Effects of heart rate on cardiac cycle US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Effects of heart rate on cardiac cycle. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Effects of heart rate on cardiac cycle US Medical PG Question 1: A woman with coronary artery disease is starting to go for a walk. As she begins, her heart rate accelerates from a resting pulse of 60 bpm until it reaches a rate of 120 bpm, at which point she begins to feel a tightening in her chest. She stops walking to rest and the tightening resolves. This has been happening to her consistently for the last 6 months. Which of the following is a true statement?
- A. This patient's chest pain is indicative of transmural ischemia
- B. Perfusion of the myocardium takes place equally throughout the cardiac cycle
- C. Increasing the heart rate increases the amount of time spent during each cardiac cycle
- D. Increasing the heart rate decreases the relative amount of time spent during diastole (Correct Answer)
- E. Perfusion of the myocardium takes place primarily during systole
Effects of heart rate on cardiac cycle Explanation: ***Increasing the heart rate decreases the relative amount of time spent during diastole***
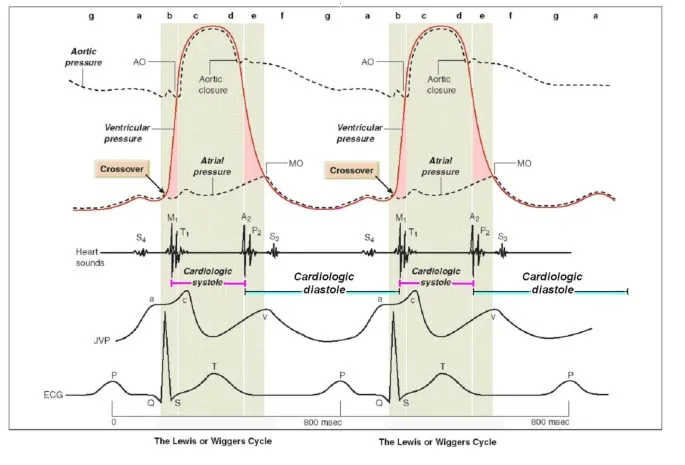
- With increasing heart rate, the **duration of the cardiac cycle decreases**, but this reduction is disproportionately greater in **diastole (filling phase)** compared to systole (ejection phase), which becomes critical in patients with coronary artery disease as myocardial perfusion occurs during diastole.
- Reduced diastolic time means less time for **coronary artery filling** and **myocardial perfusion**, exacerbating ischemia in the presence of fixed coronary stenosis.
*This patient's chest pain is indicative of transmural ischemia*
- The patient's symptoms are consistent with **stable angina**, characterized by chest pain with exertion that resolves with rest, suggesting **subendocardial ischemia** rather than transmural.
- **Transmural ischemia** typically indicates a more severe, often prolonged, and extensive reduction in blood flow, such as in a **ST-elevation myocardial infarction (STEMI)**.
*Perfusion of the myocardium takes place equally throughout the cardiac cycle*
- Myocardial perfusion is **not equal throughout the cardiac cycle**; it primarily occurs during **diastole** when the heart muscle is relaxed and coronary arteries are less compressed.
- During **systole**, the contracting myocardium compresses the coronary arteries, restricting blood flow, especially to the **subendocardial layers**.
*Increasing the heart rate increases the amount of time spent during each cardiac cycle*
- **Increasing heart rate** by definition **decreases the total duration of each cardiac cycle** (e.g., if heart rate is 60 bpm, cycle duration is 1 second; if 120 bpm, cycle duration is 0.5 seconds).
- While both systole and diastole shorten, the **diastolic phase shortens more significantly**, which is problematic for myocardial perfusion.
*Perfusion of the myocardium takes place primarily during systole*
- **Myocardial perfusion primarily occurs during diastole**, not systole, because the **intramyocardial pressure is lower** and the coronary arteries are less compressed, allowing for better blood flow.
- During **systole**, the high intramyocardial pressure, especially in the left ventricular wall, compresses the coronary vessels, significantly reducing blood flow to the myocardium.
