Isovolumetric contraction and relaxation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Isovolumetric contraction and relaxation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
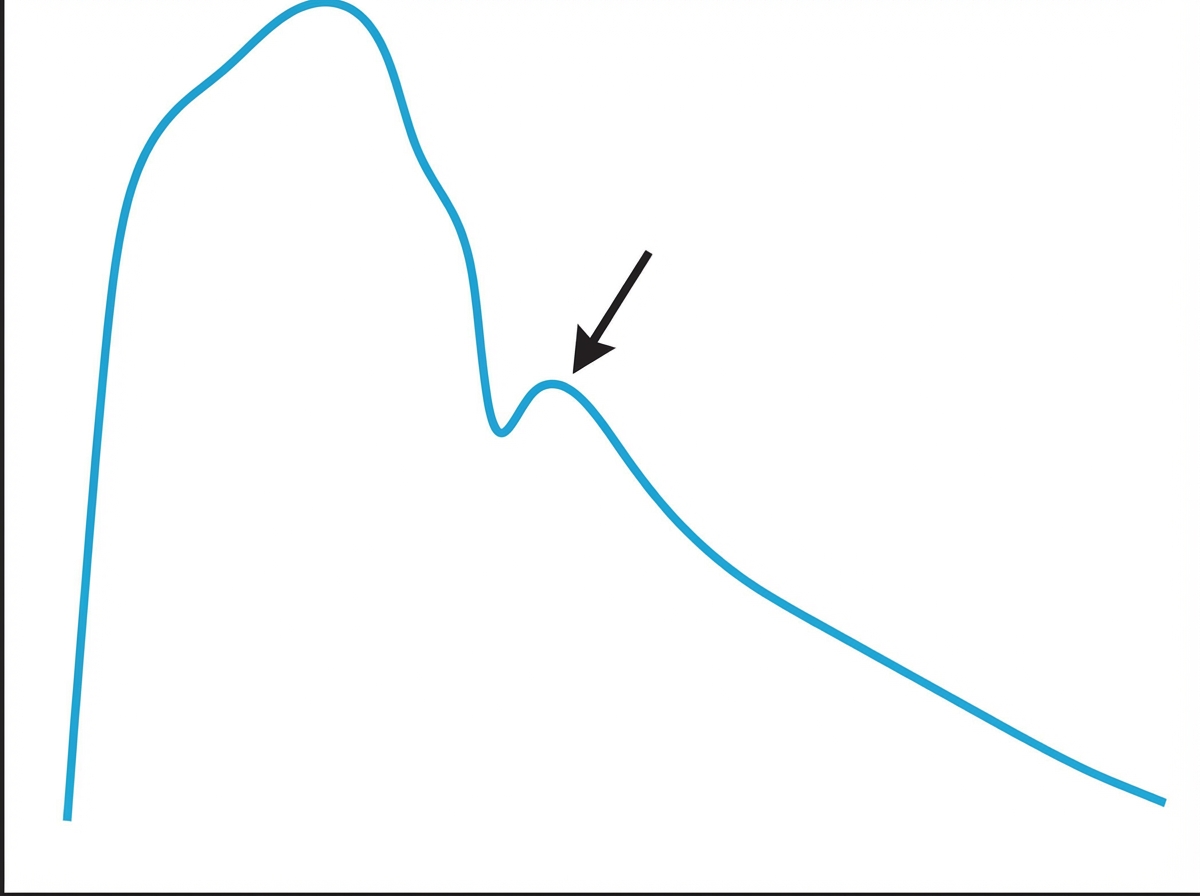
Isovolumetric contraction and relaxation US Medical PG Question 1: Prior to undergoing a total knee arthroplasty, a 62-year-old man with coronary artery disease undergoes diagnostic cardiac catheterization. The catheter is inserted via the femoral artery and then advanced to the ascending aorta. Pressure tracing of the catheter is shown. The peak marked by the arrow is most likely caused by which of the following?
