Obstructive lung disease effects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Obstructive lung disease effects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Obstructive lung disease effects US Medical PG Question 1: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Obstructive lung disease effects Explanation: ***Inhaling the entire vital capacity (VC)***
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
Obstructive lung disease effects US Medical PG Question 2: A previously healthy 64-year-old woman comes to the physician because of a dry cough and progressively worsening shortness of breath for the past 2 months. She has not had fever, chills, or night sweats. She has smoked one pack of cigarettes daily for the past 45 years. She appears thin. Examination of the lung shows a prolonged expiratory phase and end-expiratory wheezing. Spirometry shows decreased FEV1:FVC ratio (< 70% predicted), decreased FEV1, and a total lung capacity of 125% of predicted. The diffusion capacity of the lung (DLCO) is decreased. Which of the following is the most likely diagnosis?
- A. Bronchiectasis
- B. Interstitial lung disease
- C. Chronic obstructive pulmonary disease (Correct Answer)
- D. Hypersensitivity pneumonitis
- E. Bronchial asthma
Obstructive lung disease effects Explanation: ***Chronic obstructive pulmonary disease***
- The patient's long history of **smoking (45 pack-years)**, **prolonged expiratory phase**, and **end-expiratory wheezing** are classic signs of airway obstruction.
- Spirometry findings of a **decreased FEV1:FVC ratio** (< 70% predicted), **decreased FEV1**, **increased total lung capacity (TLC)**, and **decreased DLCO** are all highly indicative of **emphysema**, a subtype of COPD.
*Bronchiectasis*
- While it shares symptoms like cough and SOB, **bronchiectasis** is characterized by permanent **dilatation of bronchi** and profuse, chronic **sputum production**, which is not mentioned here.
- Spirometry typically shows **obstructive patterns**, but the marked increase in TLC and decreased DLCO are more specific to emphysema.
*Interstitial lung disease*
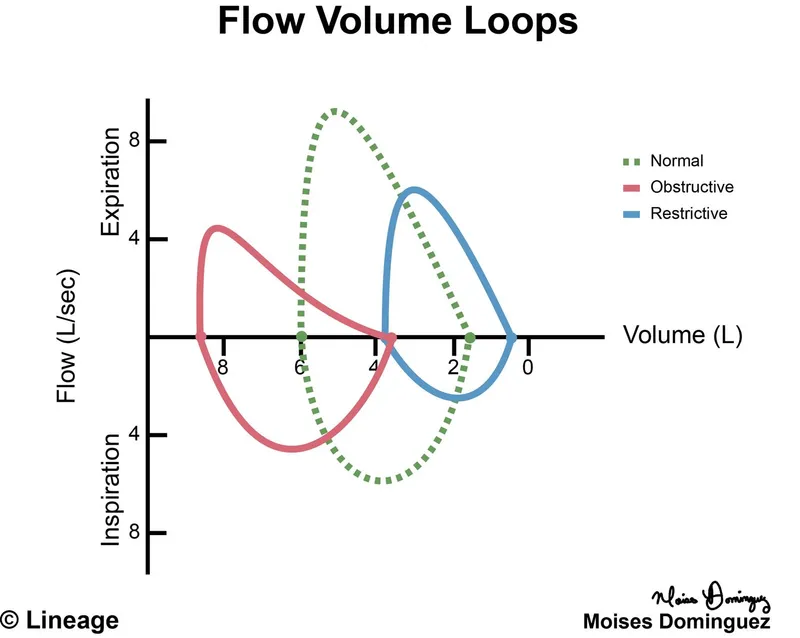
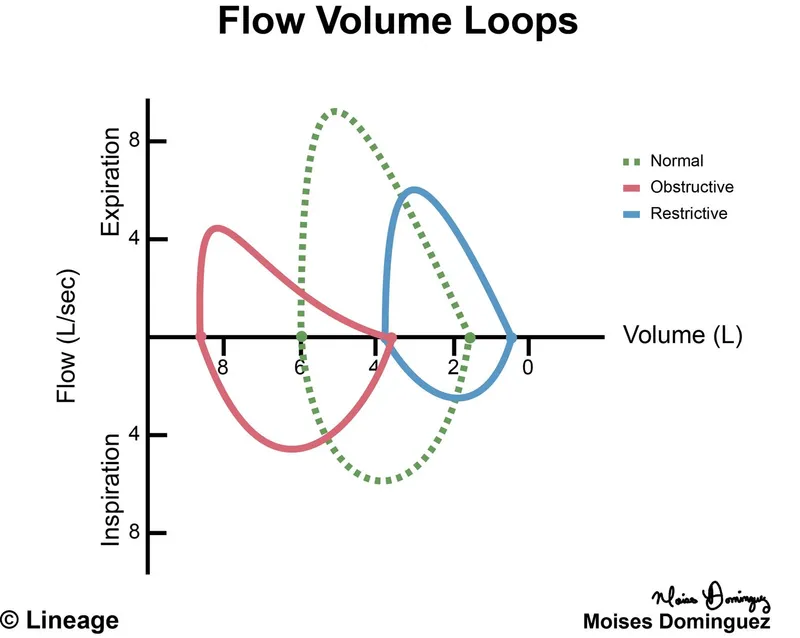
- This condition primarily causes a **restrictive lung pattern**, meaning a decreased TLC and normal or increased FEV1:FVC ratio.
