Definition of lung compliance US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Definition of lung compliance. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Definition of lung compliance US Medical PG Question 1: An 85-year-old man with hypertension and type 2 diabetes mellitus is brought to the emergency department because of a 2-day history of shortness of breath. He has smoked one pack of cigarettes daily for 30 years. His temperature is 36.9°C (98.4°F), pulse is 100/min, respirations are 30/min, and blood pressure is 138/75 mm Hg. Pulmonary function testing shows decreased tidal volume and normal lung compliance. Which of the following is the most likely underlying etiology of this patient's tachypnea?
- A. Diabetic ketoacidosis
- B. Rib fracture
- C. Pulmonary edema (Correct Answer)
- D. Emphysema exacerbation
- E. Tension pneumothorax
Definition of lung compliance Explanation: ***Pulmonary edema***
- This patient's **hypertension** and **diabetes** are major risk factors for heart failure, and the acute onset of **shortness of breath** with **tachypnea** suggests cardiogenic pulmonary edema.
- **Decreased tidal volume** occurs because fluid accumulation in the interstitium and alveoli reduces functional lung capacity, prompting rapid, shallow breathing to maintain minute ventilation.
- While pulmonary edema typically causes **decreased lung compliance** due to fluid-stiffened lungs, early or mild cases may show relatively preserved compliance, or the normal compliance here may reflect measurement timing or technique. The clinical picture and decreased tidal volume strongly support pulmonary edema.
- The combination of cardiac risk factors, acute dyspnea, tachypnea, and altered breathing pattern make this the most likely diagnosis.
*Diabetic ketoacidosis*
- DKA causes **Kussmaul respirations** (deep, labored breathing) to compensate for metabolic acidosis, not the shallow breathing pattern (decreased tidal volume) seen here.
- DKA typically presents with polyuria, polydipsia, abdominal pain, nausea, and fruity breath odor, which are not mentioned.
- While this patient has diabetes, the respiratory pattern and absence of typical DKA symptoms make this less likely.
*Rib fracture*
- Rib fractures cause **pleuritic chest pain** that worsens with breathing, leading to voluntary splinting and reduced tidal volume.
- However, there is **no history of trauma** or chest pain reported.
- Pain from rib fractures would be localized, and the acute 2-day onset of dyspnea without trauma makes this unlikely.
*Emphysema exacerbation*
- Emphysema is characterized by **increased lung compliance** (hyperinflation) due to alveolar wall destruction, which contradicts the normal compliance finding.
- While the patient has a significant smoking history, the **normal lung compliance** argues against emphysema.
- COPD exacerbations typically present with wheezing, productive cough, and hyperinflation, not decreased tidal volume with normal compliance.
*Tension pneumothorax*
- Tension pneumothorax presents with **severe respiratory distress**, unilateral absent breath sounds, **hypotension**, tracheal deviation, and jugular venous distension.
- This patient's **blood pressure is normal** (138/75 mm Hg) and there's no mention of absent breath sounds or hemodynamic compromise.
- The clinical presentation does not support this life-threatening emergency.
Definition of lung compliance US Medical PG Question 2: A 28-year-old patient presents to the hospital complaining of progressively worsening dyspnea and a dry cough. Radiographic imaging is shown below. Pulmonary function testing (PFT's) reveals a decreased FEV1 and FEV1/FVC, but an increased TLC. The patient states that he does not smoke. Which of the following conditions is most consistent with the patient's symptoms?
- A. Hypersensitivity pneumonitis
- B. Chronic bronchitis
- C. Alpha1-antitrypsin deficiency (Correct Answer)
- D. Pneumothorax
- E. Asthma
Definition of lung compliance Explanation: ***Alpha1-antitrypsin deficiency***
- The combination of **decreased FEV1**, **decreased FEV1/FVC**, and **increased TLC** without a history of smoking is highly suggestive of **emphysema**, which can be caused by alpha1-antitrypsin deficiency.
- This genetic condition leads to a lack of protection against **elastase**, causing early-onset panacinar emphysema, typically affecting the lung bases even in non-smokers.
*Hypersensitivity pneumonitis*
- This condition typically presents with a **restrictive pattern** on PFTs (decreased TLC, normal or increased FEV1/FVC), not an obstructive pattern with increased TLC.
- It is an immune-mediated interstitial lung disease, often presenting with symptoms like dyspnea and cough, but the PFTs are inconsistent.