Effects of heart rate on cardiac cycle US Medical PG Question 2: A 37-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He suffered multiple deep lacerations and experienced significant blood loss during transport. In the emergency department, his temperature is 98.6°F (37°C), blood pressure is 102/68 mmHg, pulse is 112/min, and respirations are 22/min. His lacerations are sutured and he is given 2 liters of saline by large bore intravenous lines. Which of the following changes will occur in this patient's cardiac physiology due to this intervention?
- A. Increased cardiac output and unchanged right atrial pressure
- B. Decreased cardiac output and increased right atrial pressure
- C. Increased cardiac output and decreased right atrial pressure
- D. Increased cardiac output and increased right atrial pressure (Correct Answer)
- E. Decreased cardiac output and decreased right atrial pressure
Effects of heart rate on cardiac cycle Explanation: ***Increased cardiac output and increased right atrial pressure***
- The patient experienced significant blood loss, leading to a **decreased preload** and subsequent **reduced cardiac output**. Volume resuscitation with saline directly increases the **intravascular volume** which bolsters **venous return** and **right atrial pressure**.
- According to the **Frank-Starling mechanism**, increased right atrial pressure (a measure of preload) results in an increase in ventricular stretch and a more forceful contraction, thereby increasing **stroke volume** and **cardiac output**.
*Increased cardiac output and unchanged right atrial pressure*
- While fluid administration will increase **cardiac output** by improving preload, it will also directly lead to an increase in **right atrial pressure** due to the augmented venous return.
- An unchanged right atrial pressure would imply no significant increase in central venous volume, which contradicts the effect of a large volume fluid resuscitation.
*Decreased cardiac output and increased right atrial pressure*
- This scenario is unlikely because increasing **intravascular volume** through fluid resuscitation typically aims to raise **cardiac output** by optimizing preload, not decrease it.
- A decrease in cardiac output despite increased right atrial pressure could indicate **cardiac pump failure**, which is not suggested by the clinical picture of hypovolemic shock treated with fluids.
*Increased cardiac output and decreased right atrial pressure*
- An increase in **cardiac output** as a result of fluid resuscitation is expected, but a **decreased right atrial pressure** would contradict the mechanism of increased venous return and volume expansion.
- Decreased right atrial pressure would typically indicate ongoing volume loss or inadequate fluid resuscitation to restore central venous volume.
*Decreased cardiac output and decreased right atrial pressure*
- Both decreasing **cardiac output** and decreasing **right atrial pressure** indicate a worsening state of **hypovolemia** or an inadequate response to fluid resuscitation.
- The administration of 2 liters of saline is intended to correct the hypovolemia and improve cardiodynamics, not to worsen them.
Effects of heart rate on cardiac cycle US Medical PG Question 3: Which factor most strongly influences coronary blood flow during exercise?
- A. Endothelin release
- B. Metabolic demand (Correct Answer)
- C. Myogenic response
- D. Neural regulation
- E. Baroreceptor reflex
Effects of heart rate on cardiac cycle Explanation: **Metabolic demand**
- During exercise, increased **myocardial activity** leads to a higher demand for oxygen and nutrients, prompting a significant increase in coronary blood flow.
- Local release of **metabolites** such as adenosine, nitric oxide, and hydrogen ions causes powerful vasodilation of coronary arteries, closely matching blood supply to demand.
*Endothelin release*
- **Endothelin** is a potent vasoconstrictor and plays a role in regulating vascular tone, but its primary influence is not the immediate or strongest factor dictating increased coronary flow during exercise.
- While it can modulate flow, metabolic changes are the dominant driver for the rapid and substantial increases needed during exertion.
*Myogenic response*
- The **myogenic response** is an intrinsic property of vascular smooth muscle cells to contract when stretched (due to increased pressure) and relax when pressure decreases, helping to maintain relatively constant blood flow.
- This mechanism primarily contributes to **autoregulation** and flow stability, but it does not account for the massive increase in flow required by the heart during exercise.