- The patient's **increased TLC** and **obstructive spirometry** rule out a purely restrictive process.
*Hypersensitivity pneumonitis*
- This is an inflammatory response to inhaled antigens, often presenting with **recurrent episodes** of fever, chills, and cough, and can lead to restrictive physiology.
- The patient lacks a history of specific **antigen exposure** and presents with an obstructive pattern and increased TLC.
*Bronchial asthma*
- While asthma shares obstructive features like wheezing and a decreased FEV1:FVC ratio, it is characterized by **reversibility** of airway obstruction and typically does not cause a significantly **elevated TLC** or **decreased DLCO** in uncomplicated cases.
- The patient's long smoking history points away from asthma as the primary diagnosis.
Obstructive lung disease effects US Medical PG Question 3: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Obstructive lung disease effects Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Obstructive lung disease effects US Medical PG Question 4: A 22-year-old woman presents to the emergency department with a chief concern of shortness of breath. She was hiking when she suddenly felt unable to breathe and had to take slow deep breaths to improve her symptoms. The patient is a Swedish foreign exchange student and does not speak any English. Her past medical history and current medications are unknown. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 90% on room air. Physical exam is notable for poor air movement bilaterally and tachycardia. The patient is started on treatment. Which of the following best describes this patient's underlying pathology?
FEV1 = Forced expiratory volume in 1 second
FVC = Forced vital capacity
DLCO = Diffusing capacity of carbon monoxide
- A. Increased FVC
- B. Increased FEV1
- C. Increased FEV1/FVC
- D. Decreased airway tone
- E. Normal DLCO (Correct Answer)
Obstructive lung disease effects Explanation: ***Normal DLCO***
- This patient presents with an acute exacerbation of what is likely **asthma**, showing symptoms of **shortness of breath**, **tachycardia**, poor air movement bilaterally, and improvement with slow deep breaths. **Asthma** characteristically affects the airways and not the alveoli, thus the **diffusing capacity of carbon monoxide (DLCO)**, which measures gas exchange across the alveolar-capillary membrane, would be expected to be normal.
- In asthma, the primary problem is **bronchoconstriction** and **airway inflammation**, which restricts airflow but does not typically impair the diffusion of gases like carbon monoxide across the alveolar-capillary membrane.
*Increased FVC*
- **Forced vital capacity (FVC)** is often normal or even slightly reduced in asthma due to **air trapping** and early airway closure, not increased.
- An increased FVC is usually not associated with obstructive lung diseases like asthma but could potentially be seen in conditions where lung volumes are pathologically large, which is not the case here.
*Increased FEV1*
- **Forced expiratory volume in 1 second (FEV1)** is typically **decreased** in obstructive lung diseases like asthma due to **airflow limitation**.
- An increased FEV1 would indicate better-than-average expiratory flow, which contradicts the symptoms of shortness of breath and poor air movement in this patient.
*Increased FEV1/FVC*
- The **FEV1/FVC ratio** is characteristically **decreased** in obstructive lung diseases like asthma, indicating that a disproportionately smaller amount of air can be exhaled in the first second relative to the total forced vital capacity.
