease will not bypass the **extrinsic restriction** imposed by the tight skin and musculoskeletal changes. *Chest wall-directed physical therapy, as it is the primary limiting factor* - The calculations show that **lung compliance** is actually more severely reduced (50) than chest wall compliance (75). - Focusing only on the **chest wall** would leave the primary cause of the **restrictive ventilatory defect** (pulmonary fibrosis) unaddressed.
Surfactant function and synthesis US Medical PG Question 10: A 58-year-old man with end-stage pulmonary fibrosis is being evaluated for lung transplantation. His current static compliance is 25 mL/cm H2O (normal: 200 mL/cm H2O). He also has mild obesity (BMI 32) and ankylosing spondylitis affecting chest wall mobility. Post-transplant, assuming successful bilateral lung transplant with normal donor lungs, what would be the expected change in his total respiratory system compliance?
- A. Improved lung compliance but worsened chest wall compliance from surgery
- B. Worse compliance initially due to transplant rejection and denervation
- C. Return to completely normal respiratory compliance matching healthy individuals
- D. Improved but still reduced compliance due to persistent chest wall restriction (Correct Answer)
- E. No significant change because the primary problem is muscular weakness
Surfactant function and synthesis Explanation: ***Improved but still reduced compliance due to persistent chest wall restriction***
- Total respiratory system compliance follows the formula **1/C_total = 1/C_lungs + 1/C_chest_wall**, meaning the total compliance is limited by the stiffest component.
- While the lung transplant corrects the **pulmonary fibrosis**, the patient's **obesity** and **ankylosing spondylitis** cause extrinsic restriction that maintains a low **chest wall compliance**.
*Improved lung compliance but worsened chest wall compliance from surgery*
- Although surgical trauma can temporarily affect chest wall dynamics, the **ankylosing spondylitis** is the primary chronic factor limiting chest wall expansion here.
- The logic is flawed because the improvement in **lung compliance** from the donor lungs far outweighs any minor surgical stiffness in the long term.
*Worse compliance initially due to transplant rejection and denervation*
- **Denervation** typically leads to loss of the cough reflex but does not significantly alter the mechanical **elasticity** or compliance of the lung tissue itself.
- Acute rejection would decrease compliance, but the question asks for the "expected" outcome of a **successful bilateral transplant**.
*Return to completely normal respiratory compliance matching healthy individuals*
- Total compliance cannot return to normal because the **chest wall** remains stiff due to the patient's underlying skeletal and adipose conditions.
- Even with perfect donor lungs, the **extrapulmonary restriction** means the total system compliance will remain below the normal **200 mL/cm H2O**.
*No significant change because the primary problem is muscular weakness*
- The patient's primary problem in the lungs was **pulmonary fibrosis**, which is a mechanical parenchymal issue, not purely muscular weakness.
- Total compliance will definitely show a **significant increase** from the baseline of 25 mL/cm H2O because the severely stiff fibrotic lungs have been replaced.
More Surfactant function and synthesis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.