Cardiovascular

On this page
🫀 The Cardiac Engine: Mastering Cardiovascular Fundamentals
You'll master the cardiovascular system from molecular mechanisms to bedside decisions, learning how the heart generates force, how hemodynamics drive clinical presentations, and how to recognize patterns that distinguish life-threatening emergencies from benign variants. This lesson builds your diagnostic reasoning through pathophysiology, then equips you with evidence-based treatment algorithms and integration frameworks that transform scattered facts into confident clinical action when seconds matter.
The Cardiovascular Architecture: Structural Mastery
The cardiovascular system operates as a dual-circuit hydraulic network with precise pressure gradients and flow dynamics:
-
Systemic Circuit
- Left ventricle generates 120 mmHg systolic pressure
- Aortic compliance accommodates 70 mL stroke volume
- Peripheral resistance maintains 80 mmHg diastolic pressure
- Arterioles control 60% of total resistance
- Capillaries facilitate exchange across 500 m² surface area
- Venous return carries 75% of total blood volume
-
Pulmonary Circuit
- Right ventricle generates 25 mmHg systolic pressure
- Pulmonary vascular resistance 1/10th of systemic
- Gas exchange occurs across 70 m² alveolar surface
- Pulmonary capillary transit time: 0.75 seconds
- Oxygen saturation increases from 75% to 98%
📌 Remember: "LAMP" - Left high pressure (120/80), Aortic compliance, Mitral inflow, Pulmonary low pressure (25/8). The pressure differential drives all cardiac pathophysiology.

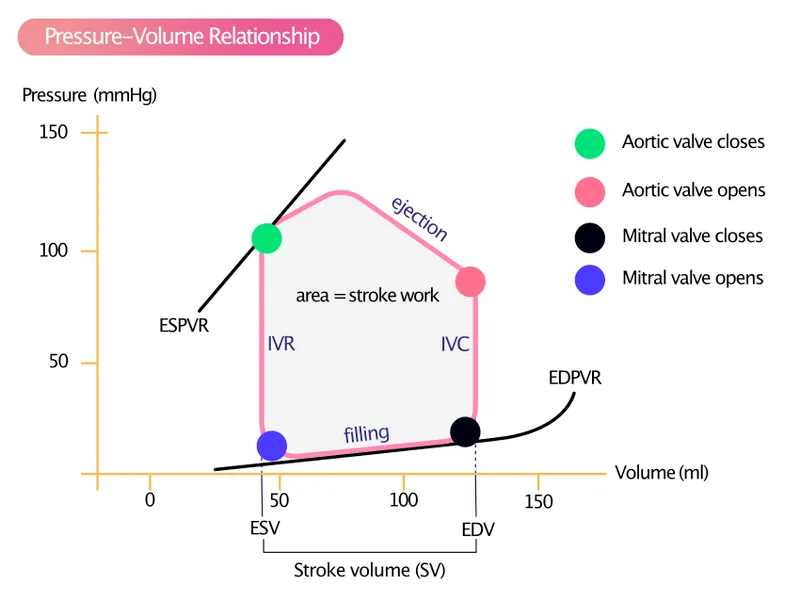
Cardiac Cycle Dynamics: The Hemodynamic Blueprint
| Phase | Duration (ms) | LV Pressure (mmHg) | Aortic Pressure (mmHg) | Valve Status | Clinical Correlation |
|---|---|---|---|---|---|
| Isovolumic Contraction | 50 | 0→120 | 80 | All closed | S1 heart sound |
| Ejection | 250 | 120→100 | 80→120 | Aortic open | Systolic murmurs |
| Isovolumic Relaxation | 80 | 100→0 | 80 | All closed | S2 heart sound |
| Filling | 420 | 0→12 | 80 | Mitral open | S3/S4 gallops |
| Atrial Kick | 100 | 12→0 | 80 | Mitral open | 25% of filling |
⭐ Clinical Pearl: Isovolumic contraction time increases in aortic stenosis (prolonged ejection) and decreases in mitral regurgitation (early pressure relief). This timing differential appears on echocardiography as altered IVCT/ET ratios.