- An increased FEV1/FVC ratio would be a sign of a restrictive lung disease or normal lung function, not an exacerbation of an obstructive process.
*Decreased airway tone*
- The underlying pathology in asthma is typically **bronchoconstriction**, which means an **increased airway tone** and narrowing of the airways, rather than decreased.
- Decreased airway tone would imply bronchodilation, which would alleviate, not cause, the patient's symptoms of shortness of breath and poor air movement.
Obstructive lung disease effects US Medical PG Question 5: A 68-year-old man comes to the emergency room with difficulty in breathing. He was diagnosed with severe obstructive lung disease a few years back. He uses his medication but often has to come to the emergency room for intravenous therapy to help him breathe. He was a smoker for 40 years smoking two packs of cigarettes every day. Which of the following best represents the expected changes in his ventilation, perfusion and V/Q ratio?
- A. Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio
- B. Medium ventilation and perfusion, V/Q that equals 0.8
- C. Higher ventilation and perfusion with lower V/Q ratio
- D. Low ventilation, normal perfusion and low V/Q ratio (Correct Answer)
- E. Lower ventilation and perfusion, but higher V/Q ratio
Obstructive lung disease effects Explanation: ***Low ventilation, normal perfusion and low V/Q ratio***
- In severe **obstructive lung disease** (like COPD), there is airflow limitation, leading to areas of **hypoventilation** in the lungs.
- While ventilation is compromised, blood flow (perfusion) to these areas can remain relatively normal, resulting in a **decreased V/Q ratio**.
*Normal ventilation, low or nonexistent perfusion and infinite V/Q ratio*
- This scenario describes a lung unit with **dead space ventilation**, where there is ventilation but no blood flow (e.g., in a pulmonary embolism).
- The patient's history of **obstructive lung disease** primarily indicates impaired airflow, not a lack of perfusion.
*Medium ventilation and perfusion, V/Q that equals 0.8*
- A **V/Q ratio of 0.8** represents the **ideal normal** ventilation-perfusion matching in a healthy lung.
- The patient has severe obstructive lung disease, which by definition means there is significant mismatch, not normal physiology.
*Higher ventilation and perfusion with lower V/Q ratio*
- While hyperventilation can occur in attempts to compensate, the primary issue in obstructive disease is **impaired ventilation**, not increased ventilation, leading to decreased gas exchange.
- A lower V/Q ratio is expected, but it is driven by **low ventilation**, not higher ventilation and perfusion.
*Lower ventilation and perfusion, but higher V/Q ratio*
- Although both ventilation and perfusion can be affected in severe disease, a **higher V/Q ratio** typically implies areas of increased dead space (more ventilation than perfusion).
- In obstructive disease, the predominant problem is **impaired air entry**, leading to underventilated units with relatively preserved perfusion, thus a **low V/Q ratio**.
Obstructive lung disease effects US Medical PG Question 6: A 37-year-old woman comes to the physician because of a 10-month history of excessive daytime sleepiness and fatigue. She says she has difficulty concentrating and has fallen asleep at work on numerous occasions. She also reports having frequent headaches during the day. She has no difficulty falling asleep at night, but wakes up gasping for breath at least once. She has always snored loudly and began using an oral device to decrease her snoring a year ago. She has occasional lower back pain, for which she takes tramadol tablets 1–2 times per week. She also began taking one rabeprazole tablet daily 3 weeks ago. She does not smoke. She is 175 cm (5 ft 7 in) tall and weighs 119 kg (262 lb); BMI is 38.8 kg/m2. Her vital signs are within normal limits. Physical and neurologic examinations show no other abnormalities. Arterial blood gas analysis on room air shows:
pH 7.35
PCO2 51 mm Hg
PO2 64 mm Hg
HCO3- 29 mEq/L
O2 saturation 92%
An x-ray of the chest and ECG show no abnormalities. Which of the following is the most likely cause of this patient's condition?
