Heart sounds and their origin US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Heart sounds and their origin. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Heart sounds and their origin US Medical PG Question 1: A 73-year-old man presents to your clinic for a routine checkup. His medical history is notable for a previous myocardial infarction. He states that he has not seen a doctor in "many years". He has no complaints. When you auscultate over the cardiac apex with the bell of your stethoscope, you notice an additional sound immediately preceding S1. This extra heart sound is most likely indicative of which of the following processes?
- A. Decreased left ventricular compliance (Correct Answer)
- B. Increased left ventricular compliance
- C. Increased pulmonary compliance
- D. Decreased left ventricular filling volume
- E. Increased left ventricular filling volume
Heart sounds and their origin Explanation: ***Decreased left ventricular compliance***
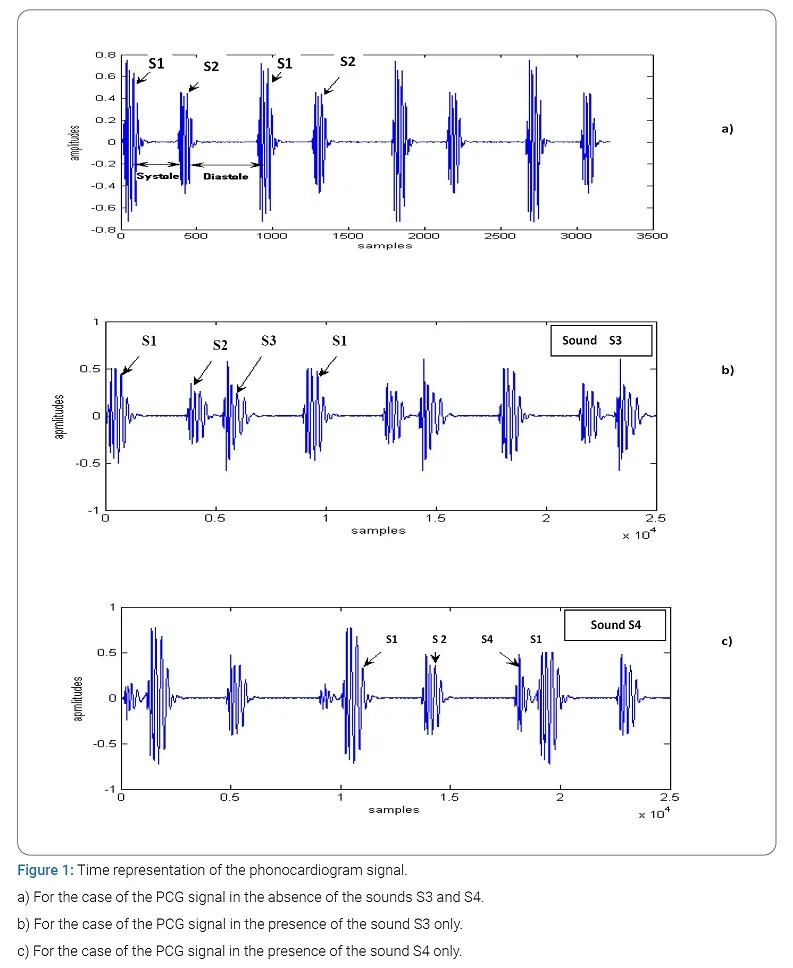
- An additional sound immediately preceding S1 suggests a **fourth heart sound (S4)**, which occurs during **atrial contraction** against a stiff, non-compliant ventricle.
- A myocardial infarction can lead to left ventricular hypertrophy and **fibrosis**, causing **decreased left ventricular compliance**.
*Increased left ventricular compliance*
- **Increased ventricular compliance** would allow for easier filling and would not generate an audible S4.
- This condition is typically seen in dilated ventricles, which accommodate larger volumes **without significant pressure increases**.
*Increased pulmonary compliance*
- **Pulmonary compliance** refers to the lungs' ability to stretch and expand, and it is unrelated to an additional heart sound preceding S1.
- This concept describes the **elastic properties of lung tissue** and has no direct bearing on cardiac auscultation in this context.
*Decreased left ventricular filling volume*
- A **decreased left ventricular filling volume** might reduce the intensity of heart sounds but would not, in itself, cause an S4 before S1.
- S4 is related to the **atrial kick** into a resistant ventricle, not the overall volume available for filling.
