Ventricular filling dynamics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ventricular filling dynamics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ventricular filling dynamics US Medical PG Question 1: A 73-year-old man presents to your clinic for a routine checkup. His medical history is notable for a previous myocardial infarction. He states that he has not seen a doctor in "many years". He has no complaints. When you auscultate over the cardiac apex with the bell of your stethoscope, you notice an additional sound immediately preceding S1. This extra heart sound is most likely indicative of which of the following processes?
- A. Decreased left ventricular compliance (Correct Answer)
- B. Increased left ventricular compliance
- C. Increased pulmonary compliance
- D. Decreased left ventricular filling volume
- E. Increased left ventricular filling volume
Ventricular filling dynamics Explanation: ***Decreased left ventricular compliance***
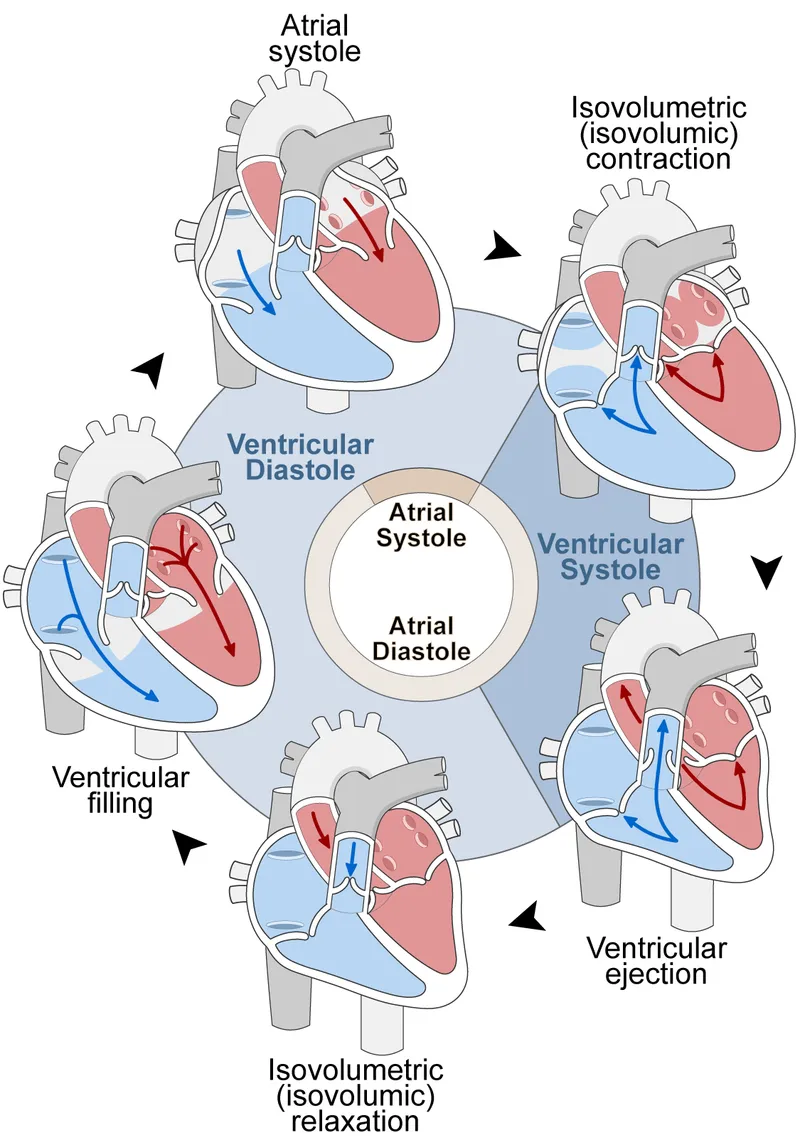
- An additional sound immediately preceding S1 suggests a **fourth heart sound (S4)**, which occurs during **atrial contraction** against a stiff, non-compliant ventricle.
- A myocardial infarction can lead to left ventricular hypertrophy and **fibrosis**, causing **decreased left ventricular compliance**.
*Increased left ventricular compliance*
- **Increased ventricular compliance** would allow for easier filling and would not generate an audible S4.
- This condition is typically seen in dilated ventricles, which accommodate larger volumes **without significant pressure increases**.