*Neural regulation*
- **Neural regulation**, primarily sympathetic stimulation, increases heart rate and contractility, which indirectly increases metabolic demand.
- However, direct neural effects on coronary arteries can be complex (both vasodilation and vasoconstriction depending on receptor type), and the overriding control during exercise is typically metabolic.
Effects of heart rate on cardiac cycle US Medical PG Question 4: A 67-year-old woman comes to the physician because of intermittent chest pain and dizziness on exertion for 6 months. Her pulse is 76/min and blood pressure is 125/82 mm Hg. Cardiac examination shows a grade 3/6, late-peaking, crescendo-decrescendo murmur heard best at the right upper sternal border. An echocardiogram confirms the diagnosis. Three months later, the patient returns to the physician with worsening shortness of breath for 2 weeks. An ECG is shown. Which of the following changes is most likely responsible for this patient's acute exacerbation of symptoms?
- A. Impaired pulmonary artery outflow
- B. Increased systemic vascular resistance
- C. Decreased left ventricular preload (Correct Answer)
- D. Impaired contractility of the left ventricle
- E. Decreased impulse conduction across the AV node
Effects of heart rate on cardiac cycle Explanation: ***Decreased left ventricular preload***
- The ECG shows **atrial fibrillation** (irregularly irregular rhythm, absence of P waves), which significantly reduces **atrial kick**.
- In a patient with **aortic stenosis** (suggested by the murmur and symptoms), maintaining adequate left ventricular preload is crucial, and its reduction due to atrial fibrillation can acutely worsen symptoms by decreasing cardiac output.
*Impaired pulmonary artery outflow*
- This condition, typically seen in **pulmonary hypertension** or **pulmonic stenosis**, primarily affects the right side of the heart.
- The patient's presentation with a murmur heard best at the **right upper sternal border** and systemic symptoms points towards left-sided heart disease, specifically aortic stenosis.
*Increased systemic vascular resistance*
- While increased afterload can exacerbate heart failure, the primary issue suggested by the ECG (atrial fibrillation) specifically impacts **preload** rather than systemic vascular resistance directly.
- There is no information provided that would indicate an acute increase in afterload.
*Impaired contractility of the left ventricle*
- While impaired contractility can lead to shortness of breath, the acute change shown in the ECG is **atrial fibrillation**, which primarily affects **diastolic filling** (preload) rather than the contractile function of the ventricle itself.
- Aortic stenosis primarily causes **pressure overload**, leading to concentric hypertrophy, and contractility may be preserved initially.
*Decreased impulse conduction across the AV node*
- This would result in a slower heart rate (e.g., **bradycardia** or **heart block**), not the irregularly irregular rhythm characteristic of atrial fibrillation.
- Atrial fibrillation in fact involves rapid and chaotic atrial activity with variable AV nodal conduction, leading to a rapid, irregular ventricular response.
Effects of heart rate on cardiac cycle US Medical PG Question 5: Which neurotransmitter is primarily responsible for parasympathetic effects on heart rate?
- A. Norepinephrine
- B. Dopamine
- C. Acetylcholine (Correct Answer)
- D. Epinephrine
Effects of heart rate on cardiac cycle Explanation: ***Acetylcholine***
- **Acetylcholine** is the primary neurotransmitter released by postganglionic parasympathetic neurons.
- It acts on **muscarinic receptors** (M2 receptors) in the heart to decrease heart rate.
*Norepinephrine*
- **Norepinephrine** is primarily associated with the **sympathetic nervous system**, increasing heart rate and contractility.
- It acts on **beta-1 adrenergic receptors** in the heart.
*Dopamine*
- **Dopamine** is a precursor to norepinephrine and epinephrine, and primarily functions as a neurotransmitter in the **central nervous system** and in regulating renal blood flow.
- While it can have cardiac effects, it is not the primary neurotransmitter for parasympathetic actions on heart rate.
*Epinephrine*
- **Epinephrine** (adrenaline) is a hormone released by the adrenal medulla and a neurotransmitter in the sympathetic nervous system, causing an **increase in heart rate** and contractility.