- A. Left atrial contraction
- B. Closure of the aortic valve (Correct Answer)
- C. Opening of the pulmonic valve
- D. Right atrial relaxation
- E. Right ventricular contraction
Isovolumetric contraction and relaxation Explanation: ***Closure of the aortic valve***
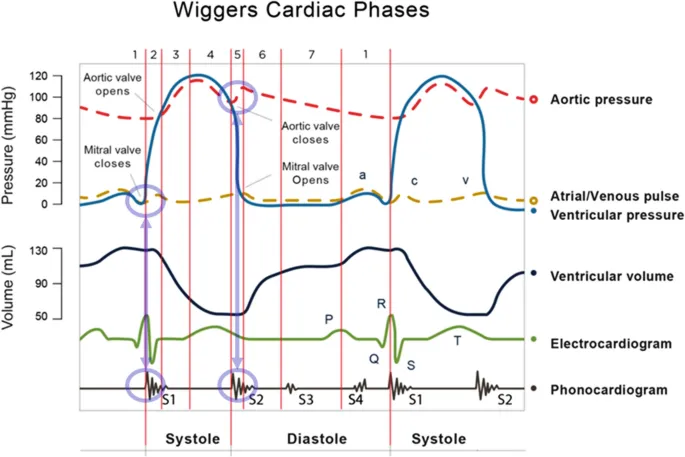
- The arrow points to the **dicrotic notch**, which marks a transient increase in aortic pressure due to the **backflow of blood** hitting the closed aortic valve, indicating the beginning of **diastole**.
- This event signifies the end of ventricular systole and the onset of ventricular relaxation, preventing regurgitation of blood into the left ventricle.
*Left atrial contraction*
- This event, responsible for the **'a' wave** in atrial pressure tracings, would occur just before ventricular systole, contributing to ventricular filling, and would not be seen as a notch in the aortic pressure tracing.
- It's a low-pressure event in the left atrium, distinct from the high-pressure changes in the aorta.
*Opening of the pulmonic valve*
- The **pulmonic valve opens** when right ventricular pressure exceeds pulmonary artery pressure, allowing blood flow into the pulmonary circulation.
- This event is unrelated to the systemic aortic pressure tracing shown and would not cause a dicrotic notch.
*Right atrial relaxation*
- **Right atrial relaxation** contributes to the 'v' wave and then the 'y' descent in venous pressure tracings as the right ventricle fills.
- This occurs during ventricular systole and is not responsible for the dicrotic notch in the systemic arterial pressure curve.
*Right ventricular contraction*
- **Right ventricular contraction** propels blood into the pulmonary artery and is not directly reflected as a pressure peak in the ascending aorta.
- The aortic pressure tracing primarily reflects events in the left ventricle and aorta.
Isovolumetric contraction and relaxation US Medical PG Question 2: A 70-year-old man presented to a medical clinic for a routine follow-up. He has had hypertension for 20 years and is currently on multiple anti-hypertensive medications. The blood pressure is 150/100 mm Hg. The remainder of the examinations were within normal limits. Echocardiography showed some changes in the left ventricle. What is the most likely reason for the change?
- A. Disordered growth of the cardiac cells
- B. Increase in number of normal cardiac cells
- C. Replacement of cardiac cells into stronger red fiber skeletal cells
- D. Decrease in cardiac cell size
- E. Increase in cardiac cell size (Correct Answer)
Isovolumetric contraction and relaxation Explanation: ***Increase in cardiac cell size***
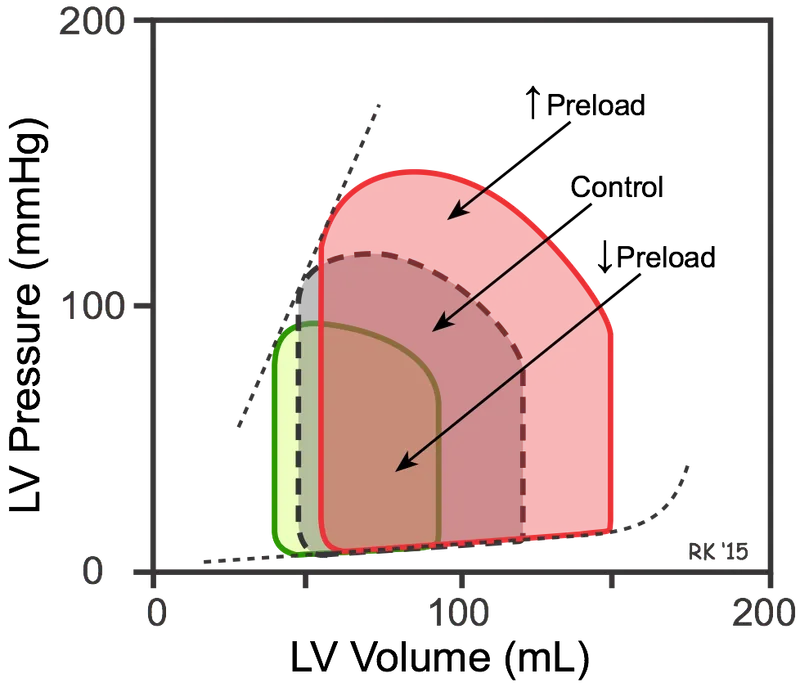
- Chronic **hypertension** increases the afterload on the left ventricle, causing the cardiac muscle cells (myocytes) to **hypertrophy** (increase in size) to generate greater force to eject blood.