*Increased pulmonary compliance*
- **Pulmonary compliance** refers to the lungs' ability to stretch and expand, and it is unrelated to an additional heart sound preceding S1.
- This concept describes the **elastic properties of lung tissue** and has no direct bearing on cardiac auscultation in this context.
*Decreased left ventricular filling volume*
- A **decreased left ventricular filling volume** might reduce the intensity of heart sounds but would not, in itself, cause an S4 before S1.
- S4 is related to the **atrial kick** into a resistant ventricle, not the overall volume available for filling.
*Increased left ventricular filling volume*
- While increased filling volume can occur in conditions like **valvular regurgitation**, it does not directly lead to an S4.
- An S4 is specifically due to a forceful atrial contraction against a **non-compliant ventricle**, regardless of the absolute filling volume.
Ventricular filling dynamics US Medical PG Question 2: A 49-year-old man presents to his physician complaining of weakness and fatigue. On exam, you note significant peripheral edema. Transthoracic echocardiogram is performed and reveals a preserved ejection fraction with impaired diastolic relaxation. A representative still image is shown in Image A. Which of the following is likely the cause of this patient's symptoms?
- A. Hemochromatosis (Correct Answer)
- B. Heavy, long-term alcohol consumption
- C. History of myocardial infarction
- D. History of a recent viral infection
- E. Previous treatment with doxorubicin
Ventricular filling dynamics Explanation: ***Hemochromatosis***
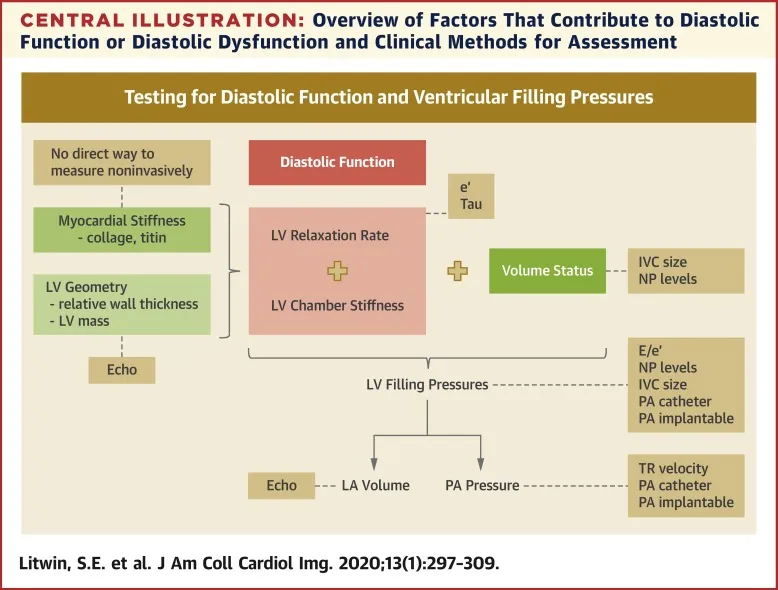
- **Hemochromatosis** can lead to **restrictive cardiomyopathy** due to iron deposition in the myocardium, causing **diastolic dysfunction** with a **preserved ejection fraction**.
- The symptoms of **weakness**, **fatigue**, and **peripheral edema** are consistent with **heart failure** secondary to this cardiac impairment.
*Heavy, long-term alcohol consumption*
- **Alcoholic cardiomyopathy** typically presents as **dilated cardiomyopathy**, characterized by **systolic dysfunction** and a **reduced ejection fraction**, which contradicts the preserved ejection fraction seen in this patient.
- While chronic alcohol use can cause heart failure symptoms, the specific echocardiographic findings do not align with this etiology.
*History of myocardial infarction*
- A **myocardial infarction** commonly leads to **systolic dysfunction** or **ischemic cardiomyopathy**, resulting in a **reduced ejection fraction** due to scar tissue formation and impaired contractility.
- The patient's preserved ejection fraction and primary diastolic relaxation abnormality make this diagnosis less likely.
*History of a recent viral infection*
- A recent viral infection can cause **viral myocarditis**, which typically leads to **dilated cardiomyopathy** and **systolic dysfunction** with a **reduced ejection fraction**.