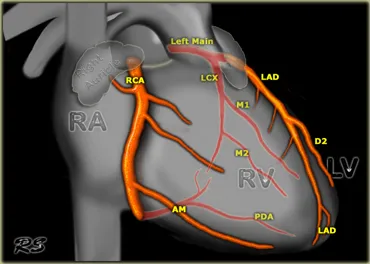
Coronary Circulation: The Heart's Lifeline
-
Right Coronary Artery (RCA) Territory
- Supplies inferior wall and posterior septum
- 85% of population has right-dominant circulation
- Provides posterior descending artery (PDA)
- Inferior MI affects leads II, III, aVF
- 40% develop heart block (AV node supply)
-
Left Anterior Descending (LAD) Territory
- Supplies anterior wall and anterior septum
- "Widow maker" - largest myocardial territory
- Diagonal branches supply lateral wall
- Anterior STEMI affects leads V1-V4
- 60% of left ventricular mass at risk
-
Left Circumflex (LCX) Territory
- Supplies lateral and posterior walls
- 15% of population has left-dominant circulation
- Often produces "silent" infarctions
- Lateral MI affects leads I, aVL, V5-V6
- Posterior MI shows tall R waves in V1-V2
💡 Master This: Coronary dominance determines AV node blood supply. Right dominance (85%) means inferior MI causes heart block. Left dominance (15%) means lateral MI causes conduction abnormalities. This knowledge predicts complications before they occur.
Understanding these cardiovascular fundamentals creates the foundation for recognizing pathological patterns. Connect these normal relationships through hemodynamic principles to understand how disease disrupts cardiac function.
🫀 The Cardiac Engine: Mastering Cardiovascular Fundamentals
⚡ The Hemodynamic Powerhouse: Cardiac Function Mechanisms
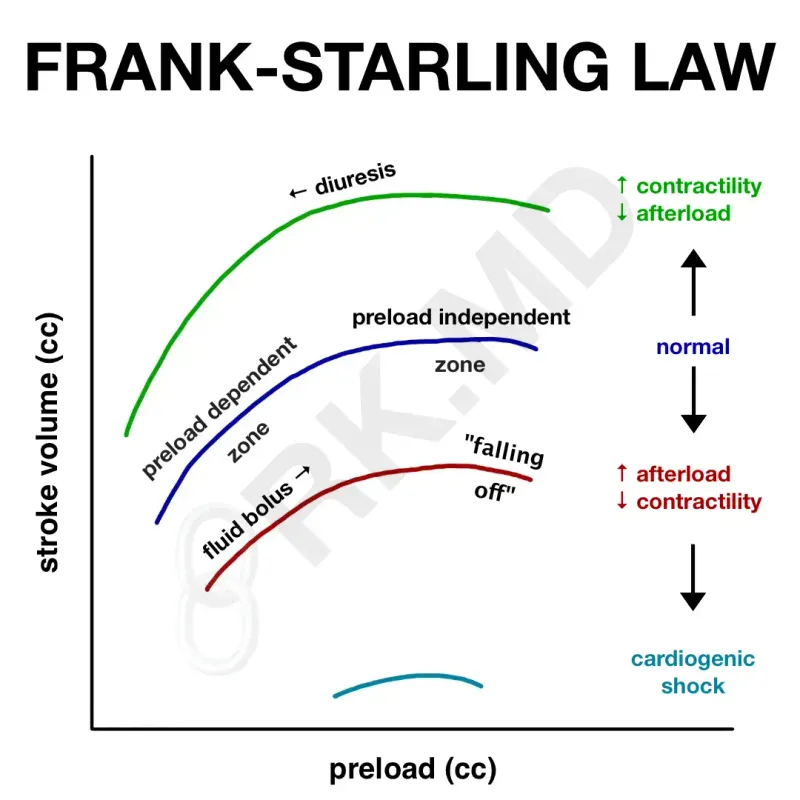
Preload Dynamics: The Filling Foundation
Preload represents ventricular end-diastolic volume, determining stroke volume through the Frank-Starling mechanism:
-
Normal Preload Parameters
- Right atrial pressure: 2-8 mmHg
- Pulmonary capillary wedge pressure: 6-12 mmHg
- Left ventricular end-diastolic pressure: 8-12 mmHg
- Optimal filling occurs at 12-15 mmHg
- Pulmonary edema develops above 18 mmHg
- Cardiogenic shock occurs below 6 mmHg
-
Preload Manipulation
- Increase: IV fluids, trendelenburg position, leg elevation
- Decrease: Diuretics, nitrates, dialysis
- Assessment: CVP, PCWP, IVC diameter on echo
- IVC collapse >50% suggests hypovolemia
- IVC diameter >2.1 cm suggests elevated preload
📌 Remember: "STARLING" - Stroke volume increases with Tension (preload), Afterload reduction, Rate optimization, Lusitropy (relaxation), Inotropy (contractility), Neurohormonal balance, Geometry preservation.