- This adaptive change is a compensatory mechanism to maintain cardiac output against increased systemic vascular resistance.
*Disordered growth of the cardiac cells*
- This description typically refers to **dysplasia**, which involves abnormal cell growth and organization, often raising suspicion for pre-cancerous conditions.
- Cardiac muscle cells, being terminally differentiated, do not commonly undergo dysplastic changes in response to hypertension.
*Increase in number of normal cardiac cells*
- An increase in the number of cells is known as **hyperplasia**, a process that occurs in tissues with high regenerative capacity.
- Mature **cardiac myocytes** have very limited proliferative capacity, so an increase in their number is not the primary mechanism of ventricular adaptation to hypertension.
*Replacement of cardiac cells into stronger red fiber skeletal cells*
- This scenario describes **metaplasia**, where one differentiated cell type is replaced by another.
- Such a transformation from cardiac muscle to skeletal muscle cells does not occur in response to hypertension and is biologically impossible within the heart.
*Decrease in cardiac cell size*
- A decrease in cell size, or **atrophy**, occurs due to decreased workload, nutrition, or hormonal stimulation.
- In hypertension, the workload on the heart is significantly increased, leading to hypertrophy rather than atrophy.
Isovolumetric contraction and relaxation US Medical PG Question 3: A 27-year-old woman, who recently immigrated from Bangladesh, presents to her primary care physician to discuss birth control. During a review of her past medical history, she reports that as a child she had a recurrent sore throat and fever followed by swollen and aching hip and knee joints. These symptoms returned every season and were never treated but went away on their own only to return with the next typhoon season. When asked about any current complaints, the patient says that she sometimes has shortness of breath and palpitations that do not last long. A physical exam is performed. In which of the auscultation sites will a murmur most likely be heard in this patient?
- A. Point 5 (Correct Answer)
- B. Point 4
- C. Point 2
- D. Point 3
- E. Point 1
Isovolumetric contraction and relaxation Explanation: ***Point 5***
- The patient's history of recurrent sore throat, fever, and migratory polyarthritis (swollen and aching hip and knee joints) followed by intermittent shortness of breath and palpitations is highly suggestive of **rheumatic fever** with subsequent **rheumatic heart disease**.
- This condition most commonly affects the **mitral valve**, leading to **mitral stenosis** or regurgitation, which would produce an apical murmur heard best at point 5 (the cardiac apex).
*Point 4*
- Point 4 corresponds to the **tricuspid area** (lower left sternal border). While rheumatic heart disease can affect the tricuspid valve, it is less common than mitral valve involvement and usually occurs in conjunction with severe mitral valve disease.
- An isolated murmur here would suggest tricuspid valve pathology, which is less likely as the primary presentation in rheumatic heart disease.
*Point 2*
- Point 2 is the **pulmonic area** (left upper sternal border, second intercostal space). Murmurs heard here typically indicate pulmonary valve disease or flow murmurs.
- While pulmonary hypertension can be a complication of severe left-sided heart disease, primary pulmonic valve involvement in rheumatic heart disease is rare.