- The observed preserved ejection fraction and isolated diastolic relaxation impairment are not characteristic features of acute viral myocarditis.
*Previous treatment with doxorubicin*
- **Doxorubicin** (an anthracycline) is a well-known cardiotoxic agent that causes **dilated cardiomyopathy** with a **reduced ejection fraction**, primarily affecting **systolic function**.
- The patient's preserved ejection fraction makes doxorubicin-induced cardiotoxicity an unlikely cause of his current presentation.
Ventricular filling dynamics US Medical PG Question 3: An 83-year-old male presents with dyspnea, orthopnea, and a chest radiograph demonstrating pulmonary edema. A diagnosis of congestive heart failure is considered. The following clinical measurements are obtained: 100 bpm heart rate, 0.2 mL O2/mL systemic blood arterial oxygen content, 0.1 mL O2/mL pulmonary arterial oxygen content, and 400 mL O2/min oxygen consumption. Using the above information, which of the following values represents this patient's cardiac stroke volume?
- A. 30 mL/beat
- B. 70 mL/beat
- C. 40 mL/beat (Correct Answer)
- D. 60 mL/beat
- E. 50 mL/beat
Ventricular filling dynamics Explanation: ***40 mL/beat***
- First, calculate cardiac output (CO) using the **Fick principle**: CO = Oxygen Consumption / (Arterial O2 content - Venous O2 content). Here, CO = 400 mL O2/min / (0.2 mL O2/mL - 0.1 mL O2/mL) = 400 mL O2/min / 0.1 mL O2/mL = **4000 mL/min**.
- Next, calculate stroke volume (SV) using the formula: SV = CO / Heart Rate. Given a heart rate of 100 bpm, SV = 4000 mL/min / 100 beats/min = **40 mL/beat**.
*30 mL/beat*
- This answer would result if there was an error in calculating either the **cardiac output** or if the **arteriovenous oxygen difference** was overestimated.
- A stroke volume of 30 mL/beat with a heart rate of 100 bpm would yield a cardiac output of 3 L/min, which is sub-physiologic for an oxygen consumption of 400 mL/min given the provided oxygen content values.
*70 mL/beat*
- This stroke volume is higher than calculated and would imply either a significantly **lower heart rate** or a much **higher cardiac output** than derived from the Fick principle with the given values.
- A stroke volume of 70 mL/beat at a heart rate of 100 bpm would mean a cardiac output of 7 L/min, which is inconsistent with the provided oxygen consumption and arteriovenous oxygen difference.
*60 mL/beat*
- This value is higher than the correct calculation, suggesting an error in the initial calculation of **cardiac output** or the **avO2 difference**.
- To get 60 mL/beat, the cardiac output would need to be 6000 mL/min, which would mean an avO2 difference of 0.067 mL O2/mL, not 0.1 mL O2/mL.
*50 mL/beat*
- This stroke volume would result from an incorrect calculation of the **cardiac output**, potentially from a slight miscalculation of the **arteriovenous oxygen difference**.
- A stroke volume of 50 mL/beat at 100 bpm would mean a cardiac output of 5 L/min, requiring an avO2 difference of 0.08 mL O2/mL, which is not consistent with the given values.
Ventricular filling dynamics US Medical PG Question 4: A 72-year-old woman comes to the emergency department because of a 2-week history of worsening shortness of breath, lower extremity swelling, and a 3-kg (6.6-lb) weight gain. Crackles are heard on auscultation of the chest. Cardiac examination shows a dull, low-pitched early diastolic sound at the 5th left intercostal space that becomes louder in the left lateral decubitus position at end-expiration. Which of the following is the most likely cause of these auscultation findings?
- A. Increased ventricular contractility
- B. Increased capacity of the pulmonary circulation
- C. Decreased left-ventricular filling pressure
- D. Increased left ventricular end-systolic volume
- E. Decreased left myocardial compliance (Correct Answer)
Ventricular filling dynamics Explanation: ***Decreased left myocardial compliance***
- A dull, low-pitched early **diastolic sound (S3 gallop)**, heard best in the left lateral decubitus position at end-expiration, indicates **rapid ventricular filling** into a ventricle with altered diastolic properties. This finding, along with worsening shortness of breath, lower extremity swelling, and weight gain, suggests **heart failure with impaired ventricular filling**.