Afterload Mechanics: The Pressure Challenge
Afterload represents systemic vascular resistance opposing ventricular ejection:
| Condition | SVR (dynes·s/cm⁵) | MAP (mmHg) | Cardiac Response | Clinical Manifestation |
|---|---|---|---|---|
| Normal | 800-1200 | 70-100 | Baseline function | Asymptomatic |
| Hypertension | >1500 | >110 | LV hypertrophy | Exertional dyspnea |
| Septic shock | <600 | <65 | Hyperdynamic | Warm extremities |
| Cardiogenic shock | >1800 | <60 | Pump failure | Cold, clammy skin |
| Aortic stenosis | Variable | Normal | Pressure overload | Syncope, angina |
- ACE inhibitors: Reduce SVR by 15-25%
- Hydralazine: Direct vasodilation, reduce SVR by 20-30%
- Nitroprusside: Immediate reduction, titrate to 10-15% MAP decrease
- Improves stroke volume in heart failure
- Reduces myocardial oxygen consumption
- Enhances forward flow in mitral regurgitation
⭐ Clinical Pearl: In acute mitral regurgitation, afterload reduction with nitroprusside increases forward stroke volume by 30-40% while reducing regurgitant fraction. Target MAP 65-75 mmHg to optimize cardiac output without compromising perfusion.
Contractility Control: The Inotropic Engine
Contractility represents intrinsic myocardial performance independent of loading conditions:
-
Positive Inotropes
- Dobutamine: β1-agonist, increases cAMP, +25-50% contractility
- Milrinone: PDE-3 inhibitor, increases cAMP, +30-60% contractility
- Digoxin: Na-K ATPase inhibitor, increases intracellular calcium
- Therapeutic level: 1.0-2.0 ng/mL
- Toxicity risk increases above 2.5 ng/mL
- 15% mortality reduction in heart failure
-
Contractility Assessment
- Ejection fraction: Normal >55%, reduced <40%
- dP/dt: Rate of pressure rise, normal >1200 mmHg/s
- Fractional shortening: Normal >25%
- Correlates with invasive contractility measures
- Independent predictor of heart failure outcomes
💡 Master This: Ejection fraction measures pump function but not contractility. A patient with severe mitral regurgitation may have EF 65% but poor contractility due to reduced afterload. True contractility requires load-independent measures like end-systolic elastance.
Heart Rate Optimization: The Chronotropic Response
Heart rate determines cardiac output through rate-dependent mechanisms:
-
Rate-Related Physiology
- Optimal heart rate: 60-100 bpm at rest
- Maximum heart rate: 220 - age during exercise
- Diastolic filling time: Inversely related to heart rate
- At HR 60: Diastole 667 ms, filling adequate
- At HR 150: Diastole 200 ms, filling compromised
- Tachycardia >120 reduces stroke volume
-
Rate Control Strategies
- Beta-blockers: Reduce HR by 15-25%, improve diastolic filling
- Calcium channel blockers: Rate control in atrial fibrillation
- Pacing: Optimize AV synchrony, 20-25% improvement in cardiac output
- Dual-chamber pacing preserves atrial kick
- Biventricular pacing improves synchrony in heart failure
⚠️ Warning: In hypertrophic cardiomyopathy, tachycardia reduces diastolic filling time and increases outflow obstruction. Beta-blockers are first-line therapy to slow heart rate and improve ventricular filling.

Understanding these hemodynamic mechanisms enables prediction of cardiovascular responses to pathological states. Connect these functional principles through clinical pattern recognition to master diagnostic approaches.
⚡ The Hemodynamic Powerhouse: Cardiac Function Mechanisms
🎯 The Diagnostic Arsenal: Pattern Recognition Mastery
ECG Pattern Recognition: The Electrical Roadmap
- ST-Elevation Patterns
-
Anterior STEMI: ST elevation in V1-V4
- LAD occlusion - largest territory at risk
- Q waves develop within 6-12 hours
- Reciprocal depression in inferior leads
- Cardiogenic shock risk: 15-20%
-
Inferior STEMI: ST elevation in II, III, aVF
- RCA occlusion in 85% of cases
- Heart block develops in 40%
- Right ventricular involvement: ST elevation in V4R
- Hypotension responds to IV fluids, not vasopressors
-
Lateral STEMI: ST elevation in I, aVL, V5-V6
- Circumflex occlusion - often "silent" presentation
- Posterior extension: Tall R waves in V1-V2
- Mitral regurgitation risk from papillary muscle ischemia
-
📌 Remember: "LIMA" for Lateral leads (I, aVL, V5-V6), Inferior leads (II, III, aVF), Middle leads (V3-V4), Anterior leads (V1-V2). Each pattern predicts specific complications and management strategies.