*Point 3*
- Point 3 (Erb's point, third intercostal space, left sternal border) is often used to auscultate for murmurs of **aortic regurgitation** or to hear the splitting of S2.
- While aortic valve involvement can occur in rheumatic heart disease, **mitral valve disease** is significantly more prevalent and typically presents earlier and more severely.
*Point 1*
- Point 1 is the **aortic area** (right upper sternal border, second intercostal space). Murmurs heard here are typically associated with **aortic stenosis** or regurgitation.
- Although the aortic valve can be affected by rheumatic heart disease, the mitral valve is the most commonly involved valve, making an apical murmur (Point 5) more likely for the initial and most prominent finding.
Isovolumetric contraction and relaxation US Medical PG Question 4: An 80-year-old African American male presents complaining of worsening shortness of breath that occurs during his weekly round of golf. He also notes he has been waking up at night "choking and gasping for air", though he has been able to gain some relief by propping his head on a stack of pillows before he goes to bed. Upon auscultation, a low frequency, early diastolic gallop is heard over the apex while the patient rests in the left lateral decubitus position. This finding is most consistent with which of the following?
- A. Left ventricular concentric hypertrophy
- B. Right atrial hypertrophy
- C. Mitral stenosis
- D. Left atrial hypertrophy
- E. Left ventricular eccentric hypertrophy (Correct Answer)
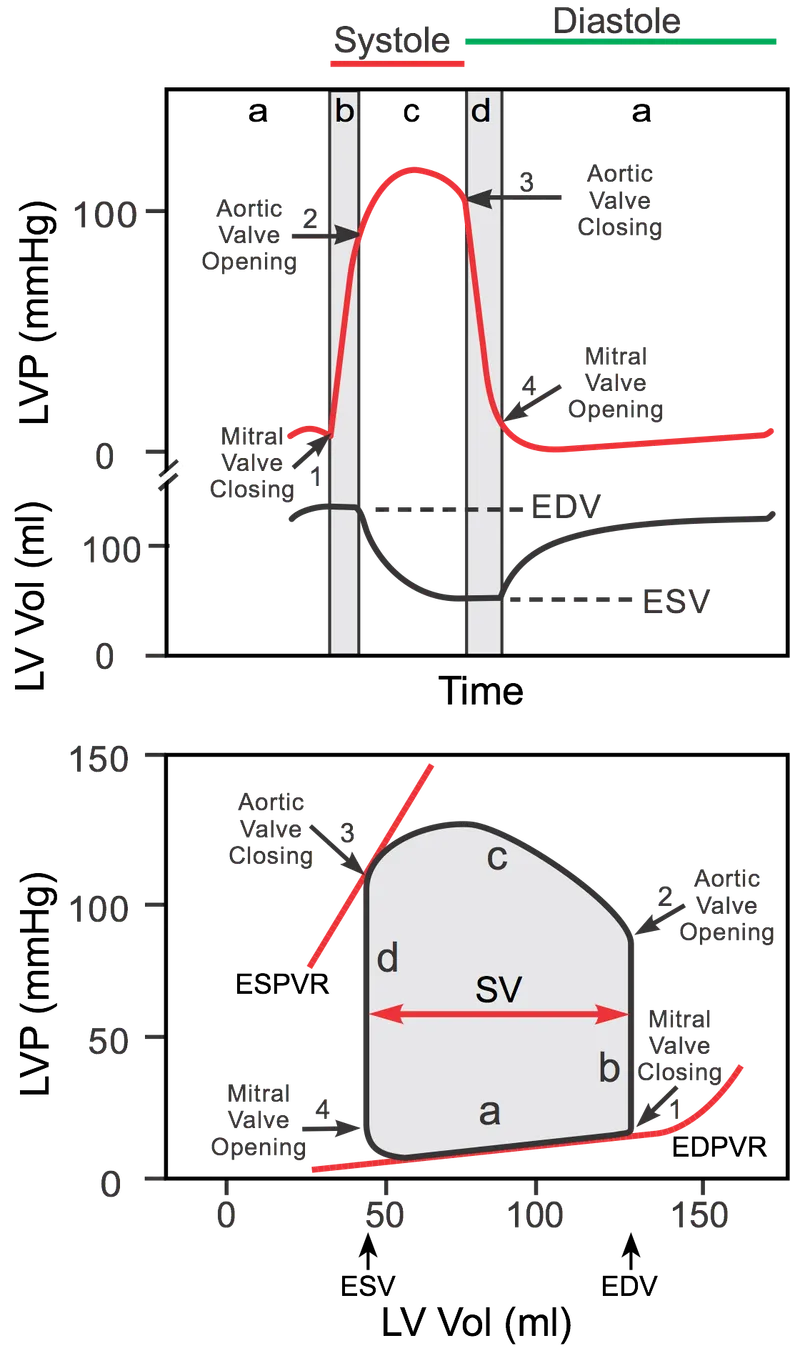
Isovolumetric contraction and relaxation Explanation: ***Left ventricular eccentric hypertrophy***
- The symptoms of **dyspnea on exertion** and **paroxysmal nocturnal dyspnea** (relieved by propping up pillows) are classic for **left-sided heart failure**.