- Decreased left myocardial compliance (increased stiffness) means the left ventricle cannot **relax and fill properly** during diastole. The S3 occurs when blood rapidly decelerates as it enters the stiff, non-compliant ventricle, creating the characteristic sound.
- This represents **diastolic dysfunction** (heart failure with preserved ejection fraction - HFpEF), which is common in elderly patients with hypertension and is characterized by a stiff ventricle with increased filling pressures.
*Increased ventricular contractility*
- Increased ventricular contractility would lead to a more forceful ejection of blood during systole, not an early diastolic filling sound.
- This would not explain the S3 gallop or the signs of heart failure with fluid retention.
*Increased capacity of the pulmonary circulation*
- Increased pulmonary circulation capacity would help accommodate fluid and prevent pulmonary congestion, which contradicts the symptoms of crackles and shortness of breath.
- The patient has **decreased** capacity to handle the fluid volume, leading to pulmonary edema.
*Decreased left-ventricular filling pressure*
- Decreased LV filling pressure would imply less fluid overload and better cardiac function, contrary to the clinical presentation.
- An S3 gallop and signs of heart failure (crackles, edema, weight gain) indicate **increased** filling pressures from impaired ventricular function.
*Increased left ventricular end-systolic volume*
- Increased end-systolic volume indicates **systolic dysfunction** (reduced ejection fraction), where the ventricle cannot adequately eject blood, leaving residual volume after contraction.
- While systolic dysfunction can also produce an S3 gallop due to volume overload, the specific clinical description emphasizes a **diastolic filling abnormality** (sound during early diastole in a specific position that optimizes detection of ventricular filling).
- The S3 in systolic dysfunction is primarily due to **volume overload**, whereas the S3 here is attributed to blood entering a **stiff ventricle** with impaired compliance, which is the primary pathophysiologic mechanism being tested.
Ventricular filling dynamics US Medical PG Question 5: A 32-year-old woman comes to the physician for a screening health examination that is required for scuba diving certification. The physician asks her to perform a breathing technique: following deep inspiration, she is instructed to forcefully exhale against a closed airway and contract her abdominal muscles while different cardiovascular parameters are evaluated. Which of the following effects is most likely after 10 seconds in this position?
- A. Decreased intra-abdominal pressure
- B. Decreased left ventricular stroke volume (Correct Answer)
- C. Decreased pulse rate
- D. Decreased systemic vascular resistance
- E. Increased venous return to left atrium
Ventricular filling dynamics Explanation: ***Decreased left ventricular stroke volume***
- After 10 seconds of performing the **Valsalva maneuver**, the increased intrathoracic pressure significantly reduces **venous return** to the heart.
- Reduced venous return leads to decreased **ventricular filling** (preload), which in turn diminishes **left ventricular stroke volume** and cardiac output.
*Decreased intra-abdominal pressure*
- The instruction to "contract her abdominal muscles" during forceful exhalation against a closed airway (Valsalva maneuver) directly leads to an **increase** in **intra-abdominal pressure**, not a decrease.
- This increase in intra-abdominal pressure further impedes venous return from the lower extremities to the heart.
*Decreased pulse rate*
- In the initial phase of the Valsalva maneuver (first 5-10 seconds), the decrease in cardiac output triggers a **reflex tachycardia** to maintain blood pressure, leading to an **increased pulse rate**.
- A decrease in pulse rate (bradycardia) is more characteristic of the release phase, not during the sustained strain.
*Decreased systemic vascular resistance*
- During the Valsalva maneuver, the body attempts to compensate for the drop in cardiac output and blood pressure by increasing **sympathetic tone**, which causes **vasoconstriction** and thus **increases systemic vascular resistance**.
- A decrease in systemic vascular resistance would further drop blood pressure and is not the physiological response during this phase.
*Increased venous return to left atrium*
- The Valsalva maneuver dramatically **reduces venous return** to both the right and left atria due to the high intrathoracic pressure compressing the great veins.
- This decreased venous return is the primary mechanism leading to the subsequent fall in cardiac output during the maneuver.
