Systolic function assessment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systolic function assessment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systolic function assessment US Medical PG Question 1: A previously healthy 19-year-old man is brought to the emergency department by his girlfriend after briefly losing consciousness. He passed out while moving furniture into her apartment. She said that he was unresponsive for a minute but regained consciousness and was not confused. The patient did not have any chest pain, palpitations, or difficulty breathing before or after the episode. He has had episodes of dizziness when exercising at the gym. His blood pressure is 125/75 mm Hg while supine and 120/70 mm Hg while standing. Pulse is 70/min while supine and 75/min while standing. On examination, there is a grade 3/6 systolic murmur at the left lower sternal border and a systolic murmur at the apex, both of which disappear with passive leg elevation. Which of the following is the most likely cause?
- A. Prolonged QT interval
- B. Hypertrophic cardiomyopathy (Correct Answer)
- C. Mitral valve stenosis
- D. Mitral valve prolapse
- E. Bicuspid aortic valve
Systolic function assessment Explanation: ***Hypertrophic cardiomyopathy***
- This patient's **syncope associated with exertion** (moving furniture) and episodes of **dizziness during exercise** are highly suggestive of hypertrophic cardiomyopathy (HCM).
- The presence of a **systolic murmur at the left sternal border and apex** that **decreases/disappears with passive leg elevation** indicates a dynamic left ventricular outflow tract (LVOT) obstruction that is sensitive to preload changes, a hallmark of HCM.
- Passive leg elevation **increases preload** → **increases LV volume** → **decreases LVOT obstruction** → **decreases murmur intensity**.
*Prolonged QT interval*
- While it can cause syncope, especially exertional, a prolonged QT interval generally **does not present with dynamic murmurs** that change with preload.
- ECG findings (not mentioned here) would be the primary diagnostic clue, not physical exam findings related to murmurs.
*Mitral valve stenosis*
- Mitral stenosis would typically present with a **diastolic murmur** (not systolic) and symptoms like dyspnea, fatigue, and possibly hemoptysis due to elevated left atrial pressure.
- The murmur of mitral stenosis would not characteristically change with passive leg elevation in the manner described.
*Mitral valve prolapse*
- Mitral valve prolapse often presents with a **mid-systolic click** followed by a systolic murmur, which typically **intensifies with standing** or maneuvers that decrease left ventricular volume.
- The murmur described here decreases with leg elevation (increased preload), which is the opposite behavior of a mitral prolapse murmur.
*Bicuspid aortic valve*
- A bicuspid aortic valve can cause an **aortic stenosis murmur** (a systolic ejection murmur heard best at the right upper sternal border) or regurgitation, but it generally **does not cause a dynamic murmur that changes with preload** in this characteristic fashion.
- Symptoms related to bicuspid aortic valve disease (like syncope) would more commonly be associated with significant stenosis, not with a murmur that is acutely sensitive to preload changes.
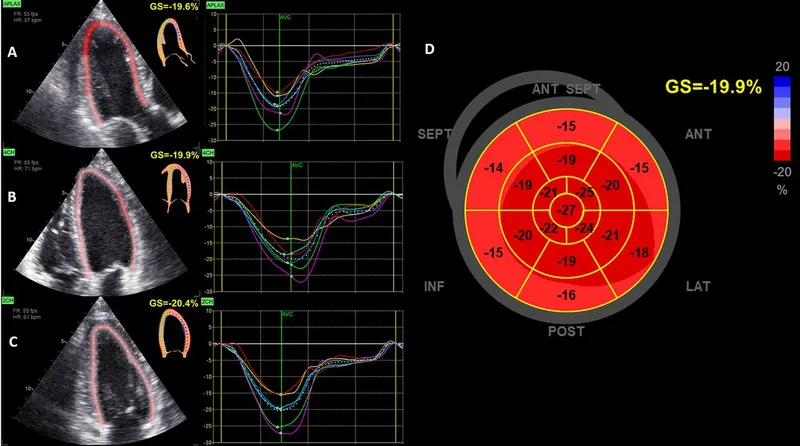
Systolic function assessment US Medical PG Question 2: A 49-year-old man presents to his physician complaining of weakness and fatigue. On exam, you note significant peripheral edema. Transthoracic echocardiogram is performed and reveals a preserved ejection fraction with impaired diastolic relaxation. A representative still image is shown in Image A. Which of the following is likely the cause of this patient's symptoms?