*Increased left ventricular filling volume*
- While increased filling volume can occur in conditions like **valvular regurgitation**, it does not directly lead to an S4.
- An S4 is specifically due to a forceful atrial contraction against a **non-compliant ventricle**, regardless of the absolute filling volume.
Heart sounds and their origin US Medical PG Question 2: A 64-year-old man presents to the emergency department because he has been experiencing increased shortness of breath for the last 2 weeks. Specifically, he says that he can barely walk up the stairs to his apartment before he feels winded. In addition, he has been waking up at night gasping for breath and has only been able to sleep propped up on 2 more pillows than usual. Physical exam reveals jugular venous distention as well as pitting lower extremity edema. Which of the following abnormal sounds will most likely be heard in this patient?
- A. Opening snap
- B. Extra heart sound in early diastole (Correct Answer)
- C. Extra heart sound in late diastole
- D. Fixed splitting
- E. Parasternal holosystolic murmur
Heart sounds and their origin Explanation: ***Extra heart sound in early diastole***
- The patient's symptoms (dyspnea, orthopnea, paroxysmal nocturnal dyspnea, jugular venous distention, edema) are classic for **congestive heart failure (CHF)**.
- An **S3 gallop** is an extra heart sound occurring in **early diastole** and is pathognomonic for **volume overload** and **ventricular dysfunction** in CHF.
*Opening snap*
- An **opening snap** is typically heard in **mitral stenosis**, which is not directly indicated by the patient's symptoms of volume overload from heart failure.
- This sound occurs shortly after S2 as the stenotic mitral valve opens.
*Extra heart sound in late diastole*
- An extra heart sound in **late diastole** is often an **S4 gallop**, which indicates **poor ventricular compliance** (e.g., in hypertension or aortic stenosis) rather than the pronounced volume overload suggested by the current presentation.
- An S4 is heard just before S1, as the atria contract to push blood into a stiff ventricle.
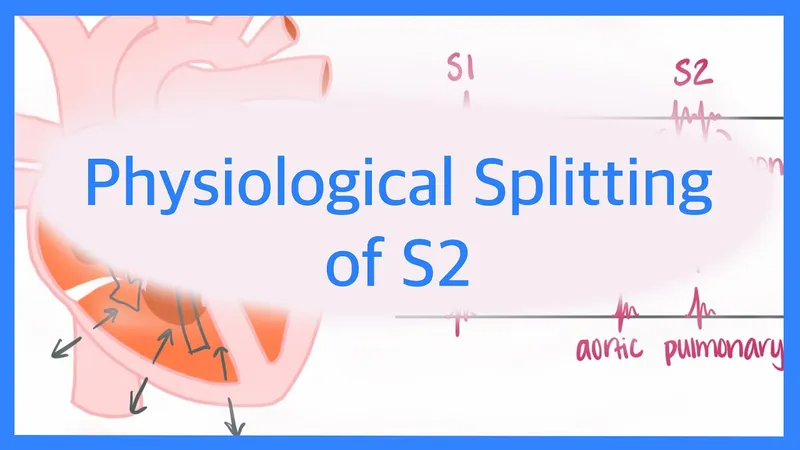
*Fixed splitting*
- **Fixed splitting of S2** is characteristic of an **atrial septal defect (ASD)**, where there is a constant delay in pulmonic valve closure, independent of respiration.
- This is not a typical finding in the context of acute decompensated heart failure as described.
*Parasternal holosystolic murmur*
- A **parasternal holosystolic murmur** is typically associated with **ventricular septal defect (VSD)** or **tricuspid regurgitation**.
- While tricuspid regurgitation can occur secondary to right heart failure, the most immediate and common auscultatory finding for overall heart failure with volume overload is an S3.
Heart sounds and their origin US Medical PG Question 3: A 31-year-old woman presents to the clinic with shortness of breath, palpitations, and fatigue. She has had these symptoms over the last several weeks. She had been tolerating these symptoms until last night when she could not fall asleep due to palpitations. She has a past medical history of infective endocarditis 6 months ago that was successfully treated with antibiotics. She does not smoke or drink alcohol. Her blood pressure is 138/89 mm Hg and her pulse is 76/min and regular. The cardiac exam reveals a soft S1, S3 gallop, a hyperdynamic apex beat, and a pansystolic murmur that radiates to the axilla on auscultation. Echocardiography reveals incompetence of one of the valves. Which of the following sites is the best position to auscultate this defect?