*Chronic bronchitis*
- While chronic bronchitis causes an **obstructive pattern** (decreased FEV1, decreased FEV1/FVC), it primarily manifests with a **chronic productive cough** (at least three months per year for two consecutive years) and is usually associated with smoking.
- An **increased TLC** is not typical in isolated chronic bronchitis; TLC is often normal or slightly increased, but not as pronounced as in emphysema.
*Pneumothorax*
- A pneumothorax is an acute condition involving air in the pleural space, leading to sudden onset dyspnea and chest pain, and would show a **collapsed lung** on imaging, not an obstructive pattern with increased TLC.
- It results in a **reduced lung volume** and would not cause an obstructive pattern with increased TLC on PFTs.
*Asthma*
- Asthma presents with **reversible airway obstruction** (decreased FEV1, decreased FEV1/FVC) but usually involves episodic wheezing and dyspnea, often triggered by allergens.
- While TLC can be increased during severe exacerbations due to **air trapping**, patients usually respond to bronchodilators and do not typically present with progressive, non-reversible obstruction and uniformly increased TLC like emphysema.
Definition of lung compliance US Medical PG Question 3: A 63-year-old man with alpha-1-antitrypsin deficiency is brought to the emergency department 1 hour after his daughter found him unresponsive. Despite appropriate care, the patient dies. At autopsy, examination of the lungs shows enlargement of the airspaces in the respiratory bronchioles and alveoli. Enzymatic activity of which of the following cells is the most likely cause of these findings?
- A. Alveolar macrophages (Correct Answer)
- B. Ciliated bronchiolar epithelial cells
- C. Elastic fibers in alveolar septa
- D. Type I pneumocytes
- E. Alveolar septal cells
Definition of lung compliance Explanation: ***Alveolar macrophages***
- In **alpha-1-antitrypsin deficiency**, alveolar macrophages (and neutrophils) release **elastase**, which is normally inhibited by alpha-1-antitrypsin.
- Unchecked elastase activity from alveolar macrophages leads to the **destruction of elastic fibers** in the alveolar walls, causing emphysema with characteristic **panacinar** distribution (worse in lower lobes).
- This results in enlargement of airspaces distal to terminal bronchioles.
*Ciliated bronchiolar epithelial cells*
- These cells are primarily involved in **mucociliary clearance** and do not produce proteolytic enzymes that degrade elastic tissue.
- Their dysfunction would lead to impaired mucus clearance and increased susceptibility to infections, but not emphysema.
*Elastic fibers in alveolar septa*
- Elastic fibers are **extracellular matrix components**, not cells.
- While their destruction is the pathological mechanism of emphysema, they do not have enzymatic activity.
*Type I pneumocytes*
- **Type I pneumocytes** form the structural lining of the alveoli and are primarily involved in gas exchange.
- They do not produce elastase or other proteolytic enzymes responsible for tissue destruction in emphysema.
*Alveolar septal cells*
- This term broadly refers to structural cells including Type I and Type II pneumocytes.
- While these cells may be damaged secondarily in emphysema, they do not produce the elastase responsible for elastic fiber destruction.
Definition of lung compliance US Medical PG Question 4: A 60-year-old woman with a history of emphysema has been referred by her pulmonologist for follow-up pulmonary function testing. During the test, the patient reaches a point where her airway pressure is equal to the atmospheric pressure. Which of the following is most likely to be found during this respiratory state?
- A. Pulmonary vascular resistance is at a maximum
- B. Transmural pressure of the lung-chest wall system is at a maximum
- C. Transmural pressure of the chest wall is at a minimum
- D. Pulmonary vascular resistance is at a minimum (Correct Answer)
- E. Transmural pressure of the lung-chest wall system is at a minimum
Definition of lung compliance Explanation: ***Pulmonary vascular resistance is at a minimum***
- When airway pressure equals atmospheric pressure during a pulmonary function test, the lungs are at **functional residual capacity (FRC)** or resting state.
- At FRC, **pulmonary vascular resistance (PVR)** is at its lowest point due to the optimal balance between alveolar and extra-alveolar vessel compression/distension.
- Extra-alveolar vessels are compressed at low lung volumes, while alveolar vessels are compressed at high lung volumes. At FRC, both are optimally distended, resulting in **minimal PVR**.