- An **early diastolic gallop** (S3 heart sound) heard best at the apex in the left lateral decubitus position is indicative of **volume overload** and a failing, dilated left ventricle, consistent with eccentric hypertrophy.
*Left ventricular concentric hypertrophy*
- Concentric hypertrophy is typically associated with **pressure overload** (e.g., hypertension, aortic stenosis) and often presents with a **late diastolic gallop (S4)** due to a stiff, non-compliant ventricle.
- While it can lead to heart failure, the presence of an **S3 gallop** points more strongly to a dilated, volume-overloaded ventricle.
*Right atrial hypertrophy*
- Right atrial hypertrophy results from **right ventricular dysfunction** or conditions like **pulmonary hypertension** and would manifest with symptoms of right heart failure (e.g., peripheral edema, jugular venous distention), not primarily left-sided symptoms.
- It is not directly associated with a left ventricular early diastolic gallop.
*Mitral stenosis*
- Mitral stenosis typically causes a **mid-diastolic murmur** with an opening snap, and its symptoms are usually related to elevated left atrial pressure leading to pulmonary congestion and dyspnea.
- An **S3 gallop** is not characteristic of mitral stenosis; it's more specific for left ventricular systolic dysfunction.
*Left atrial hypertrophy*
- Left atrial hypertrophy (enlargement) commonly results from conditions like **mitral valve disease** or **left ventricular diastolic dysfunction** but does not directly cause an S3 gallop.
- While it contributes to symptoms of left heart failure, it's a consequence rather than the primary cause of an S3.
Isovolumetric contraction and relaxation US Medical PG Question 5: A 76-year-old male with a history of chronic uncontrolled hypertension presents to the emergency room following an episode of syncope. He reports that he felt lightheaded and experienced chest pain while walking his dog earlier in the morning. He notes that he has experienced multiple similar episodes over the past year. A trans-esophageal echocardiogram demonstrates a thickened, calcified aortic valve with left ventricular hypertrophy. Which of the following heart sounds would likely be heard on auscultation of this patient?
- A. Crescendo-decrescendo murmur radiating to the carotids that is loudest at the right upper sternal border (Correct Answer)
- B. Diastolic rumble following an opening snap with an accentuated S1
- C. Early diastolic high-pitched blowing decrescendo murmur that is loudest at the left sternal border
- D. Holosystolic murmur radiating to the axilla that is loudest at the apex
- E. Midsystolic click that is loudest at the apex
Isovolumetric contraction and relaxation Explanation: ***Crescendo-decrescendo murmur radiating to the carotids that is loudest at the right upper sternal border***
- The patient's symptoms of **syncope**, **chest pain**, and findings of a **thickened, calcified aortic valve** with **left ventricular hypertrophy** are classic for **aortic stenosis**.
- Aortic stenosis classically presents with a **systolic ejecting crescendo-decrescendo murmur** which is loudest at the **right upper sternal border**, and often **radiates to the carotids**.
*Diastolic rumble following an opening snap with an accentuated S1*
- This description is characteristic of **mitral stenosis**, which is typically caused by **rheumatic fever**.