- It works through **beta-1 adrenergic receptors**, antagonistic to parasympathetic effects.
Effects of heart rate on cardiac cycle US Medical PG Question 6: A 27-year-old man is running on the treadmill at his gym. His blood pressure prior to beginning his workout was 110/72. Which of the following changes in his cardiovascular system may be seen in this man now that he is exercising?
- A. Decreased blood pressure
- B. Decreased systemic vascular resistance (Correct Answer)
- C. Increased systemic vascular resistance
- D. Decreased stroke volume
- E. Decreased heart rate
Effects of heart rate on cardiac cycle Explanation: ***Decreased systemic vascular resistance***
- During dynamic exercise, metabolic vasodilation in exercising muscles leads to a substantial **decrease in systemic vascular resistance (SVR)** to accommodate increased blood flow.
- This vasodilation overrides the systemic vasoconstriction driven by the sympathetic nervous system, resulting in a net decrease in overall SVR.
*Decreased blood pressure*
- While SVR decreases, **systolic blood pressure typically increases** during exercise due to increased cardiac output.
- **Diastolic blood pressure** usually remains stable or may slightly decrease, but overall blood pressure, specifically the mean arterial pressure, is generally maintained or elevated.
*Increased systemic vascular resistance*
- This is incorrect as **vasodilation in active muscles** causes a significant decrease in overall systemic vascular resistance.
- An increase in SVR would typically hinder blood flow to working muscles and is not a characteristic cardiovascular response to dynamic exercise.
*Decreased stroke volume*
- Stroke volume generally **increases significantly** during exercise due to enhanced venous return, increased contractility, and reduced afterload (from decreased SVR).
- A decreased stroke volume would limit cardiac output and exercise performance.
*Decreased heart rate*
- Heart rate **increases proportionally with exercise intensity** to boost cardiac output and oxygen delivery to active muscles.
- A decreased heart rate would counteract the body's physiological demand for increased blood flow during physical activity.
Effects of heart rate on cardiac cycle US Medical PG Question 7: A 73-year-old woman presents to clinic with a week of fatigue, headache, and swelling of her ankles bilaterally. She reports that she can no longer go on her daily walk around her neighborhood without stopping frequently to catch her breath. At night she gets short of breath and has found that she can only sleep well in her recliner. Her past medical history is significant for hypertension and a myocardial infarction three years ago for which she had a stent placed. She is currently on hydrochlorothiazide, aspirin, and clopidogrel. She smoked 1 pack per day for 30 years before quitting 10 years ago and socially drinks around 1 drink per month. She denies any illicit drug use. Her temperature is 99.0°F (37.2°C), pulse is 115/min, respirations are 18/min, and blood pressure is 108/78 mmHg. On physical exam there is marked elevations of her neck veins, bilateral pitting edema in the lower extremities, and a 3/6 holosystolic ejection murmur over the right sternal border. Echocardiography shows the following findings:
End systolic volume (ESV): 100 mL
End diastolic volume (EDV): 160 mL
How would cardiac output be determined in this patient?
- A. 108/3 + (2 * 78)/3
- B. (160 - 100) / 160
- C. 160 - 100
- D. (160 - 100) * 115 (Correct Answer)
- E. (100 - 160) * 115
Effects of heart rate on cardiac cycle Explanation: ***(160 - 100) * 115***
- **Cardiac output (CO)** is calculated as **stroke volume (SV) multiplied by heart rate (HR)**.
- **Stroke volume** is determined by subtracting the **end-systolic volume (ESV)** from the **end-diastolic volume (EDV)** (SV = EDV - ESV).
*(108/3 + (2 * 78)/3)*
- This formula represents the calculation for **mean arterial pressure (MAP)**, which is not directly used to determine cardiac output.
- **MAP** is approximated as (Systolic BP + 2 * Diastolic BP) / 3.
*(160 - 100) / 160*
- This formula calculates the **ejection fraction (EF)**, which is the fraction of blood pumped out of the ventricle with each beat.
