Ventricular ejection physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ventricular ejection physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ventricular ejection physiology US Medical PG Question 1: A 16-year-old boy comes to the physician for a routine health maintenance examination. He feels well. He has no history of serious illness. He is at the 60th percentile for height and weight. Vital signs are within normal limits. The lungs are clear to auscultation. A grade 3/6 ejection systolic murmur is heard along the lower left sternal border. The murmur decreases in intensity on rapid squatting and increases in intensity when he performs the Valsalva maneuver. This patient is at increased risk for which of the following complications?
- A. Sudden cardiac death (Correct Answer)
- B. Pulmonary apoplexy
- C. Infective endocarditis
- D. Cerebral aneurysm
- E. Angiodysplasia
Ventricular ejection physiology Explanation: ***Sudden cardiac death***
- The murmur characteristics (decreases with squatting, increases with Valsalva) are classic for **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a leading cause of **sudden cardiac death** in young athletes.
- HOCM causes **left ventricular outflow tract obstruction** due to asymmetric septal hypertrophy and systolic anterior motion of the mitral valve, predisposing to fatal arrhythmias.
*Pulmonary apoplexy*
- This refers to severe **pulmonary hemorrhage**, which is not associated with the cardiac murmur described.
- It is typically seen in conditions like **Goodpasture's syndrome** or severe vasculitis.
*Infective endocarditis*
- While structural heart disease can increase the risk, the primary concern with HOCM is **sudden cardiac death** due to arrhythmia, not infective endocarditis, which generally requires specific predisposing factors like prosthetic valves or prolonged IV access.
- The murmur itself is due to obstruction, not typically indicative of an infection risk without other signs.
*Cerebral aneurysm*
- There is no direct association between the murmur characteristics described and an increased risk of **cerebral aneurysms**.
- Cerebral aneurysms are often linked to conditions like **polycystic kidney disease** or specific connective tissue disorders.
*Angiodysplasia*
- **Angiodysplasia** involves vascular malformations in the GI tract leading to bleeding, which is unrelated to the cardiovascular findings in this patient.
- It is often seen in older individuals or those with **aortic stenosis**, but not typically HOCM.
Ventricular ejection physiology US Medical PG Question 2: A 27-year-old woman, who recently immigrated from Bangladesh, presents to her primary care physician to discuss birth control. During a review of her past medical history, she reports that as a child she had a recurrent sore throat and fever followed by swollen and aching hip and knee joints. These symptoms returned every season and were never treated but went away on their own only to return with the next typhoon season. When asked about any current complaints, the patient says that she sometimes has shortness of breath and palpitations that do not last long. A physical exam is performed. In which of the auscultation sites will a murmur most likely be heard in this patient?
- A. Point 5 (Correct Answer)
- B. Point 4
- C. Point 2
- D. Point 3
- E. Point 1
Ventricular ejection physiology Explanation: ***Point 5***
- The patient's history of recurrent sore throat, fever, and migratory polyarthritis (swollen and aching hip and knee joints) followed by intermittent shortness of breath and palpitations is highly suggestive of **rheumatic fever** with subsequent **rheumatic heart disease**.
- This condition most commonly affects the **mitral valve**, leading to **mitral stenosis** or regurgitation, which would produce an apical murmur heard best at point 5 (the cardiac apex).
*Point 4*
- Point 4 corresponds to the **tricuspid area** (lower left sternal border). While rheumatic heart disease can affect the tricuspid valve, it is less common than mitral valve involvement and usually occurs in conjunction with severe mitral valve disease.
- An isolated murmur here would suggest tricuspid valve pathology, which is less likely as the primary presentation in rheumatic heart disease.
*Point 2*
- Point 2 is the **pulmonic area** (left upper sternal border, second intercostal space). Murmurs heard here typically indicate pulmonary valve disease or flow murmurs.
- While pulmonary hypertension can be a complication of severe left-sided heart disease, primary pulmonic valve involvement in rheumatic heart disease is rare.
*Point 3*
- Point 3 (Erb's point, third intercostal space, left sternal border) is often used to auscultate for murmurs of **aortic regurgitation** or to hear the splitting of S2.
- While aortic valve involvement can occur in rheumatic heart disease, **mitral valve disease** is significantly more prevalent and typically presents earlier and more severely.
*Point 1*
- Point 1 is the **aortic area** (right upper sternal border, second intercostal space). Murmurs heard here are typically associated with **aortic stenosis** or regurgitation.