- A. Chronic inflammatory airflow limitation
- B. Thickening of alveolar membranes
- C. Drug-induced respiratory depression
- D. Diurnal alveolar hypoventilation
- E. Apneic episodes with obstructed upper airways (Correct Answer)
Obstructive lung disease effects Explanation: **Apneic episodes with obstructed upper airways**
- This patient has classic **obstructive sleep apnea (OSA)**, characterized by **loud snoring**, **waking up gasping for breath** (witnessed apneas), and **excessive daytime sleepiness**.
- Her **obesity (BMI 38.8)** is a major risk factor for OSA, as excess soft tissue in the upper airway predisposes to collapse during sleep.
- The ABG shows **compensated respiratory acidosis (pH 7.35, PCO2 51, HCO3- 29)** and **hypoxemia (PO2 64, O2 sat 92%)**, indicating chronic hypoventilation from recurrent apneic episodes.
- OSA is the **underlying cause** of her condition; the oral device she uses is typically employed to treat OSA by repositioning the jaw to maintain airway patency.
- The question asks for the **cause** of her condition, which is the **obstructed upper airways** leading to apneic episodes during sleep.
*Diurnal alveolar hypoventilation*
- While this patient does have daytime (diurnal) hypoventilation as evidenced by the elevated PCO2, this is a **consequence** of severe OSA, not the primary cause.
- This describes **Obesity Hypoventilation Syndrome (OHS)**, which overlaps with OSA but refers specifically to the chronic hypoventilation state.
- The **obstructed airways causing apneic episodes** are the underlying pathophysiology that leads to the chronic hypoventilation.
*Chronic inflammatory airflow limitation*
- This refers to **COPD**, which typically presents with **dyspnea, chronic cough, and wheezing**.
- The patient is a **non-smoker**, has a **normal chest x-ray**, and lacks respiratory symptoms typical of COPD.
- The clinical picture is classic for OSA, not obstructive lung disease.
*Thickening of alveolar membranes*
- This describes **interstitial lung diseases (ILD)**, which present with **progressive dyspnea, restrictive physiology**, and often **interstitial infiltrates on imaging**.
- The patient's **normal chest x-ray** and lack of exertional dyspnea make ILD unlikely.
- Her symptoms are related to sleep-disordered breathing, not parenchymal lung disease.
*Drug-induced respiratory depression*
- **Tramadol** (an opioid) can cause respiratory depression, but she takes it only **1-2 times per week** for back pain.
- The ABG shows **compensated** respiratory acidosis with elevated bicarbonate, indicating a **chronic process** lasting weeks to months, not acute drug effect.
- Her symptoms (snoring, gasping, daytime sleepiness) and obesity clearly point to OSA as the cause.
Obstructive lung disease effects US Medical PG Question 7: A 62-year-old man presents to the emergency department for evaluation of a 2-year history of increasing shortness of breath. He also has an occasional nonproductive cough. The symptoms get worse with exertion. The medical history is significant for hypertension and he takes chlorthalidone. He is a smoker with a 40-pack-year smoking history. On physical examination, the patient is afebrile; the vital signs include: blood pressure 125/78 mm Hg, pulse 90/min, and respiratory rate 18/min. The body mass index (BMI) is 31 kg/m2. The oxygen saturation is 94% at rest on room air. A pulmonary examination reveals decreased breath sounds bilaterally, but is otherwise normal with no wheezes or crackles. The remainder of the examination is unremarkable. A chest radiograph shows hyperinflation of both lungs with mildly increased lung markings, but no focal findings. Based on this clinical presentation, which of the following is most likely?
- A. Decreased total lung capacity
- B. Increased DLCO
- C. Metabolic acidosis
- D. FEV1/FVC of 80% with an FEV1 of 82%
- E. FEV1/FVC of 65% (Correct Answer)
Obstructive lung disease effects Explanation: ***FEV1/FVC of 65%***
- This patient's symptoms (shortness of breath, nonproductive cough, worsening with exertion), significant smoking history (40-pack-years), and chest X-ray findings (**hyperinflation**, mildly increased lung markings) are highly suggestive of **Chronic Obstructive Pulmonary Disease (COPD)**, particularly **emphysema** given the hyperinflation and decreased breath sounds.
- COPD is characterized by **airflow limitation** that is not fully reversible, which is reflected by a **reduced FEV1/FVC ratio** (typically < 0.7 or < 70%).