- A. Medial end of the 2nd intercostal space on the right side
- B. 4th intercostal space at the midclavicular line on the left side
- C. 5th intercostal space at the midclavicular line on the left side (Correct Answer)
- D. Medial end of the 2nd intercostal space on the left side
- E. Right lower end of the body of the sternum
Heart sounds and their origin Explanation: ***5th intercostal space at the midclavicular line on the left side***
- The patient's symptoms (shortness of breath, palpitations, fatigue, S3 gallop, hyperdynamic apex beat, and a pansystolic murmur radiating to the axilla) following infective endocarditis strongly suggest **mitral regurgitation**.
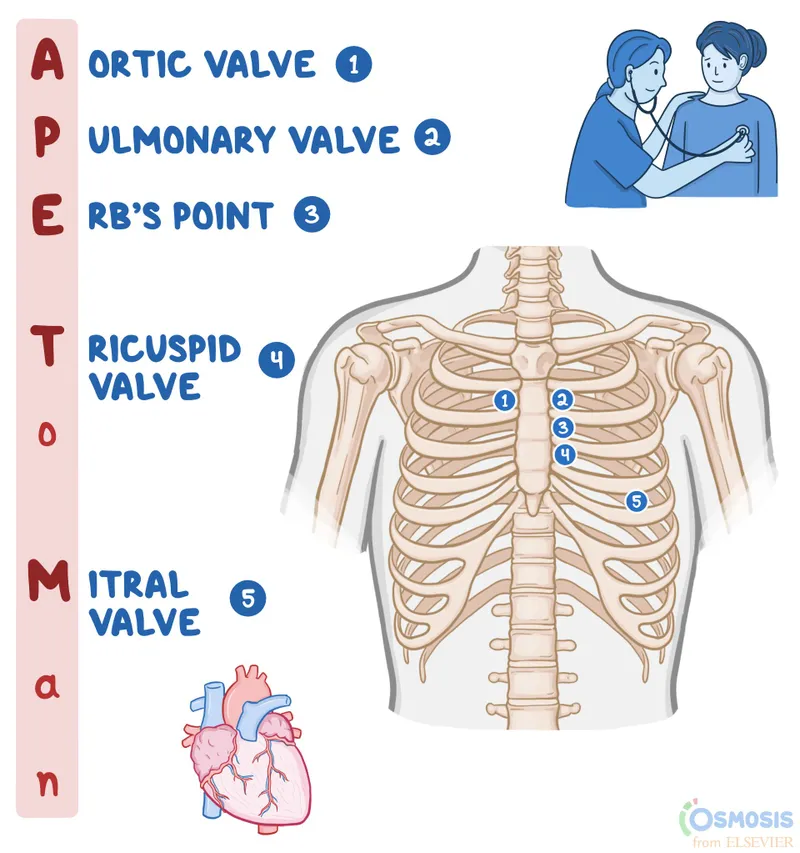
- The **mitral valve** is best auscultated at the **cardiac apex**, which is located at the **5th intercostal space at the midclavicular line on the left side**.
*Medial end of the 2nd intercostal space on the right side*
- This position is the **aortic area**, where murmurs related to the **aortic valve** (e.g., aortic stenosis or regurgitation) are best heard.
- An aortic murmur would not typically radiate to the axilla.
*4th intercostal space at the midclavicular line on the left side*
- This location is slightly above the typical apex beat and is not the primary auscultation site for any major cardiac valve.
- While close to the mitral area, it is not the optimal point for identifying mitral valve pathology.
*Medial end of the 2nd intercostal space on the left side*
- This position is the **pulmonic area**, where murmurs related to the **pulmonic valve** (e.g., pulmonary stenosis or regurgitation) are best heard.
- A pulmonic murmur would not cause a hyperdynamic apex beat or radiate to the axilla.
*Right lower end of the body of the sternum*
- This location corresponds to the **tricuspid area**, where murmurs related to the **tricuspid valve** (e.g., tricuspid regurgitation or stenosis) are best heard.
- Tricuspid murmurs are often amplified with inspiration and typically do not radiate to the axilla.