Ventricular filling dynamics US Medical PG Question 6: A 59-year-old woman comes to the physician for a 3-month history of progressively worsening shortness of breath on exertion and swelling of her legs. She has a history of breast cancer, which was treated with surgery followed by therapy with doxorubicin and trastuzumab 4 years ago. Cardiac examination shows an S3 gallop; there are no murmurs or rubs. Examination of the lower extremities shows pitting edema below the knees. Echocardiography is most likely to show which of the following sets of changes in this patient?
$$$ Ventricular wall thickness %%% Ventricular cavity size %%% Diastolic function %%% Aorto-ventricular pressure gradient $$$
- A. ↓ ↑ normal normal (Correct Answer)
- B. Normal normal ↓ normal
- C. ↑ ↓ ↓ normal
- D. ↑ ↓ ↓ ↑
- E. ↓ ↑ ↓ normal
Ventricular filling dynamics Explanation: ***↓ ↑ normal normal***
- Doxorubicin is an **anthracycline** known to cause **dilated cardiomyopathy**, characterized by **decreased ventricular wall thickness**, **increased ventricular cavity size**, and **preserved diastolic function**.
- The S3 gallop and pitting edema indicate **heart failure with reduced ejection fraction (HFrEF)**, consistent with dilated cardiomyopathy.
*Normal normal ↓ normal*
- This option suggests a primary issue with **diastolic function**, which is not the typical presentation of doxorubicin-induced cardiomyopathy.
- While diastolic dysfunction can occur, doxorubicin characteristically causes **systolic dysfunction** manifesting as chamber dilation and wall thinning.
*↑ ↓ ↓ normal*
- This pattern of **increased wall thickness** and **decreased cavity size** is characteristic of **hypertrophic cardiomyopathy** or **restrictive cardiomyopathy**, which are generally not caused by doxorubicin.
- Doxorubicin typically causes **cardiac muscle fiber damage** leading to thinning and dilation.
*↑ ↓ ↓ ↑*
- This option also suggests **increased wall thickness** and **decreased cavity size**, inconsistent with doxorubicin's effects on the heart.
- The **elevated aorto-ventricular pressure gradient** might indicate outflow tract obstruction or significant aortic stenosis, which are not typical sequelae of doxorubicin.
*↓ ↑ ↓ normal*
- While doxorubicin leads to **decreased wall thickness** and **increased cavity size**, the diastolic function is usually preserved early on, not decreased.
- A decrease in diastolic function might occur in later stages, but the primary and most characteristic feature due to doxorubicin is **systolic dysfunction** and chamber remodeling.
Ventricular filling dynamics US Medical PG Question 7: A 21-year-old man presents to his physician for a routine checkup. His doctor asks him if he has had any particular concerns since his last visit and if he has taken any new medications. He says that he has not been ill over the past year, except for one episode of the flu. He has been training excessively for his intercollege football tournament, which is supposed to be a huge event. His blood pressure is 110/70 mm Hg, pulse is 69/min, and respirations are 17/min. He has a heart sound coinciding with the rapid filling of the ventricles and no murmurs. He does not have any other significant physical findings. Which of the following best describes the heart sound heard in this patient?
- A. Fourth heart sound (S4)
- B. Opening snap
- C. Third heart sound (S3) (Correct Answer)
- D. Second heart sound (S2)
- E. Mid-systolic click
Ventricular filling dynamics Explanation: ***Third heart sound (S3)***
- An **S3 heart sound** is a low-pitched sound heard during **rapid ventricular filling** in early diastole, immediately after S2.
- In young, healthy individuals, especially athletes, an S3 can be a normal physiological finding, representing rapid filling of a **compliant ventricle**.
*Fourth heart sound (S4)*
- An **S4 heart sound** occurs during **atrial contraction** against a stiff or non-compliant ventricle, just before S1.
- It is typically associated with conditions like **ventricular hypertrophy** or **ischemia** and is less likely to be a normal finding in a young, healthy individual.
*Opening snap*
- An **opening snap** is a high-pitched, crisp sound heard after S2, caused by the sudden opening of a **stenotic mitral** or **tricuspid valve**.
- It indicates valvular pathology, specifically **mitral stenosis**, and is not related to ventricular filling in a healthy heart.
*Second heart sound (S2)*
- The **S2 heart sound** represents the **closure of the aortic and pulmonary valves** at the end of ventricular systole.
