Valve function during cardiac cycle US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Valve function during cardiac cycle. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Valve function during cardiac cycle US Medical PG Question 1: A 62-year-old man comes to the physician for decreased exercise tolerance. Over the past four months, he has noticed progressively worsening shortness of breath while walking his dog. He also becomes short of breath when lying in bed at night. His temperature is 36.4°C (97.5°F), pulse is 82/min, respirations are 19/min, and blood pressure is 155/53 mm Hg. Cardiac examination shows a high-pitch, decrescendo murmur that occurs immediately after S2 and is heard best along the left sternal border. There is an S3 gallop. Carotid pulses are strong. Which of the following is the most likely diagnosis?
- A. Aortic valve regurgitation (Correct Answer)
- B. Tricuspid valve regurgitation
- C. Mitral valve prolapse
- D. Mitral valve regurgitation
- E. Mitral valve stenosis
Valve function during cardiac cycle Explanation: ***Aortic valve regurgitation***
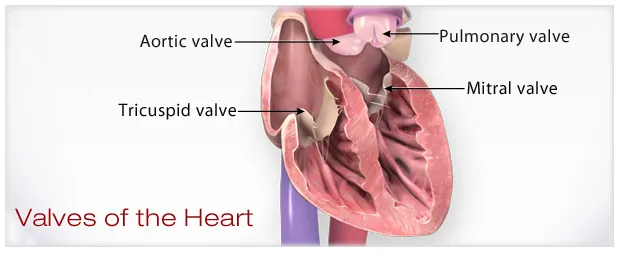
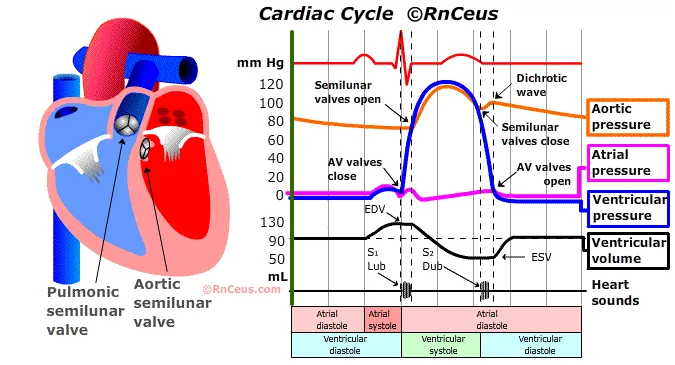
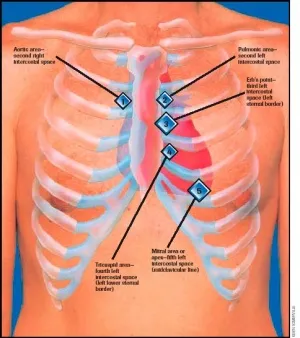
- A **high-pitch, decrescendo murmur immediately after S2** and heard best along the **left sternal border** is characteristic of **aortic regurgitation**.
- Symptoms like **dyspnea on exertion** and **orthopnea**, an **S3 gallop**, and a **wide pulse pressure** (155/53 mmHg) further support heart failure due to chronic aortic regurgitation.
*Tricuspid valve regurgitation*
- This typically presents with a **holosystolic murmur** best heard at the **left lower sternal border** that increases with inspiration.
- Clinical signs often include **jugular venous distension** and **peripheral edema**, not primarily a decrescendo diastolic murmur.
*Mitral valve prolapse*
- Characterized by a **mid-systolic click** followed by a **late systolic murmur**, and symptomatically may be asymptomatic or cause palpitations.
- The described diastolic murmur and symptoms of heart failure do not align with mitral valve prolapse.
*Mitral valve regurgitation*
- Typically presents as a **holosystolic murmur** heard best at the **apex** and often radiating to the axilla.
- While it can cause dyspnea and an S3, the character and timing of the murmur reported (decrescendo, immediately after S2) are inconsistent with mitral regurgitation.