Chest Pain Diagnostic Framework
| Feature | Typical Angina | Atypical Angina | Non-cardiac | Diagnostic Accuracy |
|---|---|---|---|---|
| Substernal location | 95% | 60% | 20% | High specificity |
| Exertional trigger | 90% | 40% | 10% | Moderate sensitivity |
| Relief with rest/nitro | 85% | 30% | 5% | High specificity |
| Duration 2-10 minutes | 80% | 50% | 30% | Moderate specificity |
| Radiation to arm/jaw | 70% | 35% | 15% | Moderate specificity |
- Age >65 with any chest pain: CAD risk 85%
- Diabetes + chest pain: Silent ischemia in 60%
- Prior MI + recurrent pain: Unstable angina in 75%
- TIMI risk score >3: 14-day mortality 5%
- GRACE score >140: Hospital mortality 3%
⭐ Clinical Pearl: Atypical presentations occur in 60% of women, 50% of diabetics, and 70% of elderly patients. Absence of classic chest pain does NOT exclude ACS. Focus on risk factors + ECG changes + biomarkers for diagnosis.

Heart Failure Recognition Patterns
-
Systolic Heart Failure (HFrEF)
- Ejection fraction <40%
- S3 gallop - pathognomonic finding
- Displaced PMI - lateral and inferior displacement
- BNP >400 pg/mL or NT-proBNP >1800 pg/mL
- Chest X-ray: Cardiomegaly, pulmonary edema
- Echo: Global hypokinesis, dilated chambers
-
Diastolic Heart Failure (HFpEF)
- Ejection fraction >50%
- S4 gallop - atrial kick against stiff ventricle
- Normal-sized heart with thick walls
- E/e' ratio >15 on echo Doppler
- Left atrial enlargement from elevated pressures
- Pulmonary hypertension in 60% of cases
💡 Master This: BNP levels correlate with filling pressures, not ejection fraction. A patient with HFpEF can have BNP >1000 pg/mL despite normal EF. Use BNP to assess hemodynamic status, not systolic function.
Murmur Diagnostic Algorithms
-
Systolic Murmur Grading
- Grade 1/6: Barely audible, requires concentration
- Grade 2/6: Soft but easily heard
- Grade 3/6: Moderate intensity, no thrill
- Grade 4/6: Loud with palpable thrill
- Grade 5/6: Very loud, heard with stethoscope barely on chest
- Grade 6/6: Heard without stethoscope
-
Dynamic Maneuvers
- Valsalva: Decreases preload
- HOCM murmur increases (less filling, more obstruction)
- Most other murmurs decrease (less venous return)
- Handgrip: Increases afterload
- Mitral regurgitation increases (higher pressure gradient)
- Aortic stenosis decreases (reduced stroke volume)
- Valsalva: Decreases preload
⚠️ Warning: All diastolic murmurs are pathologic and require echocardiography. Grade 3/6 or higher systolic murmurs in adults warrant cardiac evaluation. New murmurs in elderly patients suggest structural heart disease.
Understanding these diagnostic patterns creates systematic approaches to cardiovascular evaluation. Connect these recognition frameworks through hemodynamic analysis to master treatment selection strategies.
🎯 The Diagnostic Arsenal: Pattern Recognition Mastery
🔬 The Pathophysiology Matrix: Disease Mechanism Analysis
Atherosclerosis: The Arterial Siege
- Plaque Development Stages
-
Fatty Streak (Age 10-20)
- Foam cell accumulation in intimal layer
- No luminal narrowing or clinical symptoms
- Reversible with risk factor modification
- Present in 100% of population by age 20
-
Intermediate Lesion (Age 20-40)
- Smooth muscle cell migration and proliferation
- Extracellular lipid pools develop
- <50% stenosis, typically asymptomatic
- Positive remodeling maintains luminal diameter
-
Advanced Plaque (Age 40+)
- Fibrous cap formation over lipid core
- >50% stenosis causes flow limitation
- Vulnerable plaques: Thin cap (<65 μm), large lipid core
- Plaque rupture triggers 75% of acute coronary syndromes
-
📌 Remember: "PLAQUE" - Platelet adhesion, Lipid accumulation, Arterial remodeling, Quiescent (stable) vs Unstable, Endothelial dysfunction. Vulnerable plaques cause more events than severely stenotic stable lesions.
Myocardial Infarction: The Cellular Catastrophe
| Time Post-MI | Microscopic Changes | Gross Changes | Complications | Clinical Markers |
|---|---|---|---|---|
| 0-6 hours | Normal histology | No visible changes | Arrhythmias | Troponin rise |
| 6-24 hours | Coagulation necrosis | Pallor, edema | Pump failure | Peak CK-MB |
| 1-3 days | Neutrophil infiltration | Yellow softening | Free wall rupture | Fever, leukocytosis |
| 3-7 days | Macrophage invasion | Red-brown | Papillary muscle rupture | ESR elevation |
| 1-3 weeks | Granulation tissue | Hyperemic border | Ventricular aneurysm | Pericarditis |
| >6 weeks | Collagen scar | White, firm | Dressler syndrome | Stable scar |
- Calcium overload: Mitochondrial dysfunction
- Oxygen free radicals: Membrane lipid peroxidation
- Neutrophil activation: Microvascular plugging
- No-reflow phenomenon in 5-15% of patients
- Myocardial stunning: Reversible dysfunction
- Hibernating myocardium: Chronic hypoperfusion
⭐ Clinical Pearl: Mechanical complications peak at 3-7 days post-MI when necrotic tissue is softest. Free wall rupture (day 3-5), papillary muscle rupture (day 3-7), and ventricular septal defect (day 3-7) require immediate surgical intervention.