- A. Hemochromatosis (Correct Answer)
- B. Heavy, long-term alcohol consumption
- C. History of myocardial infarction
- D. History of a recent viral infection
- E. Previous treatment with doxorubicin
Systolic function assessment Explanation: ***Hemochromatosis***
- **Hemochromatosis** can lead to **restrictive cardiomyopathy** due to iron deposition in the myocardium, causing **diastolic dysfunction** with a **preserved ejection fraction**.
- The symptoms of **weakness**, **fatigue**, and **peripheral edema** are consistent with **heart failure** secondary to this cardiac impairment.
*Heavy, long-term alcohol consumption*
- **Alcoholic cardiomyopathy** typically presents as **dilated cardiomyopathy**, characterized by **systolic dysfunction** and a **reduced ejection fraction**, which contradicts the preserved ejection fraction seen in this patient.
- While chronic alcohol use can cause heart failure symptoms, the specific echocardiographic findings do not align with this etiology.
*History of myocardial infarction*
- A **myocardial infarction** commonly leads to **systolic dysfunction** or **ischemic cardiomyopathy**, resulting in a **reduced ejection fraction** due to scar tissue formation and impaired contractility.
- The patient's preserved ejection fraction and primary diastolic relaxation abnormality make this diagnosis less likely.
*History of a recent viral infection*
- A recent viral infection can cause **viral myocarditis**, which typically leads to **dilated cardiomyopathy** and **systolic dysfunction** with a **reduced ejection fraction**.
- The observed preserved ejection fraction and isolated diastolic relaxation impairment are not characteristic features of acute viral myocarditis.
*Previous treatment with doxorubicin*
- **Doxorubicin** (an anthracycline) is a well-known cardiotoxic agent that causes **dilated cardiomyopathy** with a **reduced ejection fraction**, primarily affecting **systolic function**.
- The patient's preserved ejection fraction makes doxorubicin-induced cardiotoxicity an unlikely cause of his current presentation.
Systolic function assessment US Medical PG Question 3: The serum brain natriuretic peptide and N-terminal pro-BNP are elevated. A diagnosis of heart failure with preserved ejection fraction is made. In addition to supplemental oxygen therapy, which of the following is the most appropriate initial step in management?
- A. Intravenous dobutamine
- B. Intravenous furosemide therapy (Correct Answer)
- C. Intravenous morphine therapy
- D. Thoracentesis
- E. Intermittent hemodialysis
Systolic function assessment Explanation: ***Intravenous furosemide therapy***
- Heart failure with **preserved ejection fraction (HFpEF)** often presents with **pulmonary congestion** due to elevated filling pressures.
- **Furosemide**, a loop diuretic, effectively reduces fluid overload and associated symptoms by increasing renal excretion of sodium and water.
*Intravenous dobutamine*
- **Dobutamine** is an inotropic agent that increases myocardial contractility and heart rate.
- It is typically used for **acute decompensated heart failure with low cardiac output** and is generally avoided in HFpEF unless there is significant hypoperfusion, as it can worsen myocardial oxygen demand and diastolic dysfunction.
*Intravenous morphine therapy*
- **Morphine** can be used in acute heart failure to reduce preload and anxiety, but it is not a primary treatment for the underlying fluid overload.
- It can cause respiratory depression and hypotension, and its use is typically reserved for patients with severe pain or dyspnea not adequately managed by other therapies.
*Thoracentesis*
- **Thoracentesis** is indicated for symptomatic **pleural effusions** causing respiratory distress.
- While pleural effusions can occur in heart failure, initial management of generalized fluid overload typically involves diuretics, making thoracentesis a secondary intervention if diuretic therapy is insufficient.
*Intermittent hemodialysis*
- **Intermittent hemodialysis** is an invasive procedure primarily used for severe renal failure or refractory fluid overload that has not responded to maximal diuretic therapy.