*Mitral valve stenosis*
- This condition presents with a **diastolic rumble** heard best at the **apex** with an opening snap.
- The murmur described is a high-pitch decrescendo murmur, which is distinct from the low-pitched rumble of mitral stenosis.
Valve function during cardiac cycle US Medical PG Question 2: A 76-year-old male with a history of chronic uncontrolled hypertension presents to the emergency room following an episode of syncope. He reports that he felt lightheaded and experienced chest pain while walking his dog earlier in the morning. He notes that he has experienced multiple similar episodes over the past year. A trans-esophageal echocardiogram demonstrates a thickened, calcified aortic valve with left ventricular hypertrophy. Which of the following heart sounds would likely be heard on auscultation of this patient?
- A. Crescendo-decrescendo murmur radiating to the carotids that is loudest at the right upper sternal border (Correct Answer)
- B. Diastolic rumble following an opening snap with an accentuated S1
- C. Early diastolic high-pitched blowing decrescendo murmur that is loudest at the left sternal border
- D. Holosystolic murmur radiating to the axilla that is loudest at the apex
- E. Midsystolic click that is loudest at the apex
Valve function during cardiac cycle Explanation: ***Crescendo-decrescendo murmur radiating to the carotids that is loudest at the right upper sternal border***
- The patient's symptoms of **syncope**, **chest pain**, and findings of a **thickened, calcified aortic valve** with **left ventricular hypertrophy** are classic for **aortic stenosis**.
- Aortic stenosis classically presents with a **systolic ejecting crescendo-decrescendo murmur** which is loudest at the **right upper sternal border**, and often **radiates to the carotids**.
*Diastolic rumble following an opening snap with an accentuated S1*
- This description is characteristic of **mitral stenosis**, which is typically caused by **rheumatic fever**.
- Mitral stenosis would present with dyspnea and fatigue, unlike the syncope and chest pain seen in this patient.
*Early diastolic high-pitched blowing decrescendo murmur that is loudest at the left sternal border*
- This murmur describes **aortic regurgitation**, where blood flows back into the left ventricle during diastole.
- While aortic regurgitation can cause heart failure symptoms, the echocardiogram shows a thickened, calcified valve more consistent with stenosis.
*Midsystolic click that is most prominent that is loudest at the apex*
- A **midsystolic click** followed by a **late systolic murmur** is characteristic of **mitral valve prolapse**.
- Symptoms of mitral valve prolapse can include atypical chest pain and palpitations, but not generally exertional syncope or the severe structural changes seen in the aortic valve.
*Holosystolic murmur radiating to the axilla that is loudest at the apex*
- This is the classic description of **mitral regurgitation**, indicating blood flow back into the left atrium during systole.
- Mitral regurgitation is associated with symptoms of heart failure and fatigue, but not usually the anginal chest pain and syncope in a patient with a calcified aortic valve.
Valve function during cardiac cycle US Medical PG Question 3: A 65-year-old male with a history of coronary artery disease and myocardial infarction status post coronary artery bypass graft (CABG) surgery presents to his cardiologist for a routine appointment. On physical exam, the cardiologist appreciates a holosystolic, high-pitched blowing murmur heard loudest at the apex and radiating towards the axilla. Which of the following is the best predictor of the severity of this patient's murmur?