Heart Failure: The Compensatory Cascade
-
Neurohormonal Activation
-
Sympathetic Nervous System
- Norepinephrine levels increase 2-5 fold
- β1-receptor downregulation by 50-60%
- Arrhythmia risk increases 3-4 fold
- Sudden death accounts for 40% of HF mortality
-
Renin-Angiotensin-Aldosterone System
- Angiotensin II increases 3-10 fold
- Aldosterone increases 5-20 fold
- Sodium retention leads to volume overload
- Potassium loss increases arrhythmia risk
-
-
Ventricular Remodeling
- Eccentric hypertrophy: Volume overload pattern
- Concentric hypertrophy: Pressure overload pattern
- Myocyte apoptosis: 1-2% annual cell loss
- Fibroblast proliferation replaces myocytes
- Collagen deposition increases wall stiffness
- Capillary density decreases relative to muscle mass
💡 Master This: ACE inhibitors and ARBs block maladaptive remodeling, not just symptoms. Mortality benefit comes from preventing progressive ventricular dysfunction, explaining why these drugs improve survival even in asymptomatic patients with reduced EF.
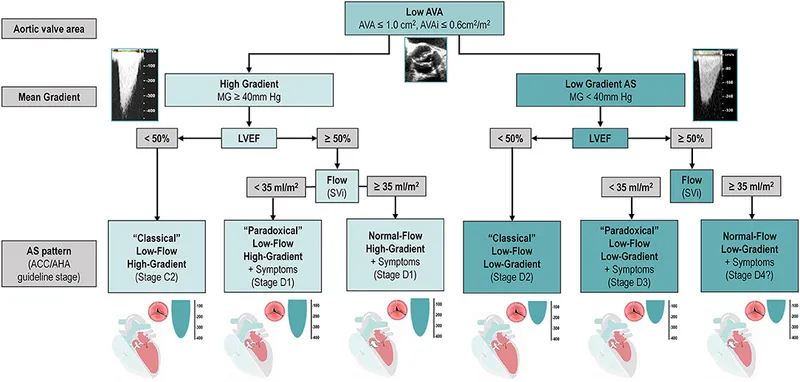
Valvular Disease: The Hemodynamic Consequences
-
Aortic Stenosis Progression
- Mild AS: Valve area >1.5 cm², gradient <25 mmHg
- Moderate AS: Valve area 1.0-1.5 cm², gradient 25-40 mmHg
- Severe AS: Valve area <1.0 cm², gradient >40 mmHg
- Pressure overload causes concentric LVH
- Diastolic dysfunction develops before systolic dysfunction
- Sudden death risk 1-2% annually in asymptomatic patients
-
Mitral Regurgitation Pathophysiology
- Acute MR: Normal-sized LA, rapid pressure rise
- Chronic MR: Dilated LA, volume accommodation
- Effective regurgitant orifice: Severe if >40 mm²
- Regurgitant volume: Severe if >60 mL
- Regurgitant fraction: Severe if >50%
- Pulmonary hypertension develops in chronic severe MR
⚠️ Warning: In acute severe MR, normal EF may represent underlying LV dysfunction due to reduced afterload from regurgitation. EF <60% in acute MR suggests impaired contractility and poor surgical outcomes.
Understanding these pathophysiological mechanisms enables prediction of disease progression and treatment responses. Connect these mechanistic insights through evidence-based treatment algorithms to master therapeutic decision-making.
🔬 The Pathophysiology Matrix: Disease Mechanism Analysis
🎯 The Treatment Command Center: Evidence-Based Therapeutic Algorithms
Acute Coronary Syndrome: The Emergency Protocol
-
STEMI Management Timeline
- Door-to-balloon time: <90 minutes for primary PCI
- Door-to-needle time: <30 minutes for thrombolysis
- Symptom-to-balloon time: <120 minutes optimal
- Mortality reduction: 25% with timely reperfusion
- Cardiogenic shock: 7% incidence, 50% mortality
- Mechanical complications: <1% with early reperfusion
-
Antiplatelet Therapy Protocols
- Aspirin: 325 mg loading, then 81 mg daily
- Clopidogrel: 600 mg loading, then 75 mg daily
- Ticagrelor: 180 mg loading, then 90 mg BID
- PLATO trial: 16% mortality reduction vs clopidogrel
- Bleeding risk: Major bleeding 2.8% annually
- Duration: 12 months minimum post-ACS
📌 Remember: "MONA-B" for Morphine, Oxygen (if hypoxic), Nitroglycerin, Aspirin, Beta-blocker. Add ACE inhibitor and statin within 24 hours for secondary prevention.