- Although the aortic valve can be affected by rheumatic heart disease, the mitral valve is the most commonly involved valve, making an apical murmur (Point 5) more likely for the initial and most prominent finding.
Ventricular ejection physiology US Medical PG Question 3: A 19-year-old man presents to the clinic with a complaint of increasing shortness of breath for the past 2 years. His shortness of breath is associated with mild chest pain and occasional syncopal attacks during strenuous activity. There is no history of significant illness in the past, however, one of his uncles had similar symptoms when he was his age and died while playing basketball a few years later. He denies alcohol use, tobacco consumption, and the use of recreational drugs. On examination, pulse rate is 76/min and is regular and bounding; blood pressure is 130/70 mm Hg. A triple apical impulse is observed on the precordium and a systolic ejection crescendo-decrescendo murmur is audible between the apex and the left sternal border along with a prominent fourth heart sound. The physician then asks the patient to take a deep breath, close his mouth, and pinch his nose and try to breathe out without allowing his cheeks to bulge out. In doing so, the intensity of the murmur increases. Which of the following hemodynamic changes would be observed first during this maneuver?
- A. ↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow
- B. ↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow (Correct Answer)
- C. ↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow
- D. ↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow
- E. ↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow
Ventricular ejection physiology Explanation: **↑ Mean Arterial Pressure, ↓ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow**
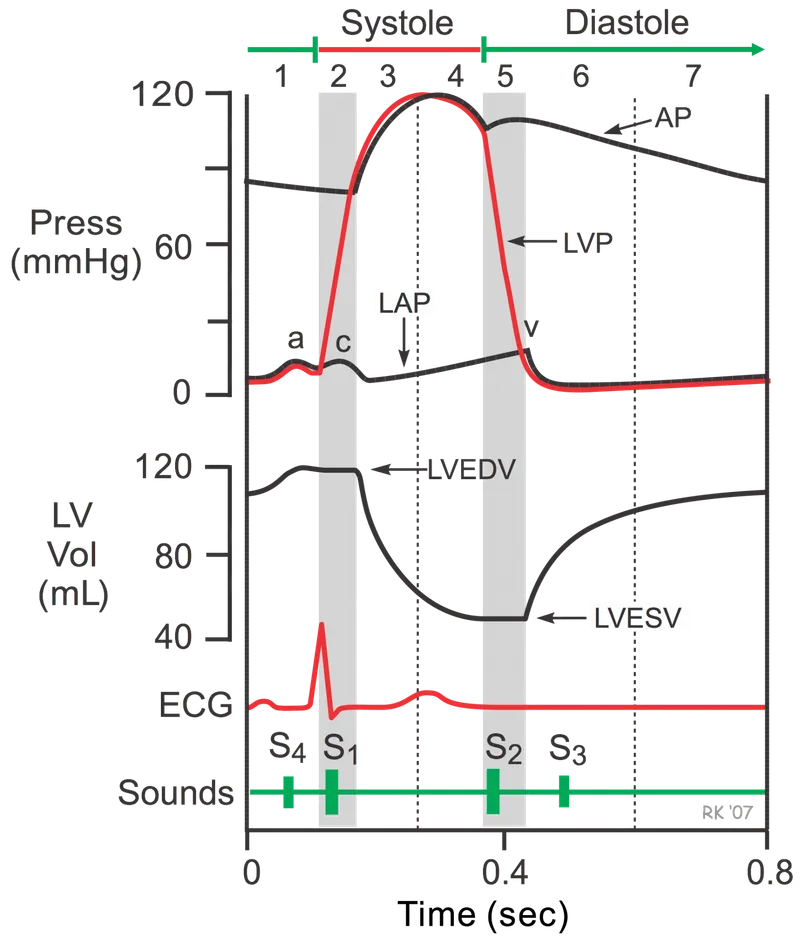
- This maneuver is the **Valsalva Maneuver**, which involves forced expiration against a closed glottis. It causes a transient increase in **intrathoracic pressure**, compressing the great vessels and temporarily increasing **mean arterial pressure**.
- The initial rise in blood pressure is detected by **baroreceptors**, leading to a reflex decrease in **heart rate** via increased **parasympathetic outflow**.
*↓ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↓ Parasympathetic Outflow*
- This option describes changes more typical of the **later phases** of a Valsalva maneuver (Phase 2), where venous return and cardiac output decrease, leading to a fall in MAP and a compensatory increase in heart rate.
- It does not represent the **immediate hemodynamic changes** (Phase 1) that occur during the initial strain of the maneuver.