- A. Enhancement with expiration
- B. Presence of audible S3 (Correct Answer)
- C. Enhancement with hand grip maneuver
- D. Presence of audible S4
- E. Enhancement with inspiration
Valve function during cardiac cycle Explanation: ***Presence of audible S3***
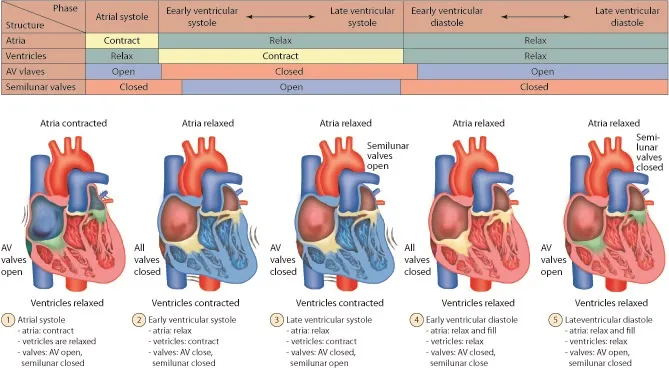
- An **S3 gallop** indicates rapid ventricular filling into a stiff or volume-overloaded ventricle, suggesting significant ventricular dysfunction due to severe regurgitation and increased preload.
- In the context of **mitral regurgitation (MR)**, an S3 is a strong predictor of **severe MR** and associated **left ventricular dysfunction**.
*Enhancement with expiration*
- This maneuver typically enhances **left-sided heart murmurs**, including mitral regurgitation, by increasing venous return to the left side of the heart.
- While it confirms the murmur's origin, it does not directly predict the **severity** of the regurgitation.
*Enhancement with hand grip maneuver*
- The **handgrip maneuver** increases afterload, which can enhance the intensity of murmurs associated with regurgitant lesions like mitral regurgitation.
- While helpful in identifying MR, it is not the best predictor of its **severity** compared to signs of ventricular dysfunction.
*Presence of audible S4*
- An **S4 heart sound** is associated with reduced ventricular compliance and atrial contraction against a stiff ventricle, often seen in conditions like **hypertension** or **aortic stenosis**.
- It does not directly indicate the **severity of mitral regurgitation** or current ventricular volume overload.
*Enhancement with inspiration*
- This maneuver typically enhances **right-sided heart murmurs** by increasing venous return to the right side of the heart.
- Since mitral regurgitation is a **left-sided murmur**, inspiration would likely have little to no effect or diminish its intensity.
Valve function during cardiac cycle US Medical PG Question 4: A 61-year-old man comes to the physician because of a 3-month history of fatigue and progressively worsening shortness of breath that is worse when lying down. Recently, he started using two pillows to avoid waking up short of breath at night. Examination shows a heart murmur. A graph with the results of cardiac catheterization is shown. Given this patient's valvular condition, which of the following murmurs is most likely to be heard on cardiac auscultation?
- A. High-frequency, diastolic murmur heard best at the 2nd left intercostal space
- B. Harsh, late systolic murmur that radiates to the carotids
- C. Blowing, early diastolic murmur heard best at the Erb point
- D. High-pitched, holosystolic murmur that radiates to the axilla (Correct Answer)
- E. Rumbling, delayed diastolic murmur heard best at the cardiac apex
Valve function during cardiac cycle Explanation: ***High-pitched, holosystolic murmur that radiates to the axilla***
- The patient's symptoms of **fatigue**, **dyspnea on exertion** and **orthopnea**, combined with a heart murmur, are highly suggestive of **heart failure** caused by **mitral regurgitation**.
- A **high-pitched**, **holosystolic murmur** heard best at the **apex** and **radiating to the axilla** is the classic description of mitral regurgitation.
*High-frequency, diastolic murmur heard best at the 2nd left intercostal space*
- This describes the murmur of **pulmonary regurgitation**, which is typically heard best at the **left upper sternal border**.
- The patient's symptoms are more consistent with left-sided heart failure due to a different valvular issue.
*Harsh, late systolic murmur that radiates to the carotids*
- This is the characteristic murmur of **aortic stenosis**, which is heard best at the **right upper sternal border**.
- While aortic stenosis can cause similar symptoms, the description of the murmur and the specific context of heart failure symptoms here point away from it.
*Blowing, early diastolic murmur heard best at the Erb point*
- This describes the **diastolic murmur of aortic regurgitation**, often heard best at the **Erb's point** (3rd intercostal space, left sternal border).