- Mitral stenosis would present with dyspnea and fatigue, unlike the syncope and chest pain seen in this patient.
*Early diastolic high-pitched blowing decrescendo murmur that is loudest at the left sternal border*
- This murmur describes **aortic regurgitation**, where blood flows back into the left ventricle during diastole.
- While aortic regurgitation can cause heart failure symptoms, the echocardiogram shows a thickened, calcified valve more consistent with stenosis.
*Midsystolic click that is most prominent that is loudest at the apex*
- A **midsystolic click** followed by a **late systolic murmur** is characteristic of **mitral valve prolapse**.
- Symptoms of mitral valve prolapse can include atypical chest pain and palpitations, but not generally exertional syncope or the severe structural changes seen in the aortic valve.
*Holosystolic murmur radiating to the axilla that is loudest at the apex*
- This is the classic description of **mitral regurgitation**, indicating blood flow back into the left atrium during systole.
- Mitral regurgitation is associated with symptoms of heart failure and fatigue, but not usually the anginal chest pain and syncope in a patient with a calcified aortic valve.
Isovolumetric contraction and relaxation US Medical PG Question 6: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Isovolumetric contraction and relaxation Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
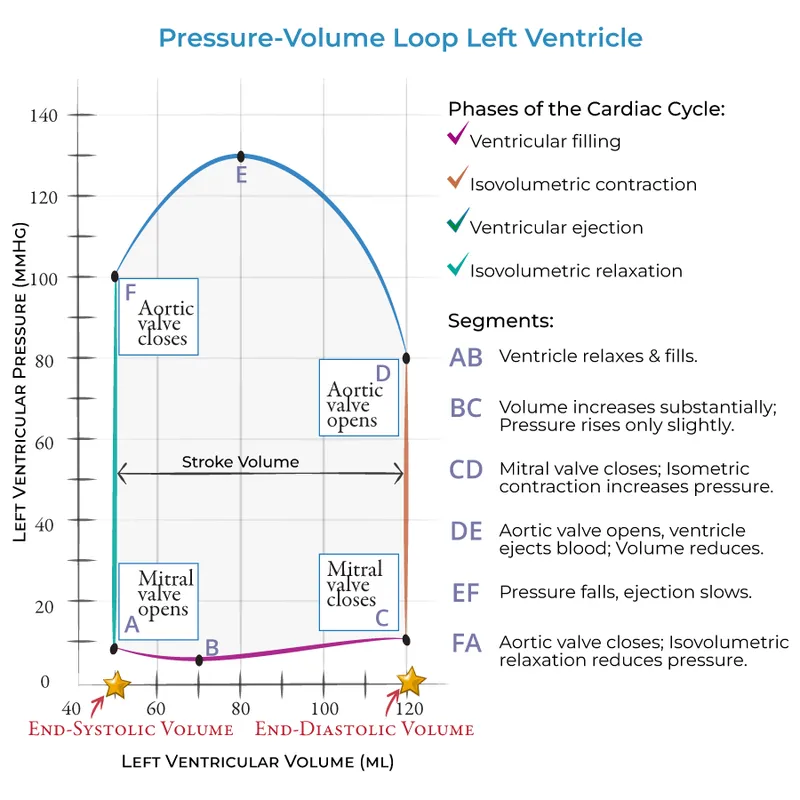
Isovolumetric contraction and relaxation US Medical PG Question 7: A 61-year-old man comes to the physician because of a 3-month history of fatigue and progressively worsening shortness of breath that is worse when lying down. Recently, he started using two pillows to avoid waking up short of breath at night. Examination shows a heart murmur. A graph with the results of cardiac catheterization is shown. Given this patient's valvular condition, which of the following murmurs is most likely to be heard on cardiac auscultation?
- A. High-frequency, diastolic murmur heard best at the 2nd left intercostal space
- B. Harsh, late systolic murmur that radiates to the carotids
- C. Blowing, early diastolic murmur heard best at the Erb point
- D. High-pitched, holosystolic murmur that radiates to the axilla (Correct Answer)
- E. Rumbling, delayed diastolic murmur heard best at the cardiac apex
Isovolumetric contraction and relaxation Explanation: ***High-pitched, holosystolic murmur that radiates to the axilla***
- The patient's symptoms of **fatigue**, **dyspnea on exertion** and **orthopnea**, combined with a heart murmur, are highly suggestive of **heart failure** caused by **mitral regurgitation**.