- While it marks the beginning of diastole, it does not coincide with the rapid filling of the ventricles itself.
*Mid-systolic click*
- A **mid-systolic click** is typically associated with **mitral valve prolapse**, caused by the sudden tensing of the chordae tendineae or valve leaflets.
- It occurs during systole, not diastole, and is not related to ventricular filling.
Ventricular filling dynamics US Medical PG Question 8: A 73-year-old woman presents to clinic with a week of fatigue, headache, and swelling of her ankles bilaterally. She reports that she can no longer go on her daily walk around her neighborhood without stopping frequently to catch her breath. At night she gets short of breath and has found that she can only sleep well in her recliner. Her past medical history is significant for hypertension and a myocardial infarction three years ago for which she had a stent placed. She is currently on hydrochlorothiazide, aspirin, and clopidogrel. She smoked 1 pack per day for 30 years before quitting 10 years ago and socially drinks around 1 drink per month. She denies any illicit drug use. Her temperature is 99.0°F (37.2°C), pulse is 115/min, respirations are 18/min, and blood pressure is 108/78 mmHg. On physical exam there is marked elevations of her neck veins, bilateral pitting edema in the lower extremities, and a 3/6 holosystolic ejection murmur over the right sternal border. Echocardiography shows the following findings:
End systolic volume (ESV): 100 mL
End diastolic volume (EDV): 160 mL
How would cardiac output be determined in this patient?
- A. 108/3 + (2 * 78)/3
- B. (160 - 100) / 160
- C. 160 - 100
- D. (160 - 100) * 115 (Correct Answer)
- E. (100 - 160) * 115
Ventricular filling dynamics Explanation: ***(160 - 100) * 115***
- **Cardiac output (CO)** is calculated as **stroke volume (SV) multiplied by heart rate (HR)**.
- **Stroke volume** is determined by subtracting the **end-systolic volume (ESV)** from the **end-diastolic volume (EDV)** (SV = EDV - ESV).
*(108/3 + (2 * 78)/3)*
- This formula represents the calculation for **mean arterial pressure (MAP)**, which is not directly used to determine cardiac output.
- **MAP** is approximated as (Systolic BP + 2 * Diastolic BP) / 3.
*(160 - 100) / 160*
- This formula calculates the **ejection fraction (EF)**, which is the fraction of blood pumped out of the ventricle with each beat.
- While **ejection fraction** is a crucial measure of cardiac function, it does not directly determine cardiac output.
*160 - 100*
- This calculation represents the **stroke volume (SV)** (EDV - ESV), which is the amount of blood ejected from the ventricle per beat.
- However, to get the **cardiac output**, stroke volume must be multiplied by the heart rate.
*(100 – 160) * 115*
- This calculation would result in a **negative stroke volume**, which is physiologically incorrect as stroke volume must be a positive value.
- **Stroke volume** is always calculated as the **end-diastolic volume minus the end-systolic volume**.
Ventricular filling dynamics US Medical PG Question 9: A 36-year-old woman is admitted to the hospital for the evaluation of progressive breathlessness. She has no history of major medical illness. Her temperature is 37°C (98.6°F), pulse is 110/min, and respirations are 22/min. Pulse oximetry on room air shows an oxygen saturation of 99%. Cardiac examination shows a loud S1 and S2. There is a grade 2/6 early systolic murmur best heard in the 2nd right intercostal space. Cardiac catheterization shows a mixed venous oxygen saturation of 55% (N= 65–70%). Which of the following is the most likely cause of this patient's breathlessness?