- While aortic regurgitation can cause heart failure, its murmur is diastolic, not holosystolic, and the maximal intensity and radiation differ from the classic mitral regurgitation.
*Rumbling, delayed diastolic murmur heard best at the cardiac apex*
- This is the characteristic murmur of **mitral stenosis**, which is typically preceded by an **opening snap**.
- Mitral stenosis would lead to different hemodynamic changes and often presents with symptoms related to pulmonary congestion, but the murmur timing and quality are distinct from a holosystolic murmur of regurgitation.
Valve function during cardiac cycle US Medical PG Question 5: A 64-year-old man presents to the emergency department because he has been experiencing increased shortness of breath for the last 2 weeks. Specifically, he says that he can barely walk up the stairs to his apartment before he feels winded. In addition, he has been waking up at night gasping for breath and has only been able to sleep propped up on 2 more pillows than usual. Physical exam reveals jugular venous distention as well as pitting lower extremity edema. Which of the following abnormal sounds will most likely be heard in this patient?
- A. Opening snap
- B. Extra heart sound in early diastole (Correct Answer)
- C. Extra heart sound in late diastole
- D. Fixed splitting
- E. Parasternal holosystolic murmur
Valve function during cardiac cycle Explanation: ***Extra heart sound in early diastole***
- The patient's symptoms (dyspnea, orthopnea, paroxysmal nocturnal dyspnea, jugular venous distention, edema) are classic for **congestive heart failure (CHF)**.
- An **S3 gallop** is an extra heart sound occurring in **early diastole** and is pathognomonic for **volume overload** and **ventricular dysfunction** in CHF.
*Opening snap*
- An **opening snap** is typically heard in **mitral stenosis**, which is not directly indicated by the patient's symptoms of volume overload from heart failure.
- This sound occurs shortly after S2 as the stenotic mitral valve opens.
*Extra heart sound in late diastole*
- An extra heart sound in **late diastole** is often an **S4 gallop**, which indicates **poor ventricular compliance** (e.g., in hypertension or aortic stenosis) rather than the pronounced volume overload suggested by the current presentation.
- An S4 is heard just before S1, as the atria contract to push blood into a stiff ventricle.
*Fixed splitting*
- **Fixed splitting of S2** is characteristic of an **atrial septal defect (ASD)**, where there is a constant delay in pulmonic valve closure, independent of respiration.
- This is not a typical finding in the context of acute decompensated heart failure as described.
*Parasternal holosystolic murmur*
- A **parasternal holosystolic murmur** is typically associated with **ventricular septal defect (VSD)** or **tricuspid regurgitation**.
- While tricuspid regurgitation can occur secondary to right heart failure, the most immediate and common auscultatory finding for overall heart failure with volume overload is an S3.
Valve function during cardiac cycle US Medical PG Question 6: A 52-year-old man comes to the physician for a routine health maintenance examination. He has not seen a physician for 10 years. He works as a telemarketer and does not exercise. Cardiac examination shows a dull, low-pitched sound during late diastole that is best heard at the apex. The sound is loudest in the left lateral decubitus position and during end-expiration. Which of the following is the most likely cause of this finding?
- A. Fusion of mitral valve leaflets
- B. Dilation of both ventricles
- C. Concentric left ventricular hypertrophy (Correct Answer)
- D. Aortic root dilatation
- E. Right bundle branch block
Valve function during cardiac cycle Explanation: ***Concentric left ventricular hypertrophy***
- The described **dull, low-pitched sound** during **late diastole**, best heard at the apex in the left lateral decubitus position and during end-expiration, is consistent with a **S4 gallop**.
- An **S4 heart sound** is caused by the **atrial kick** into a **stiff, non-compliant ventricle**, which is characteristic of **concentric left ventricular hypertrophy** due to long-standing hypertension or aortic stenosis.
*Fusion of mitral valve leaflets*
- This condition, known as **mitral stenosis**, typically causes a **mid-diastolic rumble** with an opening snap, not an S4 sound.