- It is not the initial step in managing heart failure with preserved ejection fraction and would only be considered in highly selected cases with **acute kidney injury** or diuretic resistance.
Systolic function assessment US Medical PG Question 4: A 60-year-old male engineer who complains of shortness of breath when walking a few blocks undergoes a cardiac stress test because of concern for coronary artery disease. During the test he asks his cardiologist about what variables are usually used to quantify the functioning of the heart. He learns that one of these variables is stroke volume. Which of the following scenarios would be most likely to lead to a decrease in stroke volume?
- A. Anxiety
- B. Heart failure (Correct Answer)
- C. Exercise
- D. Pregnancy
- E. Digitalis
Systolic function assessment Explanation: ***Heart failure***
- In **heart failure**, the heart's pumping ability is impaired, leading to a reduced **ejection fraction** and thus a decreased **stroke volume**.
- The weakened myocardium cannot effectively contract to expel the normal volume of blood, resulting in lower blood output per beat.
*Anxiety*
- **Anxiety** typically causes an increase in **sympathetic nervous system** activity, leading to increased heart rate and myocardial contractility.
- This often results in a temporary **increase in stroke volume** due to enhanced cardiac performance, not a decrease.
*Exercise*
- During **exercise**, there is a significant **increase in venous return** and sympathetic stimulation, leading to increased **end-diastolic volume** and contractility.
- This physiological response causes a substantial **increase in stroke volume** to meet the body's higher oxygen demands.
*Pregnancy*
- **Pregnancy** leads to significant **physiological adaptations** to accommodate the growing fetus, including a substantial increase in **blood volume**.
- This increased blood volume and cardiac output result in an **increase in stroke volume** to maintain adequate perfusion for both mother and fetus.
*Digitalis*
- **Digitalis** is a cardiac glycoside that **increases intracellular calcium** in myocardial cells, enhancing the **force of contraction**.
- This positive inotropic effect leads to an **increased stroke volume** by improving the heart's pumping efficiency.
Systolic function assessment US Medical PG Question 5: A 73-year-old woman presents to clinic with a week of fatigue, headache, and swelling of her ankles bilaterally. She reports that she can no longer go on her daily walk around her neighborhood without stopping frequently to catch her breath. At night she gets short of breath and has found that she can only sleep well in her recliner. Her past medical history is significant for hypertension and a myocardial infarction three years ago for which she had a stent placed. She is currently on hydrochlorothiazide, aspirin, and clopidogrel. She smoked 1 pack per day for 30 years before quitting 10 years ago and socially drinks around 1 drink per month. She denies any illicit drug use. Her temperature is 99.0°F (37.2°C), pulse is 115/min, respirations are 18/min, and blood pressure is 108/78 mmHg. On physical exam there is marked elevations of her neck veins, bilateral pitting edema in the lower extremities, and a 3/6 holosystolic ejection murmur over the right sternal border. Echocardiography shows the following findings:
End systolic volume (ESV): 100 mL
End diastolic volume (EDV): 160 mL
How would cardiac output be determined in this patient?
- A. 108/3 + (2 * 78)/3
- B. (160 - 100) / 160
- C. 160 - 100
- D. (160 - 100) * 115 (Correct Answer)
- E. (100 - 160) * 115
Systolic function assessment Explanation: ***(160 - 100) * 115***
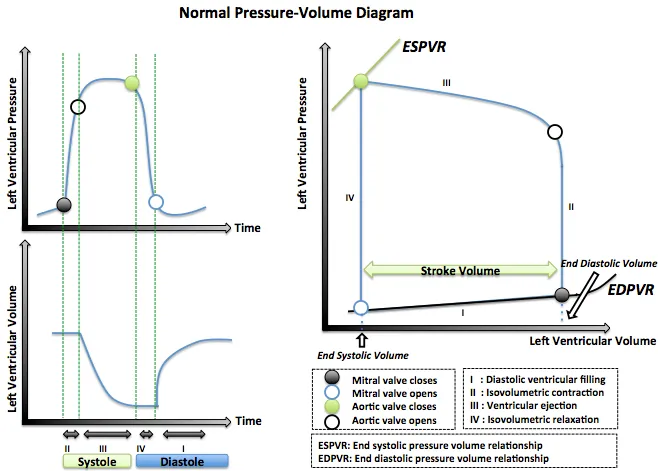
- **Cardiac output (CO)** is calculated as **stroke volume (SV) multiplied by heart rate (HR)**.