Heart sounds and their origin US Medical PG Question 4: A 21-year-old man presents to his physician for a routine checkup. His doctor asks him if he has had any particular concerns since his last visit and if he has taken any new medications. He says that he has not been ill over the past year, except for one episode of the flu. He has been training excessively for his intercollege football tournament, which is supposed to be a huge event. His blood pressure is 110/70 mm Hg, pulse is 69/min, and respirations are 17/min. He has a heart sound coinciding with the rapid filling of the ventricles and no murmurs. He does not have any other significant physical findings. Which of the following best describes the heart sound heard in this patient?
- A. Fourth heart sound (S4)
- B. Opening snap
- C. Third heart sound (S3) (Correct Answer)
- D. Second heart sound (S2)
- E. Mid-systolic click
Heart sounds and their origin Explanation: ***Third heart sound (S3)***
- An **S3 heart sound** is a low-pitched sound heard during **rapid ventricular filling** in early diastole, immediately after S2.
- In young, healthy individuals, especially athletes, an S3 can be a normal physiological finding, representing rapid filling of a **compliant ventricle**.
*Fourth heart sound (S4)*
- An **S4 heart sound** occurs during **atrial contraction** against a stiff or non-compliant ventricle, just before S1.
- It is typically associated with conditions like **ventricular hypertrophy** or **ischemia** and is less likely to be a normal finding in a young, healthy individual.
*Opening snap*
- An **opening snap** is a high-pitched, crisp sound heard after S2, caused by the sudden opening of a **stenotic mitral** or **tricuspid valve**.
- It indicates valvular pathology, specifically **mitral stenosis**, and is not related to ventricular filling in a healthy heart.
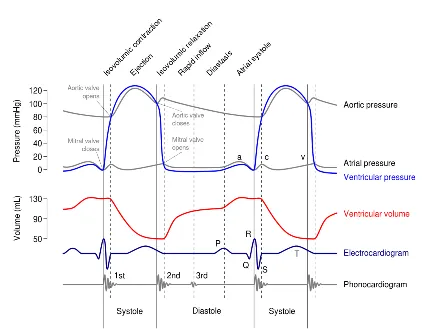
*Second heart sound (S2)*
- The **S2 heart sound** represents the **closure of the aortic and pulmonary valves** at the end of ventricular systole.
- While it marks the beginning of diastole, it does not coincide with the rapid filling of the ventricles itself.
*Mid-systolic click*
- A **mid-systolic click** is typically associated with **mitral valve prolapse**, caused by the sudden tensing of the chordae tendineae or valve leaflets.
- It occurs during systole, not diastole, and is not related to ventricular filling.
Heart sounds and their origin US Medical PG Question 5: A 74-year-old man comes to the physician for a 6-month history of progressively worsening fatigue and shortness of breath on exertion. He immigrated to the United States 35 years ago from India. His pulse is 89/min and blood pressure is 145/60 mm Hg. Crackles are heard at the lung bases. Cardiac examination shows a grade 3/6 early diastolic murmur loudest at the third left intercostal space. Further evaluation of this patient is most likely to show which of the following?
- A. Paradoxical splitting of S2
- B. Pulsus paradoxus
- C. Pulsus parvus et tardus
- D. Fixed splitting of S2
- E. Water hammer pulse (Correct Answer)
Heart sounds and their origin Explanation: ***Water hammer pulse***
- The patient's presentation with **fatigue**, **dyspnea**, **crackles**, and a **grade 3/6 early diastolic murmur** loudest at the **third left intercostal space** is highly suggestive of **aortic regurgitation (AR)**.
- A **water hammer pulse** (also known as a **Corrigan's pulse**) is a **bounding**, **collapsing pulse** characteristic of severe AR due to the rapid runoff of blood from the aorta into the left ventricle during diastole, causing a widened pulse pressure (145/60 mmHg in this case).
*Paradoxical splitting of S2*
- **Paradoxical splitting of S2** occurs when the aortic valve closes *after* the pulmonic valve, typically due to **left bundle branch block** or **severe aortic stenosis**, which are not indicated here.
- In such cases, the split narrows or disappears during inspiration.
*Pulsus paradoxus*
- **Pulsus paradoxus** is an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration, commonly seen in **cardiac tamponade**, **severe asthma**, or **constrictive pericarditis**.
- There are no features in the patient's history or examination to suggest these conditions.
*Pulsus parvus et tardus*
- **Pulsus parvus et tardus** (small and delayed pulse) is characteristic of **severe aortic stenosis**, where the pulse is weak and slow to rise due to obstruction of left ventricular outflow.