*Decreased total lung capacity*
- **Decreased total lung capacity (TLC)** is characteristic of **restrictive lung diseases**, where lung expansion is limited (e.g., pulmonary fibrosis, interstitial lung disease).
- COPD, and especially emphysema, typically presents with **increased TLC** due to air trapping and hyperinflation, not decreased TLC.
*Increased DLCO*
- **Increased DLCO** (diffusing capacity of the lung for carbon monoxide) can be seen in conditions like **pulmonary hemorrhage** or **asthma**.
- In COPD, particularly emphysema, there is destruction of alveolar-capillary membranes, leading to a **decreased DLCO** due to impaired gas exchange.
*Metabolic acidosis*
- **Metabolic acidosis** is not a primary or direct feature of uncomplicated COPD. While severe respiratory failure in later stages might lead to some acid-base disturbances, directly attributing metabolic acidosis as a defining characteristic is incorrect.
- COPD primarily causes **respiratory acidosis** due to CO2 retention in advanced stages.
*FEV1/FVC of 80% with an FEV1 of 82%*
- An **FEV1/FVC ratio of 80%** (or 0.8) and an **FEV1 of 82%** of predicted values are within the normal range and indicate **normal spirometry**.
- This would rule out significant airflow obstruction, which is central to the diagnosis of COPD.
Obstructive lung disease effects US Medical PG Question 8: A 3-day-old newborn is brought to the physician because of abdominal distention, inconsolable crying, and 3 episodes of bilious vomiting since the previous evening. He was delivered at home at 40 weeks' gestation by a trained midwife. He has not passed meconium. Physical examination shows abdominal distention, a tight anal sphincter, and an explosive passage of air and feces on removal of the examining finger. Abnormal development of which of the following best explains this patient's condition?
- A. Submucosa and muscularis externa (Correct Answer)
- B. Epithelium and submucosa
- C. Muscularis mucosae and lamina propria
- D. Muscularis mucosae and serosa
- E. Epithelium and lamina propria
Obstructive lung disease effects Explanation: ***Submucosa and muscularis externa***
- This patient's symptoms (abdominal distention, bilious vomiting, failure to pass meconium, tight anal sphincter with explosive stool passage) are classic for **Hirschsprung disease**.
- Hirschsprung disease is characterized by the absence of **ganglion cells** in the myenteric (Auerbach's) plexus (located between the inner circular and outer longitudinal layers of the muscularis externa) and the submucosal (Meissner's) plexus (located in the submucosa) of the distal colon.
*Epithelium and submucosa*
- The **epithelium** is involved in absorption and secretion, and its primary dysfunction would typically lead to diarrhea or malabsorption, not an obstructive picture like this.
- While the submucosa contains Meissner's plexus, the lack of ganglion cells in the muscularis externa's Auerbach's plexus is equally crucial to the pathophysiology of Hirschsprung disease.
*Muscularis mucosae and lamina propria*
- The **muscularis mucosae** is a thin layer that causes folding of the mucosa, while the **lamina propria** is connective tissue supporting the epithelium; neither is directly implicated in the primary pathology of Hirschsprung disease which involves neural crest cell migration.
- Absence of ganglion cells in these layers would not explain the severe motility disorder observed in Hirschsprung disease involving the entire bowel wall.
*Muscularis mucosae and serosa*
- The **serosa** is the outermost connective tissue layer and is not directly involved in the intrinsic innervation or motility problems seen in Hirschsprung disease.
- Dysfunction of the muscularis mucosae alone would not result in the functional obstruction due to absent peristalsis.
*Epithelium and lamina propria*
- The **epithelium** and **lamina propria** are primarily involved in the digestive and absorptive functions of the gut, and their abnormal development would not typically cause the characteristic features of Hirschsprung disease, which is a neurodevelopmental disorder of the gut.
- The core issue in Hirschsprung disease lies in the neural plexuses controlling motility, not the mucosal lining.
Obstructive lung disease effects US Medical PG Question 9: An investigator is studying the outcomes of a malaria outbreak in an endemic region of Africa. 500 men and 500 women with known malaria exposure are selected to participate in the study. Participants with G6PD deficiency are excluded from the study. The clinical records of the study subjects are reviewed and their peripheral blood smears are evaluated for the presence of Plasmodium trophozoites. Results show that 9% of the exposed population does not have clinical or laboratory evidence of malaria infection. Which of the following best explains the absence of infection seen in this subset of participants?