- A **high-pitched**, **holosystolic murmur** heard best at the **apex** and **radiating to the axilla** is the classic description of mitral regurgitation.
*High-frequency, diastolic murmur heard best at the 2nd left intercostal space*
- This describes the murmur of **pulmonary regurgitation**, which is typically heard best at the **left upper sternal border**.
- The patient's symptoms are more consistent with left-sided heart failure due to a different valvular issue.
*Harsh, late systolic murmur that radiates to the carotids*
- This is the characteristic murmur of **aortic stenosis**, which is heard best at the **right upper sternal border**.
- While aortic stenosis can cause similar symptoms, the description of the murmur and the specific context of heart failure symptoms here point away from it.
*Blowing, early diastolic murmur heard best at the Erb point*
- This describes the **diastolic murmur of aortic regurgitation**, often heard best at the **Erb's point** (3rd intercostal space, left sternal border).
- While aortic regurgitation can cause heart failure, its murmur is diastolic, not holosystolic, and the maximal intensity and radiation differ from the classic mitral regurgitation.
*Rumbling, delayed diastolic murmur heard best at the cardiac apex*
- This is the characteristic murmur of **mitral stenosis**, which is typically preceded by an **opening snap**.
- Mitral stenosis would lead to different hemodynamic changes and often presents with symptoms related to pulmonary congestion, but the murmur timing and quality are distinct from a holosystolic murmur of regurgitation.
Isovolumetric contraction and relaxation US Medical PG Question 8: A 54-year-old man is brought to the emergency department after having been hit by a car while riding his bicycle. He was not wearing a helmet. Despite appropriate life-saving measures, he dies 2 hours later because of a severe intracranial hemorrhage. Autopsy of the heart shows general thickening of the left ventricular wall with narrowing of the ventricular chamber. Which of the following conditions is the most likely underlying cause of the described cardiac changes?
- A. Sarcoidosis
- B. Chronic hypertension (Correct Answer)
- C. Chronic heavy drinking
- D. Aortic regurgitation
- E. Hemochromatosis
Isovolumetric contraction and relaxation Explanation: ***Chronic hypertension***
- **Systemic hypertension** leads to increased **afterload** on the left ventricle, causing **concentric hypertrophy** to normalize wall stress.
- This results in a thickened left ventricular wall and a **reduced ventricular chamber size**, which is a classic finding in long-standing untreated hypertension.
*Sarcoidosis*
- Cardiac sarcoidosis would typically present with **granulomatous inflammation** and could lead to **restrictive cardiomyopathy** or **conduction abnormalities**.
- It is less likely to cause isolated, generalized concentric left ventricular hypertrophy.
*Chronic heavy drinking*
- Chronic heavy alcohol consumption can cause **dilated cardiomyopathy**, characterized by ventricular dilation and systolic dysfunction.
- This is distinct from the concentric hypertrophy and narrowed chamber described.
*Aortic regurgitation*
- **Aortic regurgitation** causes **volume overload** on the left ventricle, leading to **eccentric hypertrophy** (ventricular dilation with increased wall thickness but maintained or increased chamber size).
- This is unlike the "narrowing of the ventricular chamber" seen in concentric hypertrophy.
*Hemochromatosis*
- **Hemochromatosis** causes **iron deposition** in myocardial cells, leading to **restrictive or dilated cardiomyopathy**.
- While it can cause heart failure, it typically does not present as isolated concentric hypertrophy with a narrowed chamber.
Isovolumetric contraction and relaxation US Medical PG Question 9: A 21-year-old man presents to his physician for a routine checkup. His doctor asks him if he has had any particular concerns since his last visit and if he has taken any new medications. He says that he has not been ill over the past year, except for one episode of the flu. He has been training excessively for his intercollege football tournament, which is supposed to be a huge event. His blood pressure is 110/70 mm Hg, pulse is 69/min, and respirations are 17/min. He has a heart sound coinciding with the rapid filling of the ventricles and no murmurs. He does not have any other significant physical findings. Which of the following best describes the heart sound heard in this patient?