- A. Increased peripheral shunting
- B. Decreased hemoglobin concentration
- C. Increased carbon dioxide retention
- D. Increased pulmonary vascular resistance
- E. Decreased left ventricular ejection fraction (Correct Answer)
Ventricular filling dynamics Explanation: ***Decreased left ventricular ejection fraction***
- The key finding is a **mixed venous oxygen saturation of 55% (normal 65-70%)** with **normal arterial oxygen saturation (99%)**, which indicates **increased tissue oxygen extraction**
- Increased oxygen extraction occurs when **cardiac output is reduced** → tissues must extract more oxygen from each pass of blood to meet metabolic demands
- This is the classic physiologic compensation in **heart failure with reduced ejection fraction**
- The cardiac findings (loud heart sounds, systolic murmur) suggest underlying cardiac pathology causing reduced cardiac output and progressive breathlessness
*Increased peripheral shunting*
- Peripheral shunting (e.g., arteriovenous malformations) would cause **venous blood to bypass capillary beds**, resulting in **decreased oxygen extraction** and **higher mixed venous O2 saturation**, not lower
- Would typically cause **hypoxemia** with reduced pulse oximetry, but this patient has 99% oxygen saturation
*Decreased hemoglobin concentration*
- Anemia reduces oxygen-carrying capacity but would not explain the **low mixed venous oxygen saturation** to this degree
- The **pulse oximetry of 99%** indicates adequate oxygen saturation of available hemoglobin
- Anemia typically causes **high cardiac output** (compensatory) rather than the low cardiac output state indicated by the low mixed venous O2 saturation
*Increased carbon dioxide retention*
- **Hypercapnia** results from **hypoventilation** and impaired gas exchange, typically causing **respiratory acidosis**
- Would present with altered mental status, drowsiness, or signs of respiratory failure
- Does not explain the **low mixed venous oxygen saturation** with normal arterial oxygen saturation
- The cardiac findings point to a primary cardiac rather than respiratory problem
*Increased pulmonary vascular resistance*
- **Pulmonary hypertension** causes **right ventricular dysfunction** and can present with breathlessness and a loud P2 component of S2
- However, isolated pulmonary hypertension would not cause the same degree of **systemic oxygen extraction** increase
- The low mixed venous O2 saturation indicates **reduced systemic cardiac output**, which primarily reflects **left ventricular dysfunction** rather than isolated right-sided pathology
Ventricular filling dynamics US Medical PG Question 10: A 72-year-old man with severe aortic regurgitation and compensated heart failure is being evaluated for surgical intervention. His echocardiogram shows LV end-diastolic dimension of 7.5 cm, ejection fraction of 45%, and severe aortic regurgitation with a regurgitant fraction of 60%. Pressure-volume loop analysis shows a markedly widened loop with increased stroke work. Evaluate the compensatory mechanisms maintaining his cardiac output and predict the timing for surgical intervention based on cardiac cycle mechanics.
- A. Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output
- B. Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction (Correct Answer)
- C. Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes
- D. Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship
- E. Surgery should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease
Ventricular filling dynamics Explanation: ***Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction***
- In chronic **aortic regurgitation**, the ventricle undergoes **eccentric hypertrophy** to accommodate large volumes, but this patient has reached critical **LV end-diastolic dimensions** (>7.0 cm), signaling the limits of compensation.
- An **ejection fraction (EF) of 45%** in the setting of severe AR is actually indicative of **systolic dysfunction**, as guidelines generally recommend intervention when EF falls below 50-55% due to the increased total stroke volume.
*Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output*
- Waiting for the **ejection fraction** to drop to 35% is dangerous; by this stage, the **myocardial damage** is often irreversible and postoperative outcomes are significantly poorer.
- A "maintained" cardiac output is deceptive here because the **total stroke work** is massive compared to the actual **forward flow**, leading to progressive heart failure.
*Surgery is should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease*
- **Asymptomatic patients** with severe AR require surgery if they meet specific **echocardiographic triggers** (like LV dimensions or EF) to prevent sudden death and permanent LV dysfunction.
- **Pressure-volume loop** analysis and chamber dimensions are highly predictive of the transition from a **compensated** to a **decompensated** state.
*Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes*
- While severe enlargement carries higher risk, an **LVEDD of 7.5 cm** is not a contraindication but rather an **urgent indication** for valve replacement to halt further decline.
- **Irreversible remodeling** is usually associated with even lower ejection fractions and severe **congestive heart failure** symptoms that do not respond to medical therapy.
*Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship*
- **Vasodilators** (like ACE inhibitors or CCBs) can reduce afterload and improve **forward flow**, but they do not stop the mechanical progression of **valvular regurgitation** or remodeling.
- **Surgical intervention** (AVR) is the only definitive treatment for severe chronic AR once the heart shows signs of **exhausted preload reserve** and declining contractility.
More Ventricular filling dynamics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.