- The associated murmur would be loudest closer to the S2 sound and might have a snapping quality.
*Dilation of both ventricles*
- **Dilated cardiomyopathy** with compromised systolic function can lead to an **S3 gallop** (early diastolic sound) due to rapid ventricular filling into an already overloaded ventricle.
- It does not typically cause an S4 sound, which is associated with ventricular stiffness.
*Aortic root dilatation*
- This can lead to **aortic regurgitation**, which is typically characterized by an **early diastolic decrescendo murmur** heard best at the left sternal border.
- It is not associated with an S4 sound.
*Right bundle branch block*
- A **right bundle branch block (RBBB)** is an electrical conduction abnormality that results in a **widely split S2 heart sound** due to delayed pulmonic valve closure.
- It does not directly produce an S4 sound, which is a mechanical event related to ventricular compliance.
Valve function during cardiac cycle US Medical PG Question 7: Seventy-two hours after admission for an acute myocardial infarction, a 48-year-old man develops dyspnea and a productive cough with frothy sputum. Physical examination shows coarse crackles in both lungs and a blowing, holosystolic murmur heard best at the apex. ECG shows Q waves in the anteroseptal leads. Pulmonary capillary wedge pressure is 23 mm Hg. Which of the following is the most likely cause of this patient’s current condition?
- A. Rupture of the ventricular free wall
- B. Postmyocardial infarction syndrome
- C. Aortic root dilation
- D. Rupture of the interventricular septum
- E. Rupture of the chordae tendineae (Correct Answer)
Valve function during cardiac cycle Explanation: ***Rupture of the chordae tendineae***
- The combination of acute dyspnea, frothy sputum (**pulmonary edema**), a new **holosystolic murmur** loudest at the apex, suggestive of **mitral regurgitation**, and high **pulmonary capillary wedge pressure** (PCWP > 18 mmHg indicating pulmonary edema) is classic for papillary muscle or chordae tendineae rupture following an **acute myocardial infarction (MI)**.
- Antero-septal Q waves suggest an infarction in an area supplied by the **left anterior descending artery**, which can also affect the **anterolateral papillary muscle** of the mitral valve.
*Rupture of the ventricular free wall*
- This typically presents as **cardiac tamponade** with hypotension, jugular venous distension, and muffled heart sounds, often leading to rapid hemodynamic collapse and death.
- While it can occur post-MI, a new holosystolic murmur and prominent pulmonary edema are not characteristic features.
*Postmyocardial infarction syndrome*
- Also known as **Dressler syndrome**, this is a **pericarditis** that develops weeks to months after an MI.
- It presents with fever, pleuritic chest pain, and pericardial friction rub and would not typically cause acute pulmonary edema or a new holosystolic murmur within 72 hours.
*Aortic root dilation*
- This condition is not directly linked to an acute MI and typically causes **aortic regurgitation**, which manifests as a **diastolic murmur** (decrescendo early diastolic murmur), not a holosystolic murmur.
- While it can cause heart failure, the acute onset post-MI with a new apical holosystolic murmur points away from this diagnosis.
*Rupture of the interventricular septum*
- This would also present with a new **holosystolic murmur**, but it would be loudest at the **left sternal border** due to a **ventricular septal defect**.
- While it can cause pulmonary edema and elevated PCWP, the murmur's location at the apex strongly points towards mitral valve pathology rather than a septal defect.