Heart Failure: The Guideline-Directed Arsenal
| Drug Class | Mechanism | Mortality Benefit | Dosing Strategy | Monitoring Parameters |
|---|---|---|---|---|
| ACE Inhibitors | RAAS blockade | 20-25% reduction | Target max tolerated | Creatinine, potassium |
| Beta-blockers | Sympathetic blockade | 30-35% reduction | Start low, titrate slow | Heart rate, blood pressure |
| Aldosterone Antagonists | Mineralocorticoid blockade | 15-20% reduction | Monitor potassium closely | Potassium, creatinine |
| SGLT2 Inhibitors | Glucose/sodium cotransporter | 13-18% reduction | Independent of diabetes | Volume status, GFR |
| ARNI | Dual RAAS/NEP inhibition | 16% vs ACE inhibitor | Replace ACE inhibitor | Angioedema risk |
- Loop diuretics: First-line for volume overload
- Furosemide: 40-80 mg daily, titrate to dry weight
- Thiazides: Add for synergistic effect in diuretic resistance
- Sequential nephron blockade: Furosemide + HCTZ
- Potassium-sparing: Spironolactone for RAAS blockade
- Daily weights: >2 kg gain in 48 hours indicates decompensation
⭐ Clinical Pearl: SGLT2 inhibitors provide cardiovascular benefit independent of diabetes status. Empagliflozin and dapagliflozin reduce heart failure hospitalizations by 30% and cardiovascular death by 15% in HFrEF patients regardless of baseline glucose.
Hypertension: The Stepped-Care Approach
-
Blood Pressure Targets
- General population: <130/80 mmHg
- Diabetes/CKD: <130/80 mmHg
- Age >65: <130/80 mmHg if tolerated
- SPRINT trial: <120 mmHg systolic reduces CV events 25%
- Intensive control: NNT = 61 to prevent 1 CV event
- Hypotension risk: Syncope 2.4% vs 1.7% standard care
-
First-Line Combinations
- ACE inhibitor + Thiazide: Lisinopril 10 mg + HCTZ 12.5 mg
- ARB + Calcium channel blocker: Losartan 50 mg + Amlodipine 5 mg
- Triple therapy: Add chlorthalidone 25 mg for resistant hypertension
- Single-pill combinations: Improve adherence by 25%
- Resistant hypertension: >3 drugs including diuretic
- Secondary causes: Evaluate if <30 years or sudden onset
Atrial Fibrillation: The Rhythm and Rate Strategy
-
CHA₂DS₂-VASc Scoring
- Congestive heart failure: 1 point
- Hypertension: 1 point
- Age ≥75: 2 points
- Diabetes: 1 point
- Stroke/TIA: 2 points
- Vascular disease: 1 point
- Age 65-74: 1 point
- Sex (female): 1 point
- Score ≥2: Anticoagulation recommended
- Score 1: Consider anticoagulation
- Annual stroke risk: Score 2 = 2.2%, Score 6 = 9.8%
-
Anticoagulation Options
- Warfarin: INR 2.0-3.0, monthly monitoring
- Apixaban: 5 mg BID, no monitoring required
- Rivaroxaban: 20 mg daily, with evening meal
- DOACs: 50% reduction in intracranial hemorrhage
- Major bleeding: 2-3% annually with any anticoagulant
- Reversal agents: Idarucizumab for dabigatran, andexanet alfa for Xa inhibitors
💡 Master This: Rate control is non-inferior to rhythm control for long-term outcomes in most AF patients. AFFIRM trial showed no mortality difference, but rhythm control may benefit younger patients with symptomatic AF and minimal comorbidities.
⚠️ Warning: Never cardiovert atrial fibrillation of >48 hours duration without adequate anticoagulation or negative TEE. Stroke risk is 5-7% within 24 hours of cardioversion without proper anticoagulation.
Understanding these evidence-based treatment algorithms enables systematic therapeutic decision-making. Connect these protocol-driven approaches through advanced integration concepts to master complex cardiovascular care.