*Pulmonary vascular resistance is at a maximum*
- PVR increases at very low lung volumes (due to extra-alveolar vessel compression) and very high lung volumes (due to alveolar vessel compression).
- The resting state (airway pressure equals atmospheric pressure) corresponds to FRC, where PVR is **minimal, not maximal**.
*Transmural pressure of the lung-chest wall system is at a maximum*
- Transmural pressure of the lung-chest wall system represents the pressure difference across the entire respiratory system.
- This pressure is higher during inspiration or forced expiration when the system is stretched or compressed.
- At FRC (airway pressure equals atmospheric pressure), the system is at **resting equilibrium**, not at maximal transmural pressure.
*Transmural pressure of the chest wall is at a minimum*
- Transmural pressure across the chest wall is the difference between intrapleural pressure and atmospheric pressure.
- This pressure is not at a minimum when airway pressure equals atmospheric pressure.
- Chest wall transmural pressure is actually minimal near **residual volume (RV)**, where the chest wall recoils inward most strongly.
*Transmural pressure of the lung-chest wall system is at a minimum*
- Transmural pressure of the lung-chest wall system reflects the elastic recoil forces of the combined system.
- At FRC (airway pressure equals atmospheric pressure), elastic recoil forces are balanced at equilibrium, but transmural pressure is **not at a minimum**—it represents the neutral resting state.
Definition of lung compliance US Medical PG Question 5: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Definition of lung compliance Explanation: ***Inhaling the entire vital capacity (VC)***
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
Definition of lung compliance US Medical PG Question 6: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Definition of lung compliance Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Definition of lung compliance US Medical PG Question 7: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Definition of lung compliance Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Definition of lung compliance US Medical PG Question 8: A 60-year-old man presents with breathlessness for the past 3 months. His symptoms have been getting progressively worse during this time. He denies any history of cough, fever, or chest pain. He works at a local shipyard and is responsible for installing the plumbing aboard the vessels. His past medical history is significant for hypertension for which he takes metoprolol every day. He denies smoking and any illicit drug use. His pulse is 74/min, respiratory rate is 14/min, blood pressure is 130/76 mm Hg, and temperature is 36.8°C (98.2°F). Physical examination is significant for fine bibasilar crackles at the end of inspiration without digital clubbing. Which of the following additional findings would most likely be present in this patient?
- A. Increased pulmonary capillary wedge pressure
- B. Increased residual lung volume
- C. Reduced FEV1/FVC ratio
- D. Decreased diffusing capacity of CO (Correct Answer)
- E. Decreased pulmonary arterial pressure
Definition of lung compliance Explanation: ***Decreased diffusing capacity of CO***
- This patient's occupation at a **shipyard**, progressive dyspnea, and bibasilar crackles without clubbing, along with normal vital signs, are highly suggestive of **asbestosis**, a type of **interstitial lung disease (ILD)**.
- ILDs cause **fibrosis of the alveolar-capillary membrane**, leading to impaired gas exchange and a characteristic **reduction in DLCO (diffusing capacity of the lung for carbon monoxide)**. This is a hallmark of parenchymal lung disease.
*Increased pulmonary capillary wedge pressure*
- An elevated **pulmonary capillary wedge pressure (PCWP)** indicates **left-sided heart failure** or **pulmonary venous hypertension**.
- While dyspnea can be a symptom of heart failure, the patient's normal blood pressure and absence of cardiac-specific symptoms or signs point away from primary cardiac pathology.
*Increased residual lung volume*
- **Increased residual lung volume** is a characteristic finding in **obstructive lung diseases** such as **COPD** and **asthma**, where there is air trapping due to airflow limitation.
- The patient's presentation with progressive dyspnea and bibasilar crackles is more consistent with a **restrictive lung disorder** like asbestosis, which typically causes **decreased lung volumes**.
*Reduced FEV1/FVC ratio*
- A **reduced FEV1/FVC ratio** is the hallmark of **obstructive lung diseases**, indicating airflow limitation.
- In **restrictive lung diseases** like asbestosis, both FEV1 and FVC are typically reduced proportionally, often resulting in a **normal or even increased FEV1/FVC ratio**.
*Decreased pulmonary arterial pressure*
- **Pulmonary arterial pressure (PAP)** is typically **normal or increased** in patients with interstitial lung disease due to **hypoxic vasoconstriction** and vascular remodeling.