- **Stroke volume** is determined by subtracting the **end-systolic volume (ESV)** from the **end-diastolic volume (EDV)** (SV = EDV - ESV).
*(108/3 + (2 * 78)/3)*
- This formula represents the calculation for **mean arterial pressure (MAP)**, which is not directly used to determine cardiac output.
- **MAP** is approximated as (Systolic BP + 2 * Diastolic BP) / 3.
*(160 - 100) / 160*
- This formula calculates the **ejection fraction (EF)**, which is the fraction of blood pumped out of the ventricle with each beat.
- While **ejection fraction** is a crucial measure of cardiac function, it does not directly determine cardiac output.
*160 - 100*
- This calculation represents the **stroke volume (SV)** (EDV - ESV), which is the amount of blood ejected from the ventricle per beat.
- However, to get the **cardiac output**, stroke volume must be multiplied by the heart rate.
*(100 – 160) * 115*
- This calculation would result in a **negative stroke volume**, which is physiologically incorrect as stroke volume must be a positive value.
- **Stroke volume** is always calculated as the **end-diastolic volume minus the end-systolic volume**.
Systolic function assessment US Medical PG Question 6: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Systolic function assessment Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Systolic function assessment US Medical PG Question 7: A researcher is studying how electrical activity propagates across the heart. In order to do this, he decides to measure the rate at which an action potential moves within various groups of cardiac muscle tissue. In particular, he isolates fibers from areas of the heart with the following characteristics:
A) Dysfunction leads to fixed PR intervals prior to a dropped beat
B) Dysfunction leads to increasing PR intervals prior to a dropped beat
C) Dysfunction leads to tachycardia with a dramatically widened QRS complex
D) Dysfunction leads to tachycardia with a sawtooth pattern on electrocardiogram
Which of the following is the proper order of these tissues from fastest action potential propagation to slowest action potential propagation.
- A. B > D > C > A
- B. D > C > A > B
- C. B > C > D > A
- D. A > D > C > B (Correct Answer)
- E. A > C > D > B
Systolic function assessment Explanation: ***A > D > C > B***
* **Purkinje fibers (A)** have the fastest conduction velocity in the heart to ensure rapid and synchronous ventricular depolarization. The description of "fixed PR intervals prior to a dropped beat" in **Mobitz type II second-degree AV block** indicates an issue with conduction distal to the AV node, often in the His-Purkinje system, while still maintaining typical conduction through the atria and AV node for conducted beats.
* **Atrial muscle (D)** has a faster conduction velocity than the AV node but slower than Purkinje fibers. The "sawtooth pattern on electrocardiogram" unequivocally points to **atrial flutter**, which is characterized by rapid, regular depolarization of the atria.
* **Ventricular muscle (C)** has a conduction velocity slower than Purkinje fibers but faster than the AV node. "Tachycardia with a dramatically widened QRS complex" is characteristic of **ventricular tachycardia (VT)**, which arises from abnormal electrical activity within the ventricles.
* **AV node (B)** has the slowest conduction velocity in the heart, which allows for proper ventricular filling. "Increasing PR intervals prior to a dropped beat" describes **Mobitz type I second-degree AV block (Wenckebach phenomenon)**, which is due to progressive prolongation of conduction delay within the AV node itself.
*B > D > C > A*
* This order incorrectly places the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest, which is contrary to the known conduction velocities in the heart.
* The AV node is critical for delaying the impulse, making it the slowest, while Purkinje fibers are designed for rapid spread, making them the fastest.
*D > C > A > B*
* This option incorrectly places **atrial muscle (D)** as faster than **Purkinje fibers (A)**. Purkinje fibers have the fastest conduction velocity in the heart, considerably faster than atrial muscle.