- The murmur described, an **early diastolic murmur**, is indicative of **aortic regurgitation**, not stenosis.
*Fixed splitting of S2*
- **Fixed splitting of S2** is typically associated with an **atrial septal defect (ASD)**, where the split between the aortic and pulmonic components of S2 remains constant during respiration.
- There is no clinical evidence to suggest an ASD in this patient.
Heart sounds and their origin US Medical PG Question 6: A 52-year-old man comes to the physician for a routine health maintenance examination. He has not seen a physician for 10 years. He works as a telemarketer and does not exercise. Cardiac examination shows a dull, low-pitched sound during late diastole that is best heard at the apex. The sound is loudest in the left lateral decubitus position and during end-expiration. Which of the following is the most likely cause of this finding?
- A. Fusion of mitral valve leaflets
- B. Dilation of both ventricles
- C. Concentric left ventricular hypertrophy (Correct Answer)
- D. Aortic root dilatation
- E. Right bundle branch block
Heart sounds and their origin Explanation: ***Concentric left ventricular hypertrophy***
- The described **dull, low-pitched sound** during **late diastole**, best heard at the apex in the left lateral decubitus position and during end-expiration, is consistent with a **S4 gallop**.
- An **S4 heart sound** is caused by the **atrial kick** into a **stiff, non-compliant ventricle**, which is characteristic of **concentric left ventricular hypertrophy** due to long-standing hypertension or aortic stenosis.
*Fusion of mitral valve leaflets*
- This condition, known as **mitral stenosis**, typically causes a **mid-diastolic rumble** with an opening snap, not an S4 sound.
- The associated murmur would be loudest closer to the S2 sound and might have a snapping quality.
*Dilation of both ventricles*
- **Dilated cardiomyopathy** with compromised systolic function can lead to an **S3 gallop** (early diastolic sound) due to rapid ventricular filling into an already overloaded ventricle.
- It does not typically cause an S4 sound, which is associated with ventricular stiffness.
*Aortic root dilatation*
- This can lead to **aortic regurgitation**, which is typically characterized by an **early diastolic decrescendo murmur** heard best at the left sternal border.
- It is not associated with an S4 sound.
*Right bundle branch block*
- A **right bundle branch block (RBBB)** is an electrical conduction abnormality that results in a **widely split S2 heart sound** due to delayed pulmonic valve closure.
- It does not directly produce an S4 sound, which is a mechanical event related to ventricular compliance.
Heart sounds and their origin US Medical PG Question 7: A 27-year-old male arrives in the emergency department with a stab wound over the precordial chest wall. The patient is in distress and is cold, sweaty, and pale. Initial physical examination is significant for muffled heart sounds, distended neck veins, and a 3 cm stab wound near the left sternal border. Breath sounds are present bilaterally without evidence of tracheal deviation. Which of the following additional findings would be expected on further evaluation?
- A. Decrease in central venous pressure by 5 mmHg with inspiration
- B. 15 mmHg decrease in systolic blood pressure with inspiration (Correct Answer)
- C. Decrease in the patient's heart rate by 15 beats per minute with inspiration
- D. Steadily decreasing heart rate to 60 beats per minute
- E. Elevated blood pressure to 170/110
Heart sounds and their origin Explanation: ***15 mmHg decrease in systolic blood pressure with inspiration***
- The constellation of muffled heart sounds, distended neck veins, and hypotension (implied by cold, sweaty, and pale appearance) following a precordial stab wound points to **cardiac tamponade**, an acutely life-threatening condition.
- A significant drop in systolic blood pressure (>10 mmHg) during inspiration, known as **pulsus paradoxus**, is a classic sign of cardiac tamponade as the increased venous return to the right heart during inspiration bows the interventricular septum, impinging on left ventricular filling.
*Decrease in central venous pressure by 5 mmHg with inspiration*
- In cardiac tamponade, the **central venous pressure (CVP) is typically elevated** and would not decrease significantly with inspiration due to impaired right ventricular filling.
- The elevated CVP contributes to the observed **distended neck veins**.
*Decrease in the patient's heart rate by 15 beats per minute with inspiration*
- In cardiac tamponade, the body attempts to compensate for reduced cardiac output with **reflex tachycardia**, so a decrease in heart rate is unexpected.
- Heart rate usually remains elevated or variable as the heart struggles to maintain perfusion.