- While **ejection fraction** is a crucial measure of cardiac function, it does not directly determine cardiac output.
*160 - 100*
- This calculation represents the **stroke volume (SV)** (EDV - ESV), which is the amount of blood ejected from the ventricle per beat.
- However, to get the **cardiac output**, stroke volume must be multiplied by the heart rate.
*(100 – 160) * 115*
- This calculation would result in a **negative stroke volume**, which is physiologically incorrect as stroke volume must be a positive value.
- **Stroke volume** is always calculated as the **end-diastolic volume minus the end-systolic volume**.
Effects of heart rate on cardiac cycle US Medical PG Question 8: A 35-year-old man presents to the physician’s clinic due to episodic chest pain over the last couple of months. He is currently pain-free. His chest pain occurs soon after he starts to exercise, and it is rapidly relieved by rest. He recently started training for a marathon after a decade of a fairly sedentary lifestyle. He was a competitive runner during his college years, but he has only had occasional exercise since then. He is concerned that he might be developing some heart disease. He has no prior medical issues and takes no medications. The family history is significant for hypertension and myocardial infarction in his father. His vital signs include: pulse 74/min, respirations 10/min, and blood pressure 120/74 mm Hg. The ECG test is normal. The physician orders an exercise tolerance test that has to be stopped after 5 minutes due to the onset of chest pain. Which of the following contributes most to the decreasing cardiac perfusion in this patient's heart?
- A. Ventricular blood volume
- B. Force of myocardial contraction
- C. Duration of diastole (Correct Answer)
- D. Coronary vasoconstriction
- E. Diastolic aortic pressure
Effects of heart rate on cardiac cycle Explanation: ***Duration of diastole***
- As heart rate increases during exercise, the **duration of diastole** decreases significantly because systole duration is relatively fixed.
- The majority of **coronary artery blood flow** to the left ventricle occurs during diastole, so a shortened diastole reduces the time available for myocardial perfusion, especially when oxygen demand is high.
*Ventricular blood volume*
- **Ventricular blood volume** (preload) generally increases with exercise due to enhanced venous return, which would typically increase stroke volume and cardiac output, not directly decrease cardiac perfusion in the coronary arteries.
- While extreme volume overload can stress the heart, it is not the primary factor limiting perfusion in a patient with exercise-induced chest pain indicative of ischemia.
*Force of myocardial contraction*
- An increased **force of myocardial contraction** (contractility) during exercise raises the heart's oxygen demand because the heart has to work harder.
- While increased contractility contributes to higher oxygen demand, it does not directly *decrease* the supply of blood (perfusion) to the heart muscle itself; rather, it highlights the inadequacy of existing perfusion.
*Coronary vasoconstriction*
- While **coronary vasoconstriction** can reduce blood flow, in this patient with exercise-induced chest pain, the primary issue is likely **fixed atherosclerotic plaques** that prevent adequate vasodilation with increased demand.
- *Primary* coronary vasoconstriction is characteristic of conditions like **Prinzmetal angina**, which typically presents with chest pain at rest, not exertion.
*Diastolic aortic pressure*
- **Diastolic aortic pressure** is the main driving force for coronary blood flow; if it is too low, perfusion can suffer.
- While a severely low diastolic pressure would impair perfusion, this patient's blood pressure is normal, and it's less likely the primary factor compared to the reduced time for filling during stress.
Effects of heart rate on cardiac cycle US Medical PG Question 9: A 77-year-old woman with congestive heart failure is admitted to the hospital for evaluation prior to cardiac transplantation. During her stay at the hospital, the physician prescribes a drug to improve cardiac contractility. The drug works by selectively inhibiting an isoenzyme that is responsible for the degradation of cyclic adenosine monophosphate. Which of the following is the most likely adverse effect of this drug?
- A. Hyperkalemia
- B. QT interval prolongation
- C. Hyperglycemia
- D. Bronchospasm
- E. Hypotension (Correct Answer)
Effects of heart rate on cardiac cycle Explanation: ***Hypotension***
- The drug described is likely a **phosphodiesterase-3 inhibitor** (e.g., milrinone), which increases cyclic AMP in cardiac myocytes and vascular smooth muscle cells.