*B > C > D > A*
* This arrangement incorrectly lists the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest. The AV node is the slowest for its physiological role of delaying ventricular contraction, while Purkinje fibers are optimized for rapid conduction.
*A > C > D > B*
* While placing **Purkinje fibers (A)** as the fastest and the **AV node (B)** as the slowest is correct, this order incorrectly places **ventricular muscle (C)** as faster than **atrial muscle (D)**. Atrial muscle generally conducts faster than ventricular muscle in normal physiology.
Systolic function assessment US Medical PG Question 8: Cardiac muscle serves many necessary functions, leading to a specific structure that serves these functions. The structure highlighted is an important histology component of cardiac muscle. What would be the outcome if this structure diffusely failed to function?
- A. Failure of potassium channels to appropriately open to repolarize the cell
- B. Failure of propagation of the action potential from the conduction system (Correct Answer)
- C. Ineffective excitation-contraction coupling due to insufficient calcium ions
- D. Inappropriate formation of cardiac valve leaflets
- E. Outflow tract obstruction
Systolic function assessment Explanation: ***Failure of propagation of the action potential from the conduction system***
- The highlighted structure, the **intercalated disc**, contains **gap junctions** which are crucial for the rapid, synchronized spread of **action potentials** between cardiac muscle cells.
- A diffuse failure of these structures would prevent the coordinated electrical activation of the myocardium, leading to a failure of impulse propagation and **compromised cardiac contraction**.
*Failure of potassium channels to appropriately open to repolarize the cell*
- This scenario describes a problem with **ion channel function** within individual cardiomyocytes, affecting their repolarization phase.
- While critical for a single cell's electrical activity, it does not directly relate to the primary function of **intercalated discs** in *propagating* action potentials across multiple cells.
*Ineffective excitation-contraction coupling due to insufficient calcium ions*
- This outcome would result from issues with **calcium handling** mechanisms, such as problems with the **sarcoplasmic reticulum** or **calcium channels**, which are internal to the cardiomyocyte.
- It is distinct from the role of **intercalated discs** in facilitating intercellular communication and electrical spread.
*Inappropriate formation of cardiac valve leaflets*
- The formation of cardiac valve leaflets is an intricate process during **embryological development** involving specific signaling pathways and cell migration.
- This structural defect is not directly related to the function of **intercalated discs** in mature cardiac muscle, which are involved in electrical and mechanical coupling.
*Outflow tract obstruction*
- **Outflow tract obstruction** is a congenital or acquired structural defect affecting the major arteries leaving the heart (e.g., aortic or pulmonary stenosis).
- This is a macroscopic structural anomaly that is not caused by a primary failure of **intercalated disc** function.
Systolic function assessment US Medical PG Question 9: A 36-year-old woman is admitted to the hospital for the evaluation of progressive breathlessness. She has no history of major medical illness. Her temperature is 37°C (98.6°F), pulse is 110/min, and respirations are 22/min. Pulse oximetry on room air shows an oxygen saturation of 99%. Cardiac examination shows a loud S1 and S2. There is a grade 2/6 early systolic murmur best heard in the 2nd right intercostal space. Cardiac catheterization shows a mixed venous oxygen saturation of 55% (N= 65–70%). Which of the following is the most likely cause of this patient's breathlessness?