*Steadily decreasing heart rate to 60 beats per minute*
- A steadily decreasing heart rate to 60 bpm (bradycardia) is contrary to the expected physiological response of **tachycardia** in cardiac tamponade as the body compensates for hypoperfusion.
- Bradycardia in this context would indicate severe decompensation and imminent cardiac arrest rather than a compensatory mechanism.
*Elevated blood pressure to 170/110*
- This patient is in **obstructive shock** due to cardiac tamponade; therefore, their blood pressure would be **hypotensive**, not hypertensive.
- **Hypotension** is a key component of Beck's triad (muffled heart sounds, distended neck veins, hypotension) which strongly suggests cardiac tamponade.
Heart sounds and their origin US Medical PG Question 8: A 45-year-old man is brought to the emergency department after a car accident with pain in the middle of his chest and some shortness of breath. He has sustained injuries to his right arm and leg. He did not lose consciousness. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 18/min, and blood pressure is 90/60 mm Hg. He is alert and oriented to person, place, and time. Examination shows several injuries to the upper extremities and chest. There are jugular venous pulsations 10 cm above the sternal angle. Heart sounds are faint on cardiac examination. The lungs are clear to auscultation. An ECG is shown. Which of the following is the most appropriate next step in management?
- A. Contrast-enhanced CT angiography
- B. Transthoracic echocardiography (Correct Answer)
- C. X-ray of the chest
- D. CT scan of the brain
- E. Contrast esophagram with gastrografin
Heart sounds and their origin Explanation: ***Transthoracic echocardiography***
- The patient's presentation with **chest pain**, shortness of breath, **hypotension**, **elevated jugular venous pressure (JVP)**, and **faint heart sounds** after trauma strongly suggests **Beck's triad**, which is classic for **cardiac tamponade**.
- **Transthoracic echocardiography** is the fastest and most accurate method to diagnose cardiac tamponade by visualizing pericardial fluid and its hemodynamic effects.
*Contrast-enhanced CT angiography*
- While CT angiography can detect vascular injuries or aortic dissection, it is not the initial diagnostic test for suspected cardiac tamponade.
- The patient's **hemodynamic instability** requires a rapid diagnostic tool to identify life-threatening conditions like tamponade.
*X-ray of the chest*
- A chest X-ray might show a **widened mediastinum** or **cardiomegaly** if there's a large effusion, but it is not sensitive enough to detect smaller effusions causing tamponade or to assess their hemodynamic impact.
- It does not provide real-time visualization of the heart and pericardium, which is crucial in this emergent setting.
*CT scan of the brain*
- A CT scan of the brain is indicated for suspected head injuries or neurological deficits, but the patient is alert and oriented, and his immediate life threat is clearly thoracic.
- Addressing the signs of cardiac tamponade takes precedence over evaluating the brain given his stable neurological status.
*Contrast esophagram with gastrografin*
- This study is used to diagnose **esophageal perforations**. While possible in significant trauma, the patient's symptoms of **Beck's triad** point specifically to cardiac tamponade, making esophageal perforation a less likely primary diagnosis and this investigation less urgent.
- It would not address the immediate, life-threatening cardiovascular compromise.
Heart sounds and their origin US Medical PG Question 9: A 65-year-old woman comes to the physician because of a 3-month history of intermittent palpitations and shortness of breath. Cardiopulmonary examination shows no other abnormalities. An ECG shows an absence of P waves, an oscillating baseline, and irregular RR intervals at a rate of approximately 95 beats per minute. The difference between atrial and ventricular rates in this patient is most likely due to which of the following?
- A. Prolonged influx through voltage-gated Ca2+ channels in the bundle of His
- B. Transient activation of K+ current in Purkinje fibers
- C. Inhibition of the Na+/K+-ATPase pump in ventricular cells
- D. Limited speed of conduction through the left bundle branch
- E. Temporary inactivation of Na+ channels in the AV node (Correct Answer)
Heart sounds and their origin Explanation: ***Temporary inactivation of Na+ channels in the AV node***
- The ECG findings are classic for **atrial fibrillation**, characterized by a rapid, irregular atrial rhythm (oscillating baseline with no P waves) and an irregularly irregular ventricular response.
- The **AV node's refractory period** and the number of sodium channels available for conduction dictate the rate at which atrial impulses can pass to the ventricles, preventing a dangerously fast ventricular rate.