- Increased **cyclic AMP** in vascular smooth muscle leads to **vasodilation**, causing a drop in systemic vascular resistance and subsequently **hypotension**.
*Hyperkalemia*
- **Hyperkalemia** is not a characteristic adverse effect of phosphodiesterase inhibitors. It is associated with drugs like **ACE inhibitors**, **ARBs**, or **aldosterone antagonists**.
- These drugs primarily affect the **renin-angiotensin-aldosterone system** or potassium excretion.
*QT interval prolongation*
- While some **phosphodiesterase inhibitors** can cause **QT prolongation**, it is not the *most likely* adverse effect compared to hypotension, especially in a patient with heart failure.
- Furthermore, **QT prolongation** is a more prominent concern with drugs like **antiarrhythmics** (e.g., amiodarone, sotalol) or certain **antibiotics** (e.g., macrolides).
*Hyperglycemia*
- **Hyperglycemia** is typically associated with drugs that interfere with **insulin secretion** or **insulin sensitivity**, such as **corticosteroids** or some **atypical antipsychotics**.
- Phosphodiesterase inhibitors do not directly cause significant **glucose disturbances**.
*Bronchospasm*
- **Bronchospasm** is a common side effect of **beta-blockers** due to their antagonism of beta-2 adrenergic receptors in the airways.
- Phosphodiesterase inhibitors, by increasing **cyclic AMP**, would theoretically cause **bronchodilation**, not bronchospasm.
Effects of heart rate on cardiac cycle US Medical PG Question 10: A 28-year-old research assistant is brought to the emergency department for severe chemical burns 30 minutes after accidentally spilling hydrochloric acid on himself. The burns cover both hands and forearms. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 20/min, and blood pressure is 108/82 mm Hg. Initial stabilization and resuscitation is begun, including respiratory support, fluid resuscitation, and cardiovascular stabilization. The burned skin is irrigated with saline water to remove the chemical agent. Which of the following is the most appropriate method to verify adequate fluid infusion in this patient?
- A. The Parkland formula
- B. Blood pressure
- C. Pulmonary capillary wedge pressure
- D. Heart rate
- E. Urinary output (Correct Answer)
Effects of heart rate on cardiac cycle Explanation: ***Urinary output***
- Maintaining a specific **urinary output** (e.g., adult with major burns: 0.5-1.0 mL/kg/hr or 30-50 mL/hr) is the most reliable clinical indicator of adequate fluid resuscitation in burn patients.
- This ensures sufficient end-organ perfusion and avoids both under-resuscitation (leading to shock and organ damage) and over-resuscitation (risk of compartment syndrome and pulmonary edema).
*The Parkland formula*
- The **Parkland formula** is used to *calculate* the initial fluid volume needed, but it does not *verify* the adequacy of the infusion once started.
- This formula provides a starting point for fluid administration, which then needs to be adjusted based on the patient's response.
*Blood pressure*
- **Blood pressure** can be misleading in burn patients; it may remain deceptively normal due to compensatory mechanisms even with significant fluid deficits.
- It is a late indicator of hypovolemic shock, and relying solely on it can lead to under-resuscitation.
*Pulmonary capillary wedge pressure*
- **Pulmonary capillary wedge pressure (PCWP)** requires invasive monitoring via a pulmonary artery catheter, which is rarely indicated for routine fluid management in burn patients due to its invasiveness and associated risks.
- Less invasive and equally effective methods, like urinary output, are preferred for monitoring resuscitation.
*Heart rate*
- **Heart rate** is a sensitive but non-specific indicator of fluid status; it can be elevated due to pain, anxiety, or infection, not solely hypovolemia.
- While a decreasing heart rate can indicate improved fluid status, it is not as reliable or direct an indicator of end-organ perfusion as urinary output.
More Effects of heart rate on cardiac cycle US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.