- A. Translocation of c-myc gene
- B. Glutamic acid substitution in the β-globin chain (Correct Answer)
- C. Inherited mutation affecting ribosome synthesis
- D. Inherited defect in erythrocyte membrane ankyrin protein
- E. Defective X-linked ALA synthase gene
Obstructive lung disease effects Explanation: ***Glutamic acid substitution in the β-globin chain***
- This describes **sickle cell trait (heterozygous HbS)**, which confers significant protection against severe malaria, explaining the absence of infection despite exposure.
- Individuals with sickle cell trait have **abnormally shaped red blood cells** under low oxygen conditions, which are less hospitable for **Plasmodium falciparum** growth and are more rapidly cleared by the spleen.
*Translocation of c-myc gene*
- A **t(8;14) translocation of the c-myc gene** is characteristic of **Burkitt lymphoma**, a B-cell malignancy, and has no protective effect against malaria.
- This genetic alteration leads to overexpression of **c-myc**, a proto-oncogene, contributing to uncontrolled cell growth.
*Inherited mutation affecting ribosome synthesis*
- Defects in **ribosome synthesis** can lead to various **ribosomopathies**, affecting cell proliferation and function, but they are not known to provide protection against malaria.
- Such mutations often result in syndromes with **developmental abnormalities** or **bone marrow failure**.
*Inherited defect in erythrocyte membrane ankyrin protein*
- Defects in **ankyrin protein** are associated with **hereditary spherocytosis**, causing fragile, spherical red blood cells that are prematurely destroyed.
- While hereditary spherocytosis can reduce malaria severity, its role in preventing initial infection is less pronounced, and the question refers to absence of infection.
*Defective X-linked ALA synthase gene*
- A defective **X-linked ALA synthase gene** (ALAS2) is associated with **X-linked sideroblastic anemia**, causing impaired heme synthesis.
- This condition is characterized by **microcytic, hypochromic anemia** and iron overload in erythroid precursors, with no known protective effect against malaria.
Obstructive lung disease effects US Medical PG Question 10: A 55-year-old man with a 60 pack-year smoking history is referred by his primary care physician for a pulmonary function test (PFT). A previously obtained chest x-ray is shown below. Which of the following will most likely appear in his PFT report?
- A. Residual volume increased, total lung capacity decreased
- B. Residual volume normal, total lung capacity decreased
- C. Residual volume normal, total lung capacity normal
- D. Residual volume decreased, total lung capacity increased
- E. Residual volume increased, total lung capacity increased (Correct Answer)
Obstructive lung disease effects Explanation: ***Residual volume increased, total lung capacity increased***
- The chest X-ray shows **hyperinflation** and a **flattened diaphragm**, which are classic signs of **emphysema**, a type of COPD.
- In emphysema, destruction of alveolar walls leads to air trapping, resulting in an **increased residual volume** and **total lung capacity**.
*Residual volume increased, total lung capacity decreased*
- An increased residual volume suggests **air trapping**, typical of obstructive lung diseases like emphysema.
- However, a **decreased total lung capacity** is characteristic of restrictive lung diseases, which would contradict the clinical and radiological findings for emphysema.
*Residual volume normal, total lung capacity decreased*
- A **normal residual volume** indicates no significant air trapping, which is inconsistent with emphysema.
- A **decreased total lung capacity** is seen in restrictive lung diseases, not obstructive diseases like emphysema.
*Residual volume normal, total lung capacity normal*
- **Normal lung volumes** would indicate healthy lung function, which is not expected in a patient with a heavy smoking history and radiological evidence of emphysema.
- The patient's 60 pack-year smoking history strongly points towards significant lung pathology.
*Residual volume decreased, total lung capacity increased*
- A **decreased residual volume** would suggest improved exhalation and less air trapping, which is contrary to the pathophysiology of emphysema.
- While total lung capacity can be increased in emphysema, the decrease in residual volume makes this option incorrect.
More Obstructive lung disease effects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.