*Prolonged influx through voltage-gated Ca2+ channels in the bundle of His*
- The **bundle of His** primarily conducts impulses rather than primarily regulating the rate difference between atria and ventricles through calcium channel kinetics.
- Prolonged calcium influx would generally **slow conduction** or decrease excitability, but it's not the primary mechanism explaining the ventricular rate control in atrial fibrillation.
*Transient activation of K+ current in Purkinje fibers*
- **Purkinje fibers** are involved in rapid ventricular depolarization, but their primary role is not to mediate the rate difference between atria and ventricles in atrial fibrillation.
- Activation of K+ current typically leads to **repolarization**, affecting action potential duration, not the overall filtering of atrial impulses.
*Inhibition of the Na+/K+-ATPase pump in ventricular cells*
- Inhibition of the **Na+/K+-ATPase pump** would lead to intracellular sodium accumulation and depolarization, potentially causing arrhythmias, not regulating the ventricular rate in atrial fibrillation.
- This is the mechanism of action for **digoxin**, which can slow AV nodal conduction but through a different primary pathway affecting the pump.
*Limited speed of conduction through the left bundle branch*
- While conduction system abnormalities can occur, a **limited speed of conduction** specifically in the left bundle branch would cause a wide QRS complex or bundle branch block, not the inherent rate-limiting seen in atrial fibrillation.
- The AV node is the primary regulator of ventricular response rate in atrial fibrillation due to its inherent physiological properties.
Heart sounds and their origin US Medical PG Question 10: A 72-year-old man with severe aortic regurgitation and compensated heart failure is being evaluated for surgical intervention. His echocardiogram shows LV end-diastolic dimension of 7.5 cm, ejection fraction of 45%, and severe aortic regurgitation with a regurgitant fraction of 60%. Pressure-volume loop analysis shows a markedly widened loop with increased stroke work. Evaluate the compensatory mechanisms maintaining his cardiac output and predict the timing for surgical intervention based on cardiac cycle mechanics.
- A. Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output
- B. Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction (Correct Answer)
- C. Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes
- D. Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship
- E. Surgery should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease
Heart sounds and their origin Explanation: ***Surgery is indicated now because the increased stroke work indicates the ventricle is operating at near-maximal preload reserve with impending decompensation despite preserved ejection fraction***
- In chronic **aortic regurgitation**, the ventricle undergoes **eccentric hypertrophy** to accommodate large volumes, but this patient has reached critical **LV end-diastolic dimensions** (>7.0 cm), signaling the limits of compensation.
- An **ejection fraction (EF) of 45%** in the setting of severe AR is actually indicative of **systolic dysfunction**, as guidelines generally recommend intervention when EF falls below 50-55% due to the increased total stroke volume.
*Surgery should be delayed until ejection fraction falls below 35% because current compensatory mechanisms are adequate as evidenced by maintained cardiac output*
- Waiting for the **ejection fraction** to drop to 35% is dangerous; by this stage, the **myocardial damage** is often irreversible and postoperative outcomes are significantly poorer.
- A "maintained" cardiac output is deceptive here because the **total stroke work** is massive compared to the actual **forward flow**, leading to progressive heart failure.
*Surgery is should wait until symptoms develop because pressure-volume loop changes alone do not predict outcomes in valvular disease*
- **Asymptomatic patients** with severe AR require surgery if they meet specific **echocardiographic triggers** (like LV dimensions or EF) to prevent sudden death and permanent LV dysfunction.
- **Pressure-volume loop** analysis and chamber dimensions are highly predictive of the transition from a **compensated** to a **decompensated** state.
*Surgery is contraindicated due to excessive left ventricular dimensions indicating irreversible remodeling with poor surgical outcomes*
- While severe enlargement carries higher risk, an **LVEDD of 7.5 cm** is not a contraindication but rather an **urgent indication** for valve replacement to halt further decline.
- **Irreversible remodeling** is usually associated with even lower ejection fractions and severe **congestive heart failure** symptoms that do not respond to medical therapy.
*Medical management with vasodilators should continue indefinitely because reduced afterload optimizes the pressure-volume relationship*
- **Vasodilators** (like ACE inhibitors or CCBs) can reduce afterload and improve **forward flow**, but they do not stop the mechanical progression of **valvular regurgitation** or remodeling.
- **Surgical intervention** (AVR) is the only definitive treatment for severe chronic AR once the heart shows signs of **exhausted preload reserve** and declining contractility.
More Heart sounds and their origin US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.