🎯 The Treatment Command Center: Evidence-Based Therapeutic Algorithms
🧠 The Integration Matrix: Advanced Cardiovascular Synthesis
Cardio-Renal Syndrome: The Bidirectional Crisis
-
Type 1 (Acute Cardio-Renal)
- Acute heart failure → Acute kidney injury
- Mechanism: Reduced renal perfusion + venous congestion
- Incidence: 25-30% of acute HF admissions
- Creatinine rise >0.3 mg/dL within 48 hours
- Mortality increase: 2-3 fold with AKI
- Length of stay: +3-5 days average
-
Type 2 (Chronic Cardio-Renal)
- Chronic heart failure → Progressive CKD
- GFR decline: 2-4 mL/min/1.73m² annually
- Shared risk factors: Diabetes, hypertension, aging
- RAAS activation: Promotes both cardiac and renal fibrosis
- Mineral metabolism: Phosphorus >4.5 mg/dL increases CV mortality
- Anemia: Hgb <12 g/dL worsens HF outcomes
📌 Remember: "RIFLE" criteria for AKI - Risk (Cr ↑1.5x), Injury (Cr ↑2x), Failure (Cr ↑3x), Loss (>4 weeks), End-stage (>3 months). Each stage doubles mortality risk in HF patients.
Diabetes-Cardiovascular Nexus: The Metabolic Connection
| Diabetic Complication | CV Risk Multiplier | Mechanism | Therapeutic Target | Outcome Benefit |
|---|---|---|---|---|
| Microalbuminuria | 2-3x | Endothelial dysfunction | ACE inhibitor/ARB | 25% CV risk reduction |
| Diabetic nephropathy | 4-5x | Accelerated atherosclerosis | SGLT2 inhibitor | 35% HF hospitalization ↓ |
| Autonomic neuropathy | 3-4x | Silent ischemia | Beta-blocker | 30% sudden death ↓ |
| Retinopathy | 2-3x | Microvascular disease | Intensive glucose control | 15% macrovascular events ↓ |
| Poor glycemic control | 1.5-2x | Glycation, inflammation | HbA1c <7% | 10% major CV events ↓ |
- Empagliflozin: 14% CV death reduction in EMPA-REG
- Canagliflozin: 14% CV death reduction in CANVAS
- Dapagliflozin: 17% CV death reduction in DECLARE
- Mechanism: Volume reduction, BP ↓3-5 mmHg
- Weight loss: 2-3 kg average
- HF benefit: Independent of diabetes status
⭐ Clinical Pearl: GLP-1 agonists provide CV protection beyond glucose control. Liraglutide reduces CV death by 22% and semaglutide by 26% through weight loss, BP reduction, and anti-inflammatory effects.
Cardio-Oncology: The Emerging Frontier
-
Anthracycline Cardiotoxicity
- Doxorubicin: Dose-dependent cardiomyopathy
- Cumulative dose >250 mg/m²: 5% HF risk
- Cumulative dose >550 mg/m²: 26% HF risk
- Type I: Irreversible myocyte damage
- Mechanism: Free radical generation, mitochondrial dysfunction
- Prevention: Dexrazoxane chelation therapy
-
Trastuzumab Cardiotoxicity
- Type II: Reversible dysfunction
- Incidence: 2-7% when used alone
- With anthracyclines: 27% HF risk
- Mechanism: HER2 receptor blockade in cardiomyocytes
- Recovery: >50% improve with HF therapy
- Monitoring: Echo every 3 months during therapy
Perioperative Cardiovascular Risk: The Surgical Challenge
-
Revised Cardiac Risk Index (RCRI)
- High-risk surgery: 1 point
- Ischemic heart disease: 1 point
- Heart failure: 1 point
- Cerebrovascular disease: 1 point
- Diabetes on insulin: 1 point
- Creatinine >2.0 mg/dL: 1 point
- 0 points: 0.4% cardiac event rate
- 1 point: 1.0% cardiac event rate
- 2 points: 2.4% cardiac event rate
- ≥3 points: 5.4% cardiac event rate
-
Perioperative Beta-Blockade
- Continue existing beta-blockers
- Avoid new beta-blockers in low-risk patients
- Consider in high-risk patients with careful titration
- POISE trial: Metoprolol reduced MI but increased stroke
- Target heart rate: 60-70 bpm perioperatively
- Hypotension risk: Monitor closely first 48 hours
💡 Master This: Statins provide pleiotropic benefits beyond cholesterol lowering. Perioperative statin therapy reduces cardiac events by 30% through plaque stabilization, anti-inflammatory effects, and endothelial protection. Continue statins throughout perioperative period.
⚠️ Warning: Perioperative MI often presents without chest pain in 60-70% of cases. Monitor troponins and ECGs in high-risk patients for 48-72 hours postoperatively, as silent MI carries similar mortality risk.

Understanding these integration principles enables comprehensive cardiovascular care across multiple specialties and clinical scenarios. Connect these advanced concepts through rapid mastery frameworks to achieve clinical excellence.