- A decreased PAP would be an unusual and atypical finding in such a patient and is not associated with this clinical picture.
Definition of lung compliance US Medical PG Question 9: A 45-year-old man presents to the physician with complaints of burning pain in both feet and lower legs for 3 months. He reports that the pain is especially severe at night. He has a history of diabetes mellitus for the past 5 years, and he frequently skips his oral antidiabetic medications. His temperature is 36.9°C (98.4°F), heart rate is 80/min, respiratory rate is 15/min, and blood pressure is 120/80 mm Hg. His weight is 70 kg (154.3 lb) and height is 165 cm (approx. 5 ft 5 in). The neurologic examination reveals loss of sensations of pain and temperature over the dorsal and ventral sides of the feet and over the distal one-third of both legs. Proprioception is normal; knee jerks and ankle reflexes are also normal. The tone and strength in all muscles are normal. The hemoglobin A1C is 7.8%. Involvement of what type of nerve fibers is the most likely cause of the patient’s symptoms?
- A. Aδ & C fibers (Correct Answer)
- B. Aα & Aβ fibers
- C. Aγ & B fibers
- D. Aγ & C fibers
- E. Aβ & Aγ fibers
Definition of lung compliance Explanation: ***Aδ & C fibers***
- The patient's symptoms of **burning pain** and loss of **pain and temperature sensations** are characteristic of small fiber neuropathy, which primarily involves **Aδ and C fibers**.
- These are **unmyelinated or thinly myelinated** fibers responsible for transmitting pain (nociception) and thermal sensations, and they are frequently affected in **diabetic neuropathy**.
*Aα & Aβ fibers*
- **Aα fibers** are large, myelinated fibers involved in **proprioception** and motor function; **Aβ fibers** transmit touch and pressure sensations.
- The patient's **normal proprioception** and motor strength indicate that these fibers are largely spared.
*Aγ & B fibers*
- **Aγ fibers** innervate muscle spindles and are involved in **motor control** and stretch reflexes.
- **B fibers** are preganglionic autonomic fibers; neither is directly responsible for pain and temperature sensation.
*Aγ & C fibers*
- While **C fibers** are involved in pain and temperature, **Aγ fibers** are primarily motor, controlling muscle spindle sensitivity.
- The combination does not accurately represent the sensory deficits observed in this patient.
*Aβ & Aγ fibers*
- **Aβ fibers** are involved in touch and pressure, and **Aγ fibers** are motor.
- The patient's primary complaint is burning pain and loss of temperature sensation, not deficits related to these fiber types.
Definition of lung compliance US Medical PG Question 10: A 68-year-old man with both severe COPD (emphysema) and newly diagnosed idiopathic pulmonary fibrosis presents with worsening dyspnea. His pressure-volume curve shows a complex pattern with features of both diseases. Static compliance measured at mid-lung volumes is 120 mL/cm H2O. His pulmonologist must decide on optimal management. Synthesizing the pathophysiology of both conditions, what represents the most significant clinical challenge in managing his combined disease?