*↑ Mean Arterial Pressure, ↓ Heart rate, ↓ Baroreceptor activity, ↑ Parasympathetic Outflow*
- A decrease in **baroreceptor activity** would typically lead to an *increase* in heart rate and a *decrease* in parasympathetic outflow, contrary to the initial response to increased blood pressure.
- The initial increase in MAP correctly leads to *increased* baroreceptor activity.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↓ Baroreceptor activity, ↓ Parasympathetic Outflow*
- An increase in **mean arterial pressure** (MAP) would reflexively cause a *decrease* in heart rate and an *increase* in parasympathetic outflow, mediated by *increased* baroreceptor activity, not decreased activity.
- Therefore, the proposed changes in heart rate, baroreceptor activity, and parasympathetic outflow are inconsistent with an initial increase in MAP.
*↑ Mean Arterial Pressure, ↑ Heart rate, ↑ Baroreceptor activity, ↑ Parasympathetic Outflow*
- While an increase in **mean arterial pressure** does lead to an increase in **baroreceptor activity** and **parasympathetic outflow**, the reflexive response to this increased pressure is a *decrease* in **heart rate**, not an increase.
- An increased heart rate combined with increased parasympathetic outflow is contradictory, as sympathetic and parasympathetic systems typically exert opposing effects on heart rate.
Ventricular ejection physiology US Medical PG Question 4: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Ventricular ejection physiology Explanation: ***Heart failure***
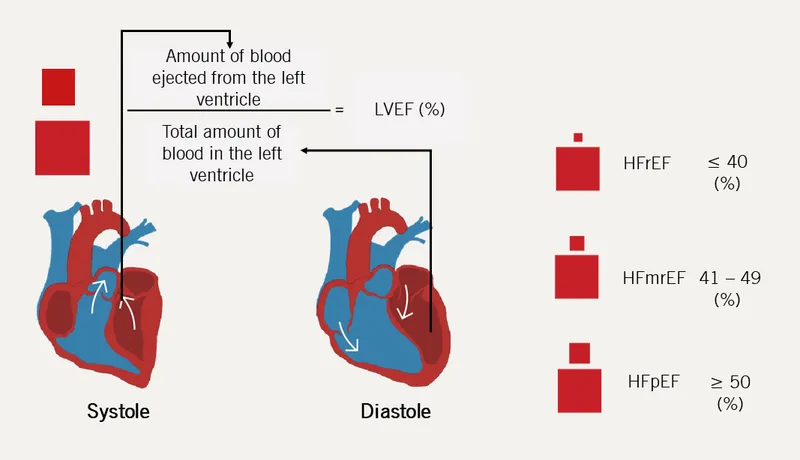
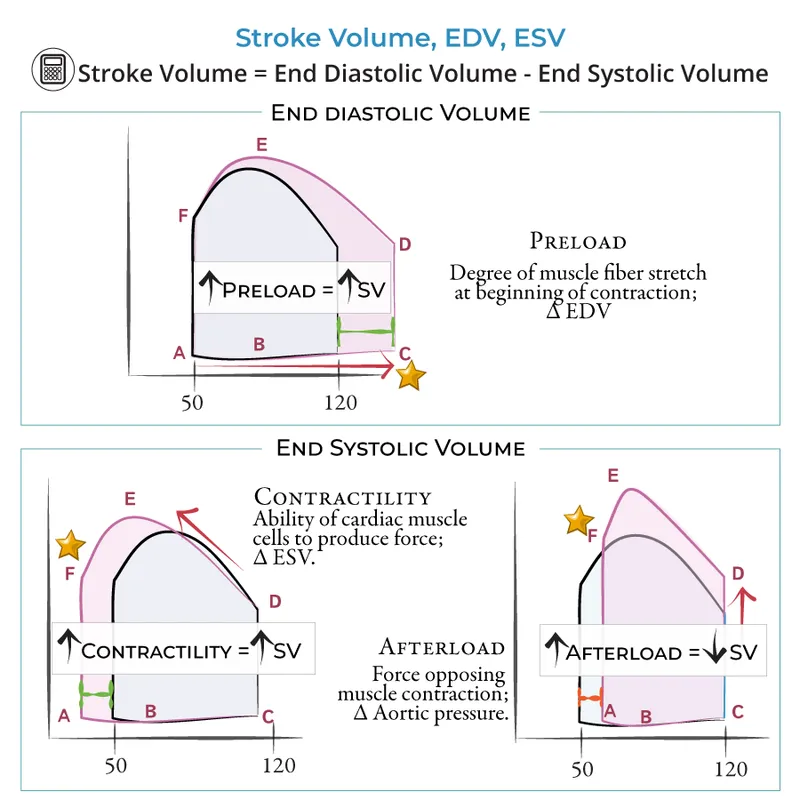
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Ventricular ejection physiology US Medical PG Question 5: A 37-year-old male presents to your clinic with shortness of breath and lower extremity edema. He was born in Southeast Asia and emigrated to America ten years prior. Examination demonstrates 2+ pitting edema to the level of his knees, ascites, and bibasilar crackles, as well as an opening snap followed by a mid-to-late diastolic murmur. The patient undergoes a right heart catheterization that demonstrates a pulmonary capillary wedge pressure (PCWP) of 24 mmHg. The patient is most likely to have which of the following?
- A. Normal or decreased left ventricular end diastolic pressure (LVEDP) (Correct Answer)
- B. Decreased transmitral gradient
- C. Decreased pulmonary artery systolic pressure (PASP)
- D. Increased left ventricular end diastolic pressure (LVEDP)
- E. Increased pulmonary vascular compliance
Ventricular ejection physiology Explanation: ***Normal or decreased left ventricular end diastolic pressure (LVEDP)***
- The patient's symptoms (opening snap, mid-to-late diastolic murmur, Southeast Asian origin) strongly suggest **mitral stenosis**.
- In mitral stenosis, the obstruction at the **mitral valve** leads to elevated left atrial pressure (reflected by the high PCWP), but the left ventricle itself is not failing, so LVEDP is typically normal or even decreased.
*Decreased transmitral gradient*
- A **mid-to-late diastolic murmur** and an **opening snap** are classic signs of mitral stenosis, indicating a high pressure gradient across the mitral valve during diastole.
- A decreased transmitral gradient would imply reduced obstruction, which contradicts the patient's strong clinical presentation.
*Decreased pulmonary artery systolic pressure (PASP)*
- Elevated pulmonary capillary wedge pressure (PCWP) of 24 mmHg indicates **pulmonary hypertension secondary to left atrial pressure elevation** in mitral stenosis.
- This consistently leads to an **increased pulmonary artery systolic pressure (PASP)**, not a decreased one, as the right ventricle has to work harder to pump blood through the high-pressure pulmonary vasculature.
*Increased left ventricular end diastolic pressure (LVEDP)*
- While PCWP is elevated due to **left atrial pressure overload** in mitral stenosis, the left ventricle itself is not volume or pressure overloaded during diastole.
- The LVEDP would only be increased if there was actual left ventricular dysfunction or aortic valve disease, which is not suggested here.
*Increased pulmonary vascular compliance*
- Chronic pulmonary hypertension, as seen in advanced mitral stenosis with high PCWP, leads to **pulmonary vascular remodeling** and **decreased pulmonary vascular compliance**.
- The pulmonary vessels become stiffer and less distensible, not more compliant.
Ventricular ejection physiology US Medical PG Question 6: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Ventricular ejection physiology Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Ventricular ejection physiology US Medical PG Question 7: A 59-year-old woman comes to the physician for a 3-month history of progressively worsening shortness of breath on exertion and swelling of her legs. She has a history of breast cancer, which was treated with surgery followed by therapy with doxorubicin and trastuzumab 4 years ago. Cardiac examination shows an S3 gallop; there are no murmurs or rubs. Examination of the lower extremities shows pitting edema below the knees. Echocardiography is most likely to show which of the following sets of changes in this patient?
$$$ Ventricular wall thickness %%% Ventricular cavity size %%% Diastolic function %%% Aorto-ventricular pressure gradient $$$
- A. ↓ ↑ normal normal (Correct Answer)
- B. Normal normal ↓ normal
- C. ↑ ↓ ↓ normal
- D. ↑ ↓ ↓ ↑
- E. ↓ ↑ ↓ normal
Ventricular ejection physiology Explanation: ***↓ ↑ normal normal***
- Doxorubicin is an **anthracycline** known to cause **dilated cardiomyopathy**, characterized by **decreased ventricular wall thickness**, **increased ventricular cavity size**, and **preserved diastolic function**.
- The S3 gallop and pitting edema indicate **heart failure with reduced ejection fraction (HFrEF)**, consistent with dilated cardiomyopathy.
*Normal normal ↓ normal*
- This option suggests a primary issue with **diastolic function**, which is not the typical presentation of doxorubicin-induced cardiomyopathy.
- While diastolic dysfunction can occur, doxorubicin characteristically causes **systolic dysfunction** manifesting as chamber dilation and wall thinning.
*↑ ↓ ↓ normal*
- This pattern of **increased wall thickness** and **decreased cavity size** is characteristic of **hypertrophic cardiomyopathy** or **restrictive cardiomyopathy**, which are generally not caused by doxorubicin.
- Doxorubicin typically causes **cardiac muscle fiber damage** leading to thinning and dilation.
*↑ ↓ ↓ ↑*
- This option also suggests **increased wall thickness** and **decreased cavity size**, inconsistent with doxorubicin's effects on the heart.
- The **elevated aorto-ventricular pressure gradient** might indicate outflow tract obstruction or significant aortic stenosis, which are not typical sequelae of doxorubicin.
*↓ ↑ ↓ normal*
- While doxorubicin leads to **decreased wall thickness** and **increased cavity size**, the diastolic function is usually preserved early on, not decreased.
- A decrease in diastolic function might occur in later stages, but the primary and most characteristic feature due to doxorubicin is **systolic dysfunction** and chamber remodeling.
Ventricular ejection physiology US Medical PG Question 8: You are interested in studying the etiology of heart failure reduced ejection fraction (HFrEF) and attempt to construct an appropriate design study. Specifically, you wish to look for potential causality between dietary glucose consumption and HFrEF. Which of the following study designs would allow you to assess for and determine this causality?
- A. Cross-sectional study
- B. Case series
- C. Cohort study (Correct Answer)
- D. Case-control study
- E. Randomized controlled trial
Ventricular ejection physiology Explanation: ***Cohort study***
- A **cohort study** observes a group of individuals over time to identify risk factors and outcomes, allowing for the assessment of **temporal relationships** between exposure (dietary glucose) and outcome (HFrEF).
- This design is suitable for establishing a potential **causal link** as it tracks participants from exposure to outcome, enabling the calculation of incidence rates and relative risks.
*Cross-sectional study*
- A **cross-sectional study** measures exposure and outcome simultaneously at a single point in time, making it impossible to determine the **temporal sequence** of events.
- This design can only identify **associations** or correlations, not causation, as it cannot establish whether high glucose consumption preceded HFrEF.
*Case series*
- A **case series** describes characteristics of a group of patients with a particular disease or exposure, often to highlight unusual clinical features, but it lacks a **comparison group**.
- It cannot assess causality because it does not provide information on the frequency of exposure in healthy individuals or the incidence of the disease in unexposed individuals.
*Case-control study*
- A **case-control study** compares individuals with the outcome (cases) to those without the outcome (controls) to determine past exposures, which makes it prone to **recall bias**.
- While it can suggest associations, it cannot definitively establish a temporal relationship or causation as the outcome is already known when exposure is assessed.
*Randomized controlled trial*
- A **randomized controlled trial (RCT)** is the gold standard for establishing causation by randomly assigning participants to an intervention or control group, but it may not be ethical or feasible for studying long-term dietary exposures and chronic diseases like HFrEF due to the long follow-up period and complexity of diet.
- While ideal for causality, directly controlling and randomizing dietary glucose intake over decades to observe HFrEF development might be practically challenging or unethical.
Ventricular ejection physiology US Medical PG Question 9: A 53-year-old man with a past medical history significant for hyperlipidemia, hypertension, and hyperhomocysteinemia presents to the emergency department complaining of 10/10 crushing, left-sided chest pain radiating down his left arm and up his neck into the left side of his jaw. His ECG shows ST-segment elevation in leads V2-V4. He is taken to the cardiac catheterization laboratory for successful balloon angioplasty and stenting of a complete blockage in his left anterior descending coronary artery. Echocardiogram the following day shows decreased left ventricular function and regional wall motion abnormalities. A follow-up echocardiogram 14 days later shows a normal ejection fraction and no regional wall motion abnormalities. This post-infarct course illustrates which of the following concepts?
- A. Coronary collateral circulation
- B. Ventricular remodeling
- C. Myocardial hibernation
- D. Myocardial stunning (Correct Answer)
- E. Reperfusion injury
Ventricular ejection physiology Explanation: ***Myocardial stunning***
- This refers to a temporary **post-ischemic contractile dysfunction** that persists even after blood flow has been restored following an acute ischemic event.
- The return to normal left ventricular function and absence of regional wall motion abnormalities after successful reperfusion indicates that the initial dysfunction was transient and not due to permanent myocardial damage.
- Classic timeframe: recovery occurs over **days to weeks** after reperfusion, as seen in this patient (14 days).
*Coronary collateral circulation*
- This involves the development of alternative pathways for blood supply to the myocardium when the primary coronary arteries are occluded.
- While it can mitigate the extent of myocardial injury, it generally doesn't explain the reversal of severe regional wall motion abnormalities and low ejection fraction to normal in such a short period after a complete blockage.
*Ventricular remodeling*
- This refers to changes in the **size, shape, and function of the ventricles** in response to myocardial injury or chronic pressure/volume overload, often leading to progressive heart failure.
- It typically involves *persistent* and *often detrimental* changes, which is contrary to the improvement seen in this patient's echocardiogram.
*Myocardial hibernation*
- This is a state of **persistently impaired myocardial function at rest** due to **chronic inadequate blood flow** that can improve with revascularization.
- Hibernation requires **pre-existing chronic ischemia** with baseline dysfunction prior to intervention, not an acute complete occlusion presenting as STEMI.
- This patient had an **acute presentation** with complete blockage and no history suggesting chronic stable ischemia, making stunning (not hibernation) the correct answer.
*Reperfusion injury*
- This is damage to the myocardial tissue that occurs **after blood flow is restored** to an ischemic area, often involving oxidative stress and inflammation.
- While it can worsen myocardial function, it is a complication of reperfusion that causes *additional damage*, not a phenomenon that explains the *recovery* of cardiac function after reperfusion.
Ventricular ejection physiology US Medical PG Question 10: A 36-year-old woman is admitted to the hospital for the evaluation of progressive breathlessness. She has no history of major medical illness. Her temperature is 37°C (98.6°F), pulse is 110/min, and respirations are 22/min. Pulse oximetry on room air shows an oxygen saturation of 99%. Cardiac examination shows a loud S1 and S2. There is a grade 2/6 early systolic murmur best heard in the 2nd right intercostal space. Cardiac catheterization shows a mixed venous oxygen saturation of 55% (N= 65–70%). Which of the following is the most likely cause of this patient's breathlessness?
- A. Increased peripheral shunting
- B. Decreased hemoglobin concentration
- C. Increased carbon dioxide retention
- D. Increased pulmonary vascular resistance
- E. Decreased left ventricular ejection fraction (Correct Answer)
Ventricular ejection physiology Explanation: ***Decreased left ventricular ejection fraction***
- The key finding is a **mixed venous oxygen saturation of 55% (normal 65-70%)** with **normal arterial oxygen saturation (99%)**, which indicates **increased tissue oxygen extraction**
- Increased oxygen extraction occurs when **cardiac output is reduced** → tissues must extract more oxygen from each pass of blood to meet metabolic demands
- This is the classic physiologic compensation in **heart failure with reduced ejection fraction**
- The cardiac findings (loud heart sounds, systolic murmur) suggest underlying cardiac pathology causing reduced cardiac output and progressive breathlessness
*Increased peripheral shunting*
- Peripheral shunting (e.g., arteriovenous malformations) would cause **venous blood to bypass capillary beds**, resulting in **decreased oxygen extraction** and **higher mixed venous O2 saturation**, not lower
- Would typically cause **hypoxemia** with reduced pulse oximetry, but this patient has 99% oxygen saturation
*Decreased hemoglobin concentration*
- Anemia reduces oxygen-carrying capacity but would not explain the **low mixed venous oxygen saturation** to this degree
- The **pulse oximetry of 99%** indicates adequate oxygen saturation of available hemoglobin
- Anemia typically causes **high cardiac output** (compensatory) rather than the low cardiac output state indicated by the low mixed venous O2 saturation
*Increased carbon dioxide retention*
- **Hypercapnia** results from **hypoventilation** and impaired gas exchange, typically causing **respiratory acidosis**
- Would present with altered mental status, drowsiness, or signs of respiratory failure
- Does not explain the **low mixed venous oxygen saturation** with normal arterial oxygen saturation
- The cardiac findings point to a primary cardiac rather than respiratory problem
*Increased pulmonary vascular resistance*
- **Pulmonary hypertension** causes **right ventricular dysfunction** and can present with breathlessness and a loud P2 component of S2
- However, isolated pulmonary hypertension would not cause the same degree of **systemic oxygen extraction** increase
- The low mixed venous O2 saturation indicates **reduced systemic cardiac output**, which primarily reflects **left ventricular dysfunction** rather than isolated right-sided pathology
More Ventricular ejection physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.