- A. Fourth heart sound (S4)
- B. Opening snap
- C. Third heart sound (S3) (Correct Answer)
- D. Second heart sound (S2)
- E. Mid-systolic click
Isovolumetric contraction and relaxation Explanation: ***Third heart sound (S3)***
- An **S3 heart sound** is a low-pitched sound heard during **rapid ventricular filling** in early diastole, immediately after S2.
- In young, healthy individuals, especially athletes, an S3 can be a normal physiological finding, representing rapid filling of a **compliant ventricle**.
*Fourth heart sound (S4)*
- An **S4 heart sound** occurs during **atrial contraction** against a stiff or non-compliant ventricle, just before S1.
- It is typically associated with conditions like **ventricular hypertrophy** or **ischemia** and is less likely to be a normal finding in a young, healthy individual.
*Opening snap*
- An **opening snap** is a high-pitched, crisp sound heard after S2, caused by the sudden opening of a **stenotic mitral** or **tricuspid valve**.
- It indicates valvular pathology, specifically **mitral stenosis**, and is not related to ventricular filling in a healthy heart.
*Second heart sound (S2)*
- The **S2 heart sound** represents the **closure of the aortic and pulmonary valves** at the end of ventricular systole.
- While it marks the beginning of diastole, it does not coincide with the rapid filling of the ventricles itself.
*Mid-systolic click*
- A **mid-systolic click** is typically associated with **mitral valve prolapse**, caused by the sudden tensing of the chordae tendineae or valve leaflets.
- It occurs during systole, not diastole, and is not related to ventricular filling.
Isovolumetric contraction and relaxation US Medical PG Question 10: A 74-year-old man comes to the physician for a 6-month history of progressively worsening fatigue and shortness of breath on exertion. He immigrated to the United States 35 years ago from India. His pulse is 89/min and blood pressure is 145/60 mm Hg. Crackles are heard at the lung bases. Cardiac examination shows a grade 3/6 early diastolic murmur loudest at the third left intercostal space. Further evaluation of this patient is most likely to show which of the following?
- A. Paradoxical splitting of S2
- B. Pulsus paradoxus
- C. Pulsus parvus et tardus
- D. Fixed splitting of S2
- E. Water hammer pulse (Correct Answer)
Isovolumetric contraction and relaxation Explanation: ***Water hammer pulse***
- The patient's presentation with **fatigue**, **dyspnea**, **crackles**, and a **grade 3/6 early diastolic murmur** loudest at the **third left intercostal space** is highly suggestive of **aortic regurgitation (AR)**.
- A **water hammer pulse** (also known as a **Corrigan's pulse**) is a **bounding**, **collapsing pulse** characteristic of severe AR due to the rapid runoff of blood from the aorta into the left ventricle during diastole, causing a widened pulse pressure (145/60 mmHg in this case).
*Paradoxical splitting of S2*
- **Paradoxical splitting of S2** occurs when the aortic valve closes *after* the pulmonic valve, typically due to **left bundle branch block** or **severe aortic stenosis**, which are not indicated here.
- In such cases, the split narrows or disappears during inspiration.
*Pulsus paradoxus*
- **Pulsus paradoxus** is an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration, commonly seen in **cardiac tamponade**, **severe asthma**, or **constrictive pericarditis**.
- There are no features in the patient's history or examination to suggest these conditions.
*Pulsus parvus et tardus*
- **Pulsus parvus et tardus** (small and delayed pulse) is characteristic of **severe aortic stenosis**, where the pulse is weak and slow to rise due to obstruction of left ventricular outflow.
- The murmur described, an **early diastolic murmur**, is indicative of **aortic regurgitation**, not stenosis.
*Fixed splitting of S2*
- **Fixed splitting of S2** is typically associated with an **atrial septal defect (ASD)**, where the split between the aortic and pulmonic components of S2 remains constant during respiration.
- There is no clinical evidence to suggest an ASD in this patient.
More Isovolumetric contraction and relaxation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.