- A. Pulmonary rehabilitation cannot address the opposing mechanical derangements
- B. The increased compliance from emphysema completely negates decreased compliance from fibrosis
- C. The opposing effects on compliance create a pseudonormal total respiratory compliance masking disease severity (Correct Answer)
- D. Emphysema treatment with bronchodilators will worsen fibrosis progression
- E. Oxygen therapy beneficial for COPD will accelerate fibrotic changes
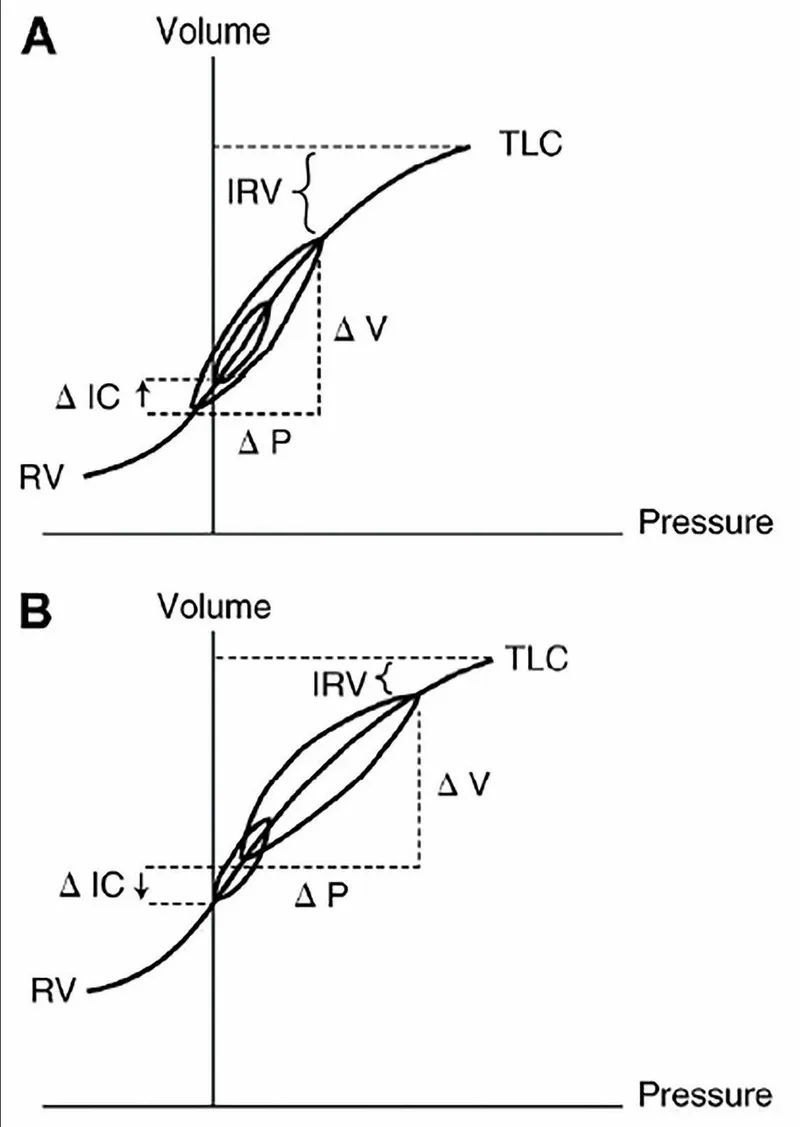
Definition of lung compliance Explanation: ***The opposing effects on compliance create a pseudonormal total respiratory compliance masking disease severity***
- In **Combined Pulmonary Fibrosis and Emphysema (CPFE)**, the **increased lung compliance** from upper-lobe emphysema is offset by the **decreased compliance** from lower-lobe fibrosis.
- This results in a **pseudonormalization** of lung volumes (like FVC and TLC) and compliance measurements, which can lead to a significant **underestimation of disease severity** during clinical assessment.
*Pulmonary rehabilitation cannot address the opposing mechanical derangements*
- While mechanical derangements are complex, **pulmonary rehabilitation** remains a cornerstone of management to improve functional capacity and reduce dyspnea in both conditions.
- The challenge is not that rehabilitation is ineffective, but rather the **physiological monitoring** and objective assessment of progress are hampered by masked lung volumes.
*The increased compliance from emphysema completely negates decreased compliance from fibrosis*
- The two forces do not perfectly negate each other; rather, they coexist to produce a **paradoxical physiological profile** where static measurements appear mid-range while gas exchange is severely impaired.
- Patients often exhibit a **disproportionate reduction in DLCO** (diffusion capacity) despite relatively preserved lung volumes, indicating the negation is only superficial and numerical.
*Emphysema treatment with bronchodilators will worsen fibrosis progression*
- There is no clinical evidence suggesting that **bronchodilators** (beta-agonists or anticholinergics) used for COPD/emphysema accelerate the **pathological scarring** seen in idiopathic pulmonary fibrosis.
- Bronchodilators primarily target **airway smooth muscle** and do not interfere with the fibroblastic pathways driving interstitial lung disease.
*Oxygen therapy beneficial for COPD will accelerate fibrotic changes*
- **Long-term oxygen therapy (LTOT)** is used to treat chronic hypoxemia in both COPD and fibrosis and does not cause or accelerate **lung remodeling** or fibrosis.
- While high concentrations of inspired oxygen (FiO2) can cause **oxidative stress**, the flow rates used for clinical management do not contribute to the progression of pulmonary fibrosis.
More Definition of lung compliance US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 , normal, and low (fibrosis) lung compliance)
, normal, and low (fibrosis) lung compliance)