- A. Increased peripheral shunting
- B. Decreased hemoglobin concentration
- C. Increased carbon dioxide retention
- D. Increased pulmonary vascular resistance
- E. Decreased left ventricular ejection fraction (Correct Answer)
Systolic function assessment Explanation: ***Decreased left ventricular ejection fraction***
- The key finding is a **mixed venous oxygen saturation of 55% (normal 65-70%)** with **normal arterial oxygen saturation (99%)**, which indicates **increased tissue oxygen extraction**
- Increased oxygen extraction occurs when **cardiac output is reduced** → tissues must extract more oxygen from each pass of blood to meet metabolic demands
- This is the classic physiologic compensation in **heart failure with reduced ejection fraction**
- The cardiac findings (loud heart sounds, systolic murmur) suggest underlying cardiac pathology causing reduced cardiac output and progressive breathlessness
*Increased peripheral shunting*
- Peripheral shunting (e.g., arteriovenous malformations) would cause **venous blood to bypass capillary beds**, resulting in **decreased oxygen extraction** and **higher mixed venous O2 saturation**, not lower
- Would typically cause **hypoxemia** with reduced pulse oximetry, but this patient has 99% oxygen saturation
*Decreased hemoglobin concentration*
- Anemia reduces oxygen-carrying capacity but would not explain the **low mixed venous oxygen saturation** to this degree
- The **pulse oximetry of 99%** indicates adequate oxygen saturation of available hemoglobin
- Anemia typically causes **high cardiac output** (compensatory) rather than the low cardiac output state indicated by the low mixed venous O2 saturation
*Increased carbon dioxide retention*
- **Hypercapnia** results from **hypoventilation** and impaired gas exchange, typically causing **respiratory acidosis**
- Would present with altered mental status, drowsiness, or signs of respiratory failure
- Does not explain the **low mixed venous oxygen saturation** with normal arterial oxygen saturation
- The cardiac findings point to a primary cardiac rather than respiratory problem
*Increased pulmonary vascular resistance*
- **Pulmonary hypertension** causes **right ventricular dysfunction** and can present with breathlessness and a loud P2 component of S2
- However, isolated pulmonary hypertension would not cause the same degree of **systemic oxygen extraction** increase
- The low mixed venous O2 saturation indicates **reduced systemic cardiac output**, which primarily reflects **left ventricular dysfunction** rather than isolated right-sided pathology
Systolic function assessment US Medical PG Question 10: A 72-year-old man with severe aortic regurgitation and compensated heart failure is being evaluated for surgical intervention. His echocardiogram shows LV end-diastolic dimension of 7.5 cm, ejection fraction of 45%, and severe aortic regurgitation with a regurgitant fraction of 60%. Pressure-volume loop analysis shows a markedly widened loop with increased stroke work. Evaluate the compensatory mechanisms maintaining his cardiac output and predict the timing for surgical intervention based on cardiac cycle mechanics.
- A. Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output
- B. Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction (Correct Answer)
- C. Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes
- D. Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship
- E. Surgery should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease
Systolic function assessment Explanation: ***Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction***
- In chronic **aortic regurgitation**, the ventricle undergoes **eccentric hypertrophy** to accommodate large volumes, but this patient has reached critical **LV end-diastolic dimensions** (>7.0 cm), signaling the limits of compensation.
- An **ejection fraction (EF) of 45%** in the setting of severe AR is actually indicative of **systolic dysfunction**, as guidelines generally recommend intervention when EF falls below 50-55% due to the increased total stroke volume.
*Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output*
- Waiting for the **ejection fraction** to drop to 35% is dangerous; by this stage, the **myocardial damage** is often irreversible and postoperative outcomes are significantly poorer.
- A "maintained" cardiac output is deceptive here because the **total stroke work** is massive compared to the actual **forward flow**, leading to progressive heart failure.
*Surgery is should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease*
- **Asymptomatic patients** with severe AR require surgery if they meet specific **echocardiographic triggers** (like LV dimensions or EF) to prevent sudden death and permanent LV dysfunction.
- **Pressure-volume loop** analysis and chamber dimensions are highly predictive of the transition from a **compensated** to a **decompensated** state.
*Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes*
- While severe enlargement carries higher risk, an **LVEDD of 7.5 cm** is not a contraindication but rather an **urgent indication** for valve replacement to halt further decline.
- **Irreversible remodeling** is usually associated with even lower ejection fractions and severe **congestive heart failure** symptoms that do not respond to medical therapy.
*Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship*
- **Vasodilators** (like ACE inhibitors or CCBs) can reduce afterload and improve **forward flow**, but they do not stop the mechanical progression of **valvular regurgitation** or remodeling.
- **Surgical intervention** (AVR) is the only definitive treatment for severe chronic AR once the heart shows signs of **exhausted preload reserve** and declining contractility.
More Systolic function assessment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.