Valve function during cardiac cycle US Medical PG Question 8: A 65-year-old man is brought to the emergency department with central chest pain for the last hour. He rates his pain as 8/10, dull in character, and says it is associated with profuse sweating and shortness of breath. He used to have heartburn and upper abdominal pain associated with food intake but had never experienced chest pain this severe. He has a history of diabetes, hypertension, and hypercholesterolemia. His current medication list includes amlodipine, aspirin, atorvastatin, insulin, valsartan, and esomeprazole. He has smoked 1 pack of cigarettes per day for the past 35 years. Physical examination reveals: blood pressure 94/68 mm Hg, pulse 112/min, oxygen saturation 95% on room air, and BMI 31.8 kg/m2. His lungs are clear to auscultation. An electrocardiogram (ECG) shows ST-segment elevations in the inferior leads. The patient is discharged home after 3 days on aspirin, clopidogrel, and atenolol in addition to his previous medications. He is advised to get an exercise tolerance test (ETT) in one month. A month later at his ETT, his resting blood pressure is 145/86 mm Hg. The pre-exercise ECG shows normal sinus rhythm with Q waves in the inferior leads. After 3 minutes of exercise, the patient develops chest pain that is gradually worsening, and repeat blood pressure is 121/62 mm Hg. No ischemic changes are noted on the ECG. What is the most appropriate next step?
- A. Stop exercise and order a coronary angiography (Correct Answer)
- B. Stop exercise and order a pharmacological stress test
- C. Stop exercise and order an echo stress test
- D. Continue exercise since ECG does not show ischemic changes
- E. Repeat exercise tolerance testing after one month
Valve function during cardiac cycle Explanation: **Stop exercise and order a coronary angiography**
- The patient's developing chest pain during the exercise tolerance test, despite no ECG changes, is highly suggestive of **myocardial ischemia** due to his extensive cardiac risk factors and prior STEMI. The **drop in blood pressure** during exercise indicates possible cardiac dysfunction or severe ischemia, making immediate investigation with **coronary angiography** critical.
- Given the patient's strong history of coronary artery disease (CAD), including a recent myocardial infarction, an exercise-induced symptom warrants immediate and definitive evaluation for **obstructive CAD** to guide further management.
*Stop exercise and order a pharmacological stress test*
- While pharmacological stress tests are useful for patients unable to exercise, this patient is already undergoing an exercise test and has demonstrated a symptom during exertion.
- A pharmacological stress test would provide functional information but would not directly image the coronary arteries, which is crucial given the high suspicion for severe CAD.
*Stop exercise and order an echo stress test*
- An echo stress test would assess wall motion abnormalities indicative of ischemia, but similar to other stress tests, it provides functional information rather than direct anatomical visualization of coronary blockages.
- While valuable, in the context of this patient's acute symptoms and risk profile, **coronary angiography** offers a more direct and definitive diagnostic approach to identify and potentially intervene on arterial blockages.
*Continue exercise since ECG does not show ischemic changes*
- Continuing exercise when a patient develops chest pain and a drop in blood pressure is **contraindicated** and dangerous.
- **Symptoms (chest pain)** and **hemodynamic changes (blood pressure drop)** are critical indicators of ischemia, even if ECG changes are absent, as ECG sensitivity for detecting ischemia is not 100%.
*Repeat exercise tolerance testing after one month*
- Repeating the test ignores the significant and alarming symptoms the patient experienced during this test.
- It would delay definitive diagnosis and treatment, putting the patient at unnecessarily high risk of another cardiac event.
Valve function during cardiac cycle US Medical PG Question 9: A 19-year-old woman comes to the physician for a routine health maintenance examination. She appears well. Her vital signs are within normal limits. Cardiac auscultation shows a mid-systolic click and a grade 3/6, late-systolic, crescendo murmur that is best heard at the cardiac apex in the left lateral recumbent position. After the patient stands up suddenly, the click is heard during early systole and the intensity of the murmur increases. Which of the following is the most likely underlying cause of this patient's examination findings?
- A. Congenital interventricular communication
- B. Myxomatous degeneration (Correct Answer)
- C. Dystrophic valvular calcification
- D. Congenital valvular fusion
- E. Myosin heavy chain defect
Valve function during cardiac cycle Explanation: ***Myxomatous degeneration***
- The classic auscultation findings of a **mid-systolic click** followed by a **late-systolic crescendo murmur** heard best at the apex are characteristic of **mitral valve prolapse (MVP)**.
- The change in timing of the click to early systole and increased murmur intensity upon standing are due to decreased left ventricular volume, which accentuates MVP by causing the mitral valve leaflets to prolapse earlier and more severely. These findings are the result of **myxomatous degeneration** of the mitral valve leaflets.
*Congenital interventricular communication*
- This condition (e.g., **ventricular septal defect**) typically presents with a **holosystolic murmur** best heard at the lower left sternal border and is usually detected earlier in life.
- It would not cause a mid-systolic click or a late-systolic crescendo murmur that changes with position in this manner.
*Dystrophic valvular calcification*
- **Dystrophic calcification** is a common cause of **aortic stenosis** in older individuals and is not typically associated with mitral valve prolapse in a young patient.
- Aortic stenosis produces a **crescendo-decrescendo systolic murmur** loudest at the right upper sternal border, often radiating to the carotids, without a mid-systolic click.
*Congenital valvular fusion*
- **Congenital valvular fusion** usually leads to **stenosis** (e.g., congenital aortic stenosis or bicuspid aortic valve) or **regurgitation**, depending on the valve involved.
- While it can cause murmurs, it does not typically present with the specific mid-systolic click and late-systolic crescendo murmur characteristic of mitral valve prolapse, especially with its dynamic changes.
*Myosin heavy chain defect*
- A **myosin heavy chain defect** is a common genetic cause of **hypertrophic cardiomyopathy (HCM)**.
- HCM typically produces a **crescendo-decrescendo systolic murmur** that increases with Valsalva maneuver (due to decreased preload) and decreases with squatting (due to increased preload and afterload), but it does not feature a mid-systolic click.
Valve function during cardiac cycle US Medical PG Question 10: A 37-year-old man with a history of schizophrenia, obesity, anxiety, recurrent pneumonia, and depression is brought to the emergency department. He was recently discharged from inpatient psychiatric care where he was treated for an acute psychotic episode with fluphenazine and started on a new antidepressant. One week after discharge, during a period of cold weather, he is found outdoors confused and poorly dressed. His rectal temperature is 93.2°F (34°C). Which of the following medications is most likely contributing to his hypothermia?
- A. Fluphenazine (Correct Answer)
- B. Valproic acid
- C. Diphenhydramine
- D. Fluoxetine
- E. Lithium
Valve function during cardiac cycle Explanation: **Fluphenazine**
- **First-generation antipsychotics** like fluphenazine can impair the body's ability to **thermoregulate** by interfering with dopaminergic pathways in the hypothalamus, increasing susceptibility to hypothermia in cold environments.
- Given the patient's recent discharge from inpatient care and exposure to cold weather while poorly dressed, the addition of an antipsychotic affecting thermoregulation strongly contributes to his hypothermia.
*Valproic acid*
- Valproic acid is an **anticonvulsant** and **mood stabilizer** primarily used for bipolar disorder and epilepsy.
- While it can have various side effects, **hypothermia** is not a commonly reported or significant side effect of valproic acid.
*Diphenhydramine*
- Diphenhydramine is an **antihistamine** with significant **sedative** and **anticholinergic** properties.
- While it can cause sedation and anticholinergic effects that might impact a patient's awareness or ability to seek shelter, it is not directly implicated in causing hypothermia through thermoregulatory dysfunction.
*Fluoxetine*
- Fluoxetine is a **selective serotonin reuptake inhibitor (SSRI)** commonly used for depression and anxiety.
- While SSRIs can have various side effects, **hypothermia** is not a characteristic or significant side effect of fluoxetine.
*Lithium*
- Lithium is a **mood stabilizer** used primarily for bipolar disorder.
- **Hypothyroidism** is a known side effect of long-term lithium use, which could theoretically contribute to an inability to maintain body temperature, but it is less likely to cause acute hypothermia compared to antipsychotics directly affecting thermoregulation.
More Valve function during cardiac cycle US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.