🧠 The Integration Matrix: Advanced Cardiovascular Synthesis
🏆 The Mastery Toolkit: Rapid Clinical Excellence Framework

The Essential Numbers Arsenal
📌 Hemodynamic Thresholds: MAP >65 (organ perfusion), CVP 8-12 (optimal preload), PCWP >18 (pulmonary edema), CI <2.2 (cardiogenic shock), SVR >1200 (afterload excess)
⭐ Cardiac Biomarkers: Troponin I >0.04 ng/mL (myocardial injury), BNP >400 pg/mL (heart failure), CK-MB >25 ng/mL (large MI), D-dimer >500 ng/mL (thrombosis risk)
💡 ECG Intervals: PR >200 ms (AV block), QRS >120 ms (conduction delay), QTc >450 ms (arrhythmia risk), ST elevation >1 mm (STEMI criteria)
Rapid Assessment Protocols
| Clinical Scenario | Key Assessment | Critical Threshold | Immediate Action | Time Target |
|---|---|---|---|---|
| Chest Pain | ECG + Troponin | ST elevation >1 mm | Activate cath lab | <10 minutes |
| Dyspnea | BNP + Echo | BNP >400 pg/mL | Diuresis + afterload reduction | <30 minutes |
| Syncope | ECG + Orthostatics | QTc >500 ms | Telemetry monitoring | <15 minutes |
| Shock | Echo + Lactate | CI <2.2 L/min/m² | Inotropes + mechanical support | <60 minutes |
| Palpitations | Rhythm strip | HR >150 bpm | Rate control vs cardioversion | <20 minutes |
📌 Remember: "CRASH CART" - Chest pain (ACS protocol), Rhythm disturbance (ACLS), Acute dyspnea (HF protocol), Shock (hemodynamic support), Hypertensive crisis (BP control), Cardiac arrest (CPR), Arrhythmia (rate/rhythm), Right heart failure (PE protocol), Tamponade (pericardiocentesis)
Drug Dosing Quick Reference
-
Emergency Medications
- Adenosine: 6 mg IV push, then 12 mg if needed
- Amiodarone: 150 mg IV over 10 minutes, then 1 mg/min
- Metoprolol: 25 mg BID, titrate to HR 60-70
- Furosemide: 40 mg IV, double dose if no response in 2 hours
- Nitroglycerin: 0.4 mg SL, repeat q5 minutes × 3
-
Chronic Therapy Targets
- ACE inhibitor: Titrate to maximum tolerated dose
- Beta-blocker: Target HR 60-70 bpm
- Statin: LDL <70 mg/dL (high risk), <100 mg/dL (moderate risk)
- Antiplatelet: Aspirin 81 mg + P2Y12 inhibitor × 12 months
⚠️ Critical Contraindications: Beta-blockers in acute cocaine toxicity, ACE inhibitors in bilateral renal artery stenosis, Nitrates with phosphodiesterase inhibitors, Calcium channel blockers in heart failure with reduced EF
Pattern Recognition Mastery Drills
💡 Master This: Wide QRS tachycardia = VT until proven otherwise. AV dissociation, capture beats, and fusion beats confirm VT. Never use verapamil for wide complex tachycardia.
⭐ Clinical Pearl: Diastolic murmur = Always pathologic. Austin Flint murmur (functional MS from severe AR), Graham Steell murmur (PR from pulmonary hypertension). All diastolic murmurs require echocardiography.
📌 High-Yield Correlation: Pulsus paradoxus >20 mmHg suggests cardiac tamponade. Beck's triad (elevated JVP, hypotension, muffled heart sounds) present in <10% of cases. Echo shows ventricular interdependence.
This mastery toolkit provides immediate clinical decision support for cardiovascular emergencies and routine care. Regular practice with these frameworks develops pattern recognition expertise and confident clinical performance across all cardiovascular scenarios.
🏆 The Mastery Toolkit: Rapid Clinical Excellence Framework
Practice Questions: Cardiovascular
Test your understanding with these related questions
A 58-year-old man comes to the emergency department for complaints of crushing chest pain for 4 hours. He was shoveling snow outside when the pain started. It is rated 7/10 and radiates to his left arm. An electrocardiogram (ECG) demonstrates ST-segment elevation in leads V2-4. He subsequently undergoes percutaneous coronary intervention (PCI) and is discharged with aspirin, clopidogrel, carvedilol, atorvastatin, and lisinopril. Five days later, the patient is brought to the emergency department by his wife with complaints of dizziness. He reports lightheadedness and palpitations for the past 2 hours but otherwise feels fine. His temperature is 99.7°F (37.6°C), blood pressure is 95/55 mmHg, pulse is 105/min, and respirations are 17/min. A pulmonary artery catheter is performed and demonstrates an increase in oxygen concentration at the pulmonary artery. What finding would you